
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Case Report - (2021)
Brain metastasis is the most common intracranial tumors amongst adults. While brain metastasis of Renal Cell Carcinoma (RCC) is less common, intraventricular localization is particularly rare. Here we report a new case of 51- years old patient diagnosed with renal tumor in 2010 and a nephrectomy was performed. He presented with a frontal syndrome consecutive to a left frontal intraventricular lesion. He was operated on for a complete excision of this tumor. Histopathological examinations revealed a metastasis of clear cell renal carcinoma. He underwent 3 radiosurgery sessions. At 6 months of follow-up, he has described an important clinical improvement.
Renal cell carcinoma; Choroid plexus tumor; Brain metastasis; Intraventicular tumor
RCC: Renal Cell Carcinoma; BM: Brain Metastasis; MRI: Magnetic Resonance Imaging; CP: Choroid Plexus.
Brain metastasis (BM) which commonly arises in patients with lung cancer, breast cancer and melanoma are the most common intracranial tumors amongst adults. While brain metastasis of Renal Cell Carcinoma (RCC) is less common, intraventricular localization is particularly rare. There are few small series and mostly case reports which have noted intraventricular involvement of RCC metastasis.
A 51-year-old patient, diagnosed with renal tumor in 2010 and a nephrectomy was performed. He presented confusion, memory loss and concentration disorders during 4 months. Nevertheless, weakness of his right half-body was noted by the patient since two months without any signs of HTIC or comitiality. Clinical examination showed a delirium, memory disturbances and aphasia with a lack of words and dysarthria, without motor deficit. A brain MRI was done showing a left frontal intraventricular tumor with ipsilateral ventricular dilation (Figure 1) The CT-TAP didn’t show suspicious lesions. He was operated on April 2021 for a complete excision of this tumor. Histopathological examinations revealed a metastasis of clear cell renal carcinoma. He underwent 3 radiosurgery sessions one month later. At 6 months of follow-up, he has described an important clinical improvement, mainly of his frontal syndrome (Figure 2).
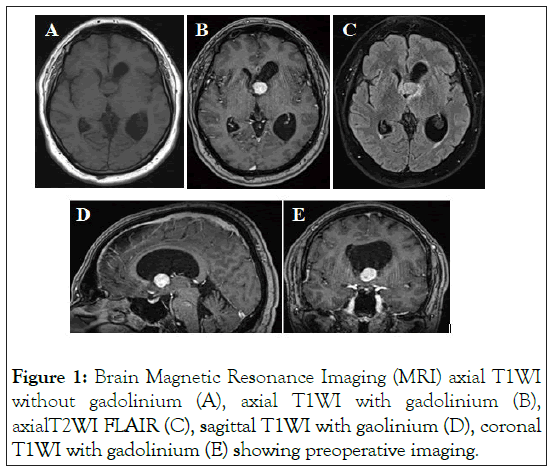
Figure 1: Brain Magnetic Resonance Imaging (MRI) axial T1WI without gadolinium (A), axial T1WI with gadolinium (B), axialT2WI FLAIR (C), sagittal T1WI with gaolinium (D), coronal T1WI with gadolinium (E) showing preoperative imaging.
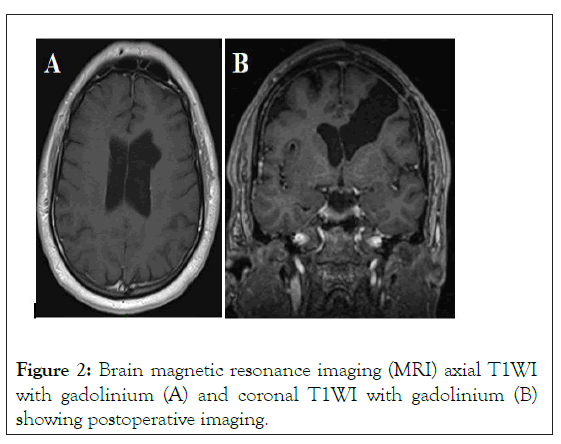
Figure 2: Brain magnetic resonance imaging (MRI) axial T1WI with gadolinium (A) and coronal T1WI with gadolinium (B) showing postoperative imaging.
The most common intraventricular tumor in adults is meningioma, whereas choroid plexus papilloma’s, carcinomas, and ependymomas tend to appear in children and young adults (3% of all intracranial tumors in children and 0.5% in adults) [1,2]. Intraventricular metastasis is rare. Usually the metastasis of the brain is present by multifocal intraparenchymal lesions. It is rare to have only one metastatic lesion at the Choroid Plexus (CP).
Metastases to the CP are mostly reported as series of autopsied patients. Schreiber et al. Study with 737 autopsied cancer patients described only 19 cases (2.6%) of choroid plexus metastasis. Only one of these cases is a single metastasis of the choroid plexus (0.14%) 2. In Japan Brain Tumor Registry, 37 cases (0.9%) of metastases to the lateral ventricle are observed among 3917 cases of brain metastasis.
RCC Metastases to the brain are described in less than 15% of cases, and metastases to the choroid plexus tended to be a relatively late complication of the disease. When the brain metastasis occurs, the prognosis is worst with a median survival of 1-3 months in untreated patients. After brain surgery, a median length survival of 12.6 months has been reported.
A study conducted by [3]. proved that BM secondary to RCC tends to be located adherent to the choroid plexus in the ventricular system. The reason for this association is still unknown.
However, it may be related to chemokine-based homing processes, which play a key role in a wide range of physiological processes during brain development. Another study suggests a relationship between immunohistochemically expression of RCC marker and other papillary carcinomas like papillary choroid carcinoma.
The mean time interval to initial metastasis after nephrectomy is 47 months (range 5-189 months, 132 months in our case). A very slight male versus female predilection was demonstrated with a predilection for the right lateral ventricle. Our case is male but with a left side localization.
On CT scan and MRI scan, CP metastases from RCC show strong homogeneous contrast enhancement with surrounding vasogenic oedema demonstrated that metastatic tumors are frequently found around the foramen of Monro or in the body rather than in the trigone of the lateral ventricle and that is important to make a differential diagnosis from meningioma, which occurs most frequently at this site [4]. An Intra and/or peritumoral flow-voids are also reported that they are relatively characteristic of brain metastasis from RCC. In the present case, the intraventricular mass was, at first, interpreted as a hemangioblastoma because of absence of peritumoral oedema and the vascular character with unhabitual bleeding during surgery.
Intraventricular tumors are in close association with the choroid plexus and are fed by choroidal vessels. Thus, when contemplating a surgical approach, early control on these vessels is important. Although, preoperative embolization of choroid plexus tumors could be a good solution to minimize bloodless and facilitate complete tumor removal.
The indication of radiosurgery is still being discussed. Sheehan et Al. conducted a retrospective review of 69 patients undergoing stereotactic radiosurgery for a total of 146 renal cell cancer metastases [5]. They found that that Stereotactic radiosurgery for treatment of brain metastasis of renal cell carcinoma provides effective local tumor control in approximately 96% of patients and a median length of survival of 15 months. Our patient underwent radiosurgery after surgical complete excision.
BM secondary to RCC tend to be located in the ventricular system with close association to the choroid plexus. Early detection of brain metastases and a therapeutic strategy including surgery and radiosurgery can offer patients an extended survival..
Patient consent
The patient consented to participate and publish their clinical data.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare no conflict of interest.
All authors contributed equally to the manuscript and read and approved the final version of the manuscript.
Citation: Trifa A, Benhadou L, Parker F (2021) Solitary Choroid Plexus Metastasis of Clear Cell Renal Carcinoma 11 years after Nephrectomy: A Case. J Clin Trials. S14:003.
Received: 12-Nov-2021 Accepted: 26-Nov-2021 Published: 03-Dec-2021
Copyright: © 2021 Trifa A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.