Journal of Research and Development
Open Access
ISSN: 2311-3278
ISSN: 2311-3278
Research Article - (2015) Volume 3, Issue 2
The current treatment of lower limb ischemia involves aggressive interventions in order to save the compromised limb and the patient’s life. The risk factors for peripheral arterial occlusive disease are essentially the same as those for atherosclerosis. Ischemic limb has a negative impact on the cardiovascular system and has been associated with increased mortality in patients with arterial occlusive disease. Atherosclerotic lesions with chronic total occlusion in the peripheral arteries are a difficult subset to treat by open or endovascular approaches. Improvements in revascularization techniques have produced more efficient results, in this situation, a minimally invasive endovascular intervention is a more attractive option compared to conventional open procedures, because it is associated with reduced surgical trauma. Now a days we`ve had new endovascular techniques, tactics and surgical materials to contribute to the technical development and improvement of our results for treatment of peripheral arterial disease. Total atherosclerotic arterial occlusions may be a limiting factor for endovascular treatment because of the difficulty in crossing the lesions with conventional guide wires and catheters. Achieving true lumen after subintimal crossing can be challenging and specialized catheters can be used to re-enter the true lumen. In this article, we provide a review of specific devices frontrunner and outback that may increase the procedural success of treating peripheral arterial total occlusions.
<Keywords: Arterial occlusive diseases; Arteriosclerosis obliterans; Intermittent claudication; Endovascular procedures; Angioplasty; Peripheral arterial disease
New endovascular techniques and materials exist to help us with the improvement of our results for the treatment of peripheral arterial disease (PAD). Few decades ago was established the concept of percutaneous transluminal angioplasty (PTA) [1,2].
The challenge to treat those lesions was the passage of the guide wire by total occlusions. It can be intraluminal or subintimal intentional recanalization as described by Bolia [3]. There is no evidence in the literature of superiority of one technique over the other, either in success or recanalization patency [4-6].
Chronic arterial total occlusions (CTOs) with a strong calcium component and extensive lesions (>15 cm) are still today, a factor limiting for endovascular treatment because of the difficulty in transposing these lesions with guide wires and catheters commonly used [7-13]. We can use specialized devices to cross lesions such as Frontrunner - Cordis (Figure 1, 2).
- Cordis (Figure 1, 2).
Achieving the true lumen after subintimal crossing can be challenging and specialized catheters can be used to re-enter the true lumen (Figure 3). In recent years, the reentry devices designed to prevent this series of events has been increasingly used. Not only in patients with critical limb ischemia, but also those with claudication [8-10,13-20].
The ability to treat CTOs was limited by the failure to cross the occlusion and the inability to cross back into the true lumen after crossing the occluded segment. Those special devices during the operation procedure have the accuracy of achieving true lumen reentry easier at the point desired without side-effects as not extending the dissection, occlusion or arterial rupture.
Outback®Cordis reentry system is a device that allows precise and controlled return to the true lumen. The device is an "over the wire" system, guided via a guide wire (0.014") until the desired re-entry point; in the same way as the balloon angioplasty catheter would be guided. During this phase the reentrant cannula highlighted, is retracted (Figure 3). After the device is positioned at the desired re-entry point, the cannula direction is performed to the true lumen through radiopaque markers "L and T" easy viewing, the guide wire is retracted and the cannula is driven through the side of the catheter shaft, allowing the return of the guide wire to the true lumen after occlusion. The tip of the cannula is then retracted and the Outback is removed, leaving free the guide wire to guide the balloon catheter. The Outback system can be used in anterograde and retrograde access, including contralateral access. It is compatible only with the guide wire 0.014" (Table 1 and Figure 4).
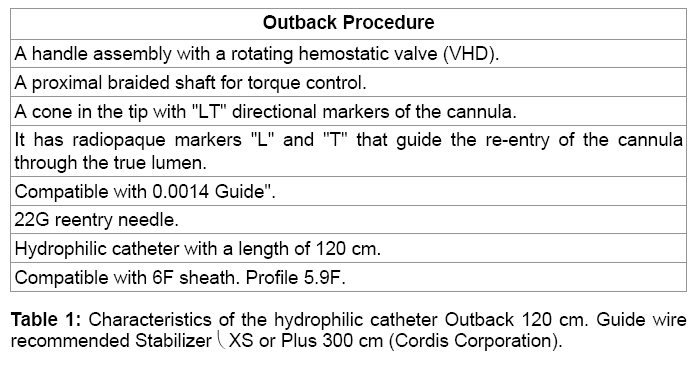
Figure 4: a: Desired reentry. The wire 0.014 guide the Outback directs by subintimal space to the point of desire dreentry. b: Cannula is positioned at the right place the wire is retracted and the can nula ispositioned towards the true lumen. ϖ. c: As advancing the guide wire, it automatically will be directed to the true lumen. d: Following the Outback catheter is removed. e: The guide wire now crossed all the occlusion and the endovascular procedure can be continued.
The reentry catheter has attached a curve needle 22G that enters the vessel lumen when triggered. An “L” marker indicates the direction of needle in an image generated by fluoroscopy (Figure 5a). The tip of the horizontal leg of the "L" should be directed toward the arterial lumen, indicating the way into the vessel. Angling the device in 90graus, orthogonal projection over the first cast, you can view a "T"; the horizontal part of the "T" must be contrasted on the artery (Figure 5b). Right now we know that this cannula directed towards the true lumen, "L" brand, and the device is aligned with the artery "T" mark. Therefore, the fluoroscope will return to its first incidence where there was a "L" mark and the firing of the cannula can be realized because confirm that the Outback is positioned. Upon firing, the wire should be retracted 15cm into the catheter body. After shooting, the guide wire advances in the vessel enabling the continuity of the endovascular procedure (Figure 5c).
Analysis of indications and results
The advantage of subintimal technique is that the plaque is close to the intima and the false lumen created between the intima and media layers are free of endothelium, hindering the formation of atheroma. This can improve the long-term results; since the restenosis is the result of neointimal hyperplasia or atheroma [3,20,21].
The femoropopliteal occlusion is the classic indication for reentry catheter use in patients with intermittent claudication or critical ischemia member [8, 10, 13-20]. There are also reports of successfully use of the device in the aortoiliac and popliteal segments. Importantly, most cases of atherosclerotic occlusions are technically feasible to be realized by the traditional technique of endovascular procedure, but only during the PTA the vascular surgeon has the exact dimension of the technical difficulty of the procedure. In prospective or retrospective studies in patients with claudication or acute ischemia the percentage of patients with occlusions where it was not possible to cross the lesion with a traditional guide wire was 21% ranging between 16.5% and 27% [19-23]. Others report a rate of 10 to 15% [7,24-26]. A study in diabetic population where the primary method of treatment was angioplasty, the technical impossibility to use the traditional endovascular procedure was observed in 25% (144/564) of them [27]. The reentry catheters rate to cross the critical atherosclerotic plaques ranges from 65% to 96%, possible explanations for the different rates of successes includes: surgeon's learning curve, occlusion length, severity of calcification and location of the lesion (aortic, iliac, superficial femoral or popliteal artery) [13-18, 28-31].
Treatment of chronic total occlusions can be challenging, and high failure rates are not unusual. Sometimes intraluminal passage is impossible, and the sub-intimal technique is the option. Recanalization failure in this situation is commonly due to the inability to re-enter distal to the occlusion. Commercially available re-entry devices, such as Outback catheters, were designed to overcome this situation. Early reports have shown a very high technical success rate. Described complications related to the use of the devices are: failure of the procedure, arterial bleeding or perforation with contrast extravasation. Most of them does not compromise or aggravates the patient's condition. In 2 patients, a series of 118 (1.7%) cases, the retractable needle could not be removed with the catheter. In both cases the system was removed without damaging the artery. Bleeding due to the use of the device in the target vessel occurred in 5/118 (4.2%) cases. Four of then were successfully completed. The fifth patient had his intervention stopped and the bleeding controlled by manual compression. It was not necessary surgical conversion.13
Technical success provided by the re-entry catheter has allowed the advance in endovascular approach to treat peripheral arterial disease, in addition to the increase in technical success also in complex cases of arterial occlusions added precision to the intervention. Help us to limit the distal dissection and not pass away the "end point", thus not increasing the dissection, avoiding complications and assist in preserve the collateral vessels. New tactics, techniques and surgical approaches arises to solve cases where failed percutaneous revascularization attempts have been recovered with the re-entry catheter. Its implementation has been more extensive and highlights the fact that the re-entry devices have become essential tools in the treatment of atherosclerotic occlusions of the complex peripheral arteries and should be available for all these cases.