Autism-Open Access
Open Access
ISSN: 2165-7890
ISSN: 2165-7890
Research Article - (2024)Volume 14, Issue 2
Background: As adequate training of healthcare professionals is one of the most critical contributors to the successful Health Care Transition (HCT) of Young Adults with Autism (YAWA), it is crucial to examine the perceptions of key stakeholders involved with the transition process.
Objective: This study explores the perspectives of parents/caregivers of YAWAs, clinicians and allied health professionals regarding the salient needs of YAWAs during HCT.
Materials and methods: Data are from 151 respondents, comprising 50 caregivers, 43 clinicians and 48 allied health professionals (Social Workers (SWs), Physical Therapists (PTs) and Occupational Therapists (OTs)). Respondents completed an online survey regarding their experiences caring for YAWAs and the specific needs that arise during HCT.
Results: Over half of parents/caregivers reported that their YAWA did not receive any transition services. Other transition-related challenges that parents/caregivers reported were providers’ in experience with YAWAs and their YAWA’s difficulty transitioning outside the medical environment. Clinicians with 10+ years of experience reported the highest comfort levels working with YAWAs. Clinicians cited employment and independent living as the top challenges for YAWAs. Among allied health professionals, comfort levels were significantly associated with frequency of interaction with YAWAs. SWs indicated that YAWAs’ salient needs during transition to adulthood include housing/independent living skills and productive involvement (e.g., employment, volunteering). PTs and OTs reported experiencing difficulties with communication, engagement and compliance when providing care for YAWAs.
Conclusion: Findings indicate that families of YAWAs, clinicians and allied health professionals would benefit from evidence-based guidance in the HCT process that incorporates existing literature and interdisciplinary perspectives.
Young adults with autism; Health care transition; Transition to adulthood; Health professionals; Caregivers of individuals with autism
Individuals with Autism (IWAs) face significant challenges in accessing appropriate preventative and specialty healthcare services [1-3]. Parents of children with autism are more likely than parents of children with other disabilities to experience unmet healthcare needs and difficulty finding providers with sufficient skills or training to provide specialty services [4]. IWAs also often experience dissatisfaction with their healthcare services, but find it difficult to articulate these feelings as well as their other personal and sensory needs to providers [5-8]. Such barriers to securing adequate and tailored healthcare services contribute to the healthcare inequities IWAs experience, which, in turn, have long-lasting implications for their health and well-being.
The transition to adulthood, inherently a complex and stressful process for most, may exacerbate these underlying challenges for IWAs, emphasizing the critical role of Health Care Transition (HCT) processes for these populations. The Society for Adolescent Medicine (SAM) defines HCT as a multi-faceted, active process that attends to the medical, psychological, social and education/ vocational needs of adolescents as they move from the child-focused to the adult-focused health care system [9]. HCT provides individuals with disabilities the opportunity to increase independence as they engage with adult healthcare systems, thereby empowering them to make healthier decisions and achieve better health outcomes over the life course. Direct implications of effective HCT are improved self-advocacy skills and increased knowledge regarding one’s condition and its associated challenges [10]. With appropriate HCT processes and planning in place, IWAs can better manage their healthcare, communicate with providers and obtain services that meet their specific needs. Despite its importance, the implementation of effective HCT has been infrequent, with little improvement in the past two decades [11,12]. Once Young Adults with Autism (YAWAs) leave pediatric practices, access to adult healthcare and deficiency in adult provider knowledge about support systems are major barriers [13]. For example, Bultas, et al., [14] found that healthcare practitioners have reported challenges communicating with, examining and alleviating fears of patients with autism.
As adequate training of healthcare professionals is one of the most critical contributors to the successful HCT transition of IWAs, it is crucial to examine the needs and perceptions of key stakeholders involved with the transition process. This study explores the perspectives of various stakeholders, including parents/caregivers of YAWAs, clinicians and allied health professionals, regarding the salient needs of YAWAs during HCT. This study’s findings will inform interventions specifically tailored for healthcare providers who work with YAWAs during HCT, thereby optimizing healthcare experiences during this critical junction in the life course.
Sample and procedures
Data are from 151 respondents, comprising 50 parents/caregivers of YAWAs, 43 internal medicine or family medicine clinicians and 48 allied health professionals (i.e., 16 Social Workers (SWs), 16 Physical Therapists (PTs) and 16 Occupational Therapists (OTs)). Respondents completed an online survey between May-July 2023 regarding their experiences caring for YAWAs and YAWAs’ specific needs during the transition to adulthood. Participants were recruited through healthcare networks in the region. This study was approved by the Lehigh University Institutional Review Board (IRB).
Measures
The research team utilized validated survey items from Derret, et al., [15] Provider and Staff Perceptions of Integrated Care (PSPIC) survey and Ames, et al., [16] Provider Survey for Transitioning Youth with Autism (PSTYA) and other special health care needs into adult primary care. Surveys were pretested by individuals within each stakeholder group and modified based on feedback before seeking IRB approval.
Analytical approach
Descriptive statistics, including frequencies, percentages, means and standard deviations, were calculated to illustrate the sample’s characteristics and other quantitative findings. Kruskal-Wallis tests were conducted to compare clinicians’ responses by years of experience and allied health professionals’ experiences by educational and work-related characteristics. For open-ended survey responses, one cycle of deductive coding was conducted to identify salient themes.
Parents/caregivers
Quantitative findings: The mean age of the YAWAs discussed in parent/caregiver responses was 22.58 (SD=3.63). Over half (56%) of the respondents indicated that their YAWA did not receive any medical transition services as shown in Figure 1A. Prevalent types of transition services received included help with teaching their YAWA how to manage their own health needs (20%), support in searching for an adult primary care physician (18%), discussions about how healthcare needs may change in adulthood (16%), discussions about how to manage the transition to the adult healthcare system (16%) and information about adult medical specialists (16%).
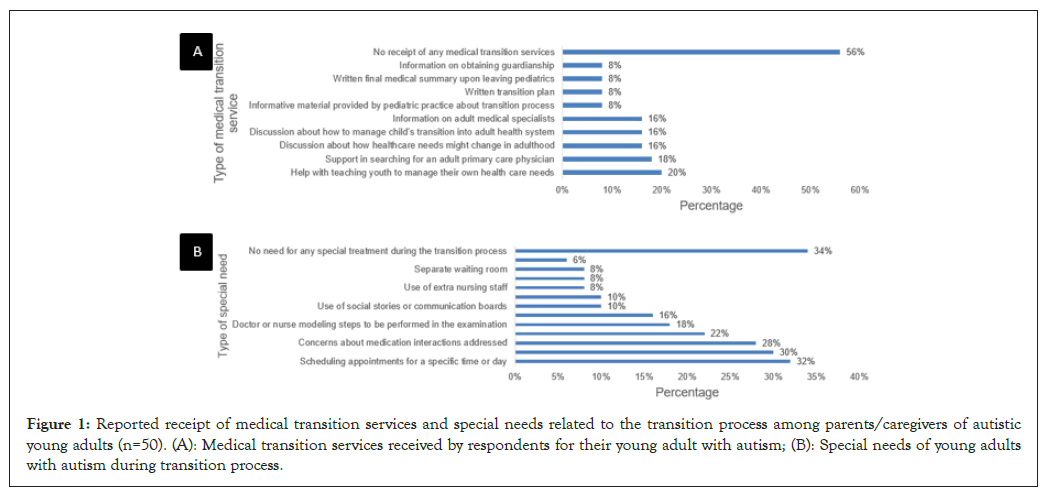
Figure 1: Reported receipt of medical transition services and special needs related to the transition process among parents/caregivers of autistic young adults (n=50). (A): Medical transition services received by respondents for their young adult with autism; (B): Special needs of young adults with autism during transition process.
When asked about challenges parents/caregivers experienced due to caring for their YAWA, 74% reported that they had concerns regarding their YAWA’s future care needs. Prevalent transition needs that were reported for YAWAs included were scheduling appointments for a specific time or day (32%), assistance with scheduling specialist appointments for additional healthcare needs (30%) and concerns about medication interactions (28%); 34% of respondents stated that their YAWA had no unique needs during the transition process as shown in Figure 1B (Figures 1A and 1B).
Qualitative findings: In the open-ended portion of the survey, 12% of parents/caregivers reported that they were not given help or support in the transition process. Some noted providers’ inexperience with the population (6%) and difficulty with non-medical transition processes (e.g., job skills, financial literacy (6%)). Only 10% of respondents noted that their young adult was comfortable with their new provider. Further, 10% of respondents reported that their child had little or no independence skills.
Clinicians
Quantitative findings: Most clinicians (72%) reported having at least 6 years of experience with IWAs who transitioned from pediatric to adult medicine. When asked how comfortable, on a scale of 0-4 (with higher scores reflecting greater comfort), they were in providing care to new YAWA patients, clinicians’ average score was 2.13 (SD=0.98). Their average comfort level with addressing the needs of YAWAs who identify as LGBTQ+ was 1.85 (SD=1.16) on a scale of 0-4, with 15% stating as not at all comfortable and 10% stating as extremely comfortable. When asked how well their medical training prepared them to care for IWAs, clinicians scored an average of 1.54 (SD=1.02) on a scale of 0-4 (0=not well at all; 4=extremely comfortable), with 15% reporting as not well at all and 0% reporting as extremely well. Further, clinicians with 10+ years of experience reported the highest comfort level working with new YAWA patients during HCT (p=0.03).
When asked to rate their interest, on a scale of 0-4 (with higher scores reflecting greater interest), in attending educational sessions regarding working with YAWAs, clinicians scored an average of 2.81 (SD=1.05), with 33% reporting that they are extremely interested and none reporting as no interest at all. Most clinicians indicated a preference for the delivery of educational sessions to have an online component (Zoom, online asynchronous, hybrid). When asked how important it is for the patients, parents and group home (i.e., Community Living Arrangement (CLA)) staff to be involved in sessions, clinicians scored an average of 3.05 (SD=0.92) on a scale of 0-4 (0=not important at all; 4=extremely important), with 42% indicating extremely important and none stating not important at all (Table 1).
| Years of experience seeing patients with autism | Comfort level with providing care to new patients with autism during transition from pediatric care | Comfort level with addressing needs of young adults with autism who identify as LGBTQ+ | Level of preparation during medical training for caring for patients with disabilities | Level of interest in attending information sessions | Degree of importance for patients, parents and group home staff to be involved in information sessions | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Range: 0-4 Mean (SD) |
P-value | Range: 0-4 Mean (SD) |
P-value | Range: 0-4 Mean (SD) |
P-value | Range: 0-4 Mean (SD) |
P-value | Range: 0-4 Mean (SD) |
P-value | |
| Total | 2.13 (0.98) | 0.03 | 1.85 (1.16) | 0.17 | 1.54 (1.02) | 0.28 | 2.81 (1.05) | 0.13 | 3.05 (0.92) | 0.77 |
| 0 years (n=4) | N/A | - | N/A | - | N/A | - | 2.00 (0.82) | - | 2.25 (0.50) | - |
| Less than 1 year (n=1) | 1.00 | - | 1.00 | - | 0.00 | - | 3.00 | - | 4.00 | - |
| 1-5 years (n=10) | 2.20 (1.03) | - | 1.70 (0.67) | - | 1.90 (0.99) | - | 3.50 (0.71) | - | 3.00 (1.05) | - |
| 6-10 years (n=11) | 1.55 (0.52) | - | 1.36 (1.12) | - | 1.45 (0.93) | - | 2.91 (1.22) | - | 3.18 (0.87) | - |
| More than 10 years (n=17) | 2.53 (1.01) | - | 2.29 (1.31) | - | 1.47 (1.07) | - | 2.53 (1.01) | - | 3.12 (0.93) | - |
Note: LGBTQ+: Lesbian, Gay, Bisexual, Transgender, Queer and other sexual orientation and gender identities; SD: Standard Deviation.
Table 1: Clinicians’ responses by years of experience (n=43).
Qualitative findings: Most clinicians (72%) who worked with transition-age IWAs stated that they were unaware of community resources that support IWAs or individuals with disabilities in general and 74% reported that no training was provided that better prepared them to work with IWAs. Clinicians reported that the most prevalent challenges facing IWAs during transition are issues with employment (72%) and independent living arrangements (59%). Many clinicians (56%) reported that having heightened knowledge of resources (e.g., lists, hubs) would be most helpful in better preparing them to work with YAWAs.
When asked what types of support systems would help providers facilitate a seamless HCT for IWAs, some clinicians (23%) recommended access to social workers, counselors and other mental health personnel and 21% noted that a more systematic process of transitioning services should be in place, such as scheduling transition visits to promote familiarity with the office prior to appointments. Lastly, when asked what types of support systems would help patients and families experience a more effective HCT, the most common responses were access to mental health services (35%) and resources/case managers (28%).
Allied health professionals
Quantitative findings: Allied health professionals, comprising SWs, PTs and OTs, reported an average of 13.95 (SD=9.70) years of experience working in their current profession, with a range of 1-26 years. Most respondents had a master’s degree (67%) and worked in outpatient settings (94%). SWs, PTs and OTs each received specific questions regarding their experiences. When asked how comfortable they felt working with IWAs, there were no significant differences in this response by type of profession. When comparing comfort level by educational and work-related characteristics, there were significant differences by frequency of work with YAWAs (p=0.03) and by frequency of interaction with individuals with disabilities other than autism (p=0.03), such that respondents who had more frequency of contact generally reported higher mean comfort scores. Respondents who had more frequent work with YAWAs reported statistically significantly higher mean confidence in providing or referring to resources for YAWAs (p=0.03).
Qualitative findings: The most common needs SWs reported seeing for YAWAs during the transition to adulthood included housing/independent living skills (63%) and enhancing productive involvement, such as through the workforce or volunteering (63%). SWs were asked what healthcare providers could do to better assist YAWAs and the most prevalent response was having knowledge about and providing resources (38%). SWs noted that conferences (44%), webinars (38%) and grand rounds (31%) would increase their comfort level in providing care to this population. Further, the most common challenge PTs reported experiencing when providing care to IWAs was difficulties with communication and engagement (50%). PTs noted that webinars (31%), readings or online courses (19%) and professional development and collaboration opportunities (19%) would increase their comfort in providing care for YAWAs. When asked the specific challenges in providing care to YAWAs, common responses from OTs were compliance with Home Exercise Program (HEP) (25%), communicating with and understanding patients (19%) and follow-through or caregiver burnout (19%). OTs reported that webinars (38%), conferences (25%) and continuing education opportunities (25%) would increase their comfort level in providing care for YAWAs (Table 2).
| Question | Themes | N (%) | Quotes |
|---|---|---|---|
| Parents/caregivers | |||
| If desired, please describe any challenges or successes you or your young adult with autism have experienced when transitioning to an adult healthcare provider? Response rate: 27/50 (54%) |
No help/transition support | 6 (12%) | We had no help. I chose her doctors and scheduled her appointments; I understand the transition isn't one that has to happen right at 18 years old but there should be more support for finding an appropriate doctor that we feel comfortable with; Our pediatrician did not help or discuss transitioning to adult care, so we are on our own. I don't even know where to go and have little time to investigate what to do; There is a real lack of assistance/support for autistic persons after adulthood. This is a real gap. Help. |
| Comfortable with provider | 5 (10%) | [Doctor’s name] provided a relaxed environment and he was comfortable with her. He actually likes going to see [Doctor’s name]; The doctors and staff have been very patient in dealing with my autistic child. They took the time to answer their questions and explain what was going on. [Doctor’s name] has been especially kind in dealing with my child, she explains things, talks to her and is very positive which I appreciate very much; Our adult primary care physician listened to my son's history and reviewed notes from not only my son’s pediatrician but also his developmental pediatrician outside [hospital name]. My son's adult physician was and is willing to write letters needed to get my son benefits from the state and federal governments. | |
| Doctors’ inexperience with specified population | 3 (6%) | Her doctors don't seem knowledgeable about adults with special needs; Lack of services to address specific needs of young adults with disabilities such as sexuality, health and mental health issues. | |
| Difficulty transitioning outside of medical environment | 3 (6%) | We had much more difficulty transitioning to adulthood/job skills/planning for his future needs; She is high functioning and struggles everyday but is adapting some survival skills to suit her, but still needs a daily phone call reminder on basic decisions. E.g., job skills, planning for future, financial. | |
| If desired, please describe any challenges or successes you or your young adult with autism have experienced when during the transition from pediatric to adult healthcare or while achieving independence in healthcare related decisions? Response rate: 14/50 (28%) |
Little or no independence | 5 (10%) | I wouldn't say he has achieved independence as we still book appointments and transport him to them; We still have the challenge of helping my child gain independence in making healthcare and life choices. They believe everything they're told by authority figures which include doctors and nurses. In one way it's good that they will follow doctor's orders, but they won't question things that may not be the best course for them. It's hard to teach judgement. |
| Doctors knowledge of history/easy transition | 4 (8%) | I was quite impressed with how little we actually had to explain. The staff seemed to have a good grasp of [child’s] needs after the 1st visit; He completed the visit by himself based on the notes, I gave him. | |
| Clinicians | |||
| Please list some community resources you know that support patients with autism or disabilities in general. Please state none if you are not aware of any such resources Response rate: 38/39 (97%) |
None/unknown/no response | 28 (72%) | - |
| Autism society (region removed) | 4 (10%) | - | |
| None | 29 (74%) | - | |
| What additional training, if any, have you received that has better prepared you to work with individuals with autism who are transitioning into adulthood? Response rate: 37/39 (95%) |
Personal/hands-on experience | 5 (13%) | Experience with patients helps treat others in the future. |
| In your experience, what specific challenges do autistic youth and their families face as they transition into adulthood (e.g. issues with employment, education, recreation, sexuality or dating, independent living, etc.) Response rate: 37/39 (95%) |
Employment | 28 (72%) | - |
| Independent living/living arrangements | 23 (59%) | Care for individual as their caregivers become more debilitated. | |
| Sexuality/dating | 10 (26%) | - | |
| Recreation | 10 (26%) | - | |
| Caregiver/family dynamics | 8 (21%) | Evaluation of patient competence to make medical decisions: Should this be deferred to caregiver or does the person with autism have the ability to make their own decisions? This line gets blurry and is hard to fully allow for patient autonomy when caregivers are sometimes overbearing. | |
| Education | 8 (21%) | - | |
| Interpersonal dynamics | 8 (21%) | Social integration. | |
| Obtaining services | 6 (15%) | Problems with services. | |
| What types of information would be most helpful to better prepare you to work with individuals with autism who are transitioning into adulthood? Response rate: 41/43 (95%) |
List of resources/community resources | 24 (56%) | List to give to patients/families |
| Improving communication and understanding of patients’ needs | 6 (14%) | Information for how I can better interact with this group of patients and any specific needs that are common; Guide on interacting with individuals with autism including their top concerns that they would like addressed at a visit. | |
| What types of support systems do you feel should be in place for providers to allow for a seamless transition to adulthood for your patients with autism? Response rate: 42/43 (98%) |
Social workers/counselors | 10 (23%) | More access to counselors/therapists. |
| Systemic process of transitioning services | 9 (21%) | Transition of care document listing services currently in place; time to allow for transition visit. | |
| Behavioural health support | 7 (16%) | Referral process to a case worker who can help connect with resources; Clinical coordinator for support staff. | |
| Case manager/list of resources | 7 (16%) | - | |
| Nurse care manager | 6 (14%) | - | |
| What types of support systems do you feel should be in place for patients and their families to allow for a seamless transition to adulthood for your patients with autism? Response rate: 42/43 (98%) |
Access to mental health services | 15 (35%) | Social workers and behavioural health therapists with experience. |
| Resources/case manager | 12 (28%) | They should know what the community and [healthcare network name] support systems. | |
| Allied health professionals | |||
| Social workers | |||
| As a social service provider, please list the three most common needs that you see for young adults with autism as they transition into adulthood. Response rate: 15/16 (94%) |
Housing/independence life skills | 10 (63%) | - |
| Productive involvement | 10 (63%) | Support for transitioning into the workforce or volunteering; continuing education; financial literacy support. | |
| Social life | 6 (38%) | Peer connections; community involvement/socializing. | |
| Support services for activities | 6 (38%) | - | |
| Counseling/psychiatry | 3 (19%) | - | |
| Transportation | 3 (19%) | - | |
| What could healthcare providers (i.e., physicians, nurse practitioners, physician assistants) do to better assist young adults with autism and their family members? Response rate: 15/16 (94%) |
Knowledge about/provide resources | 6 (38%) | Educating them to get connected to County resources prior to their 21st birthday. |
| Making referrals | 2 (13%) | - | |
| Improving communication with patients | 2 (13%) | Be clear and direct in communicating with them regarding treatment needs; Teach information differently. | |
| Improving understanding of autism | 2 (13%) | Continue to develop their understanding of autism and how it manifests in medical settings; Education/training specific to autism. | |
| Connect to autism case manager | 2 (13%) | - | |
| What types of training and resources would increase your comfort level in providing care for young adults with autism? Response rate: 15/16 (94%) |
Conferences | 7 (44%) | Conferences that provide scenarios-based trainings. |
| Webinars | 6 (38%) | - | |
| Grand rounds | 5 (31%) | - | |
| Physical therapists | |||
| What are some of the specific challenges that you see when providing care to young adults with autism (e.g., communication, compliance/adherence to care instructions, home versus on-sight physical therapy, etc.)? Response rate: 14/16 (88%) |
Communication/engagement | 8 (50%) | Engaging the patient in a meaningful way to them; Keeping their focus; Communication/providing directions at times. |
| Gaining buy-in and follow through with families | 3 (19%) | Ability to get them to buy in the limited time we are given; Follow through at home. | |
| Compliance with Home Exercise Program (HEP) | 3 (19%) | - | |
| Maintaining continuity of care | 3 (19%) | Families tend to want continuous therapy instead of breaking it up into episodes of care. | |
| What types of training and resources would increase your comfort level in providing care for young adults with autism? Response rate: 13/16 (81%) |
Webinars | 5 (31%) | - |
| Readings/online courses | 3 (19%) | - | |
| Professional development and collaboration opportunities | 3 (19%) | Education/collaboration days to learn about additional resources and others in the Network to refer to; Communication with an experienced clinician for a case-by case basis. | |
| Lists of community services | 2 (13%) | - | |
| Podcasts | 2 (13%) | - | |
| Grand rounds | 2 (13%) | - | |
| In your profession, what are the most common reasons that young adults with autism are referred for services? Response rate: 15/16 (94%) |
Pain/injuries | 12 (75%) | E.g., Concussion, orthopedic injuries, pain, musculoskeletal dysfunction. |
| Strengthening and conditioning | 3 (19%) | E.g., Core strengthening, decrease in activity due to COVID-19. | |
| Neurological issues | 2 (13%) | - | |
| Occupational therapists | |||
| If you have a patient in need of additional resources/supports, what steps do you take to assist this patient? Response rate: 14/16 (88%) |
Outreach | 9 (56%) | - |
| Research | 6 (38%) | - | |
| Direct patients to websites | 4 (25%) | - | |
| Help with job skills and searches | 3 (19%) | - | |
| What are some of the specific challenges that you see when providing care to young adults with autism (e.g., communication, compliance/adherence to care instructions, home versus on-sight therapy, etc.)? Response rate: 12/16 (75%) |
None/no response | 5 (31%) | - |
| Compliance with HEP | 4 (25%) | - | |
| Communicating with and understanding patients | 3 (19%) | - | |
| Follow-through/caregiver burnout | 3 (19%) | Caregiver burn out/resistant to change or my suggestions. | |
| Finding funding/resources | 2 (13%) | Finding funding/resources for their needs. | |
| Difficulty gaining home services | 2 (13%) | Typically home based services are only for medically frail or older adults. | |
| What types of training and resources would increase your comfort level in providing care for young adults with autism? Response rate: 14/16 (88%) |
Webinars | 6 (38%) | - |
| Conferences | 4 (25%) | Conferences specific to the community I work. I have been to general conferences/learning opportunities but it's different when it's not in the community you work. | |
| Continuing education opportunities | 4 (25%) | Currently in certification for becoming a certified autism specialist; Continuing education opportunities. | |
| Podcasts | 3 (19%) | - | |
| Any type | 2 (13%) | - | |
| In your profession, what are the most common reasons that young adults with autism are referred for services? Response rate: 14/16 (88%) |
Activities of Daily Living (ADL) skills | 3 (19%) | Delayed ADL/ Instrumental Activities of Daily Living (IADL) skills. |
| Orthopedics | 3 (19%) | E.g., Fine motor, coordination difficulties, handwriting, concussion; pain management. | |
| Vocational training | 3 (19%) | Job prep; We need to support individuals as they age and transition to work and leisure roles. | |
| Self-care tasks | 2 (13%) | Self-care deficits. | |
| Sensory processing | 2 (13%) | - | |
| Communication/social skills | 2 (13%) | To improve functional communication. | |
Table 2: Thematic analysis of open-ended responses from clinicians, parents/caregivers and allied health professionals.
The study’s findings provide important insights about the critical stage of HCT for IWAs from the perspectives of key stakeholders, including parents/caregivers, clinicians and allied health professionals. Over half of parents/caregivers reported that their young adult did not receive any transition services. Other transition-related challenges that parents/caregivers reported were providers’ inexperience with IWAs and their YAWA’s difficulty transitioning outside the medical environment. Clinicians with 10+ years of experience reported the highest comfort levels working with YAWAs. Additionally, clinicians cited employment and independent living as the top challenges for YAWAs. The majority of clinicians also indicated that they did not receive training that better prepared them to work with YAWAs and were unaware of community resources that support IWAs. Among allied health professionals, comfort levels were significantly associated with the frequency of their interactions with IWAs. The top needs SWs indicated were housing/independent living skills and enhancing productive involvement (e.g., employment, volunteering). PTs and OTs indicated that the most significant challenges they faced were difficulties with communication, engagement and compliance.
These findings corroborate with the existing literature, which has widely shown that IWAs continue to experience significant barriers in accessing needed services. These barriers are exacerbated when transitioning into adult healthcare, as IWAs are not only required to find a new provider during a time when they face challenging environmental changes, but also receive little guidance during the transition process. Qualitative survey findings further expanded on these challenges, as parents/caregivers reported obstacles such as providers’ inexperience, the need for improved communication and the desire for transition support outside of the medical environment.
Despite the increasing prevalence of autism diagnoses, clinicians and allied health professionals in this sample reported inadequate training and lack of comfort in treating IWAs [17]. Consistent with our findings, the literature indicates that medical trainees who have experienced more training and exposure to young adults with disabilities report higher confidence and comfort working with them [18]. Most clinician and allied health professional respondents also desired further training and knowledge of resources tailored to IWAs, with many noting the importance of embedding the voices of IWAs into the trainings. Overall, our findings indicate that families of IWAs, clinicians and allied health professionals would benefit from evidence-based guidance in the HCT process, thereby emphasizing the need for a training toolkit that incorporates existing literature and interdisciplinary perspectives.
Limitations
Some potential limitations should be considered when interpreting the findings. First, as our study was cross-sectional, we cannot attribute causality between potential independent variables (e.g., years of experience) and outcomes (e.g., comfort level caring for IWAs). However, our study is primarily descriptive and only aims to compare responses by key sociodemographic and work-related characteristics. Second, the sample sizes for each stakeholder group were small and may not represent the sociodemographic and work-related characteristics of these groups; nevertheless, the scope of this study is descriptive and is intended to provide a broad and preliminary snapshot of personal and health professional perspectives regarding the salient needs of IWAs during HCT. Third, due to recruitment challenges, we did not administer surveys among IWAs to directly ascertain their experiences; however, future qualitative research will be conducted to explore the lived experiences of this population as well as parents/caregivers.
Implications
This study’s findings shed important insights into the unique challenges faced by YAWAs during HCT. This multi-stakeholder exploration indicates that families are often not prepared for this process and struggle in finding adult healthcare clinicians who are experienced and comfortable in caring for YAWAs. Our findings strongly suggest that clinicians would benefit from specifically tailored trainings and increased exposure to IWAs. After gaining knowledge of available community resources through these trainings, they will be better equipped to help families connect with these resources. Similarly, allied health professionals, such as SWs, PTs and OTs, would also benefit from increased exposure to IWAs and training comprising effective communication strategies and local resources that can be shared with patients and families [19].
Importantly, the findings of this study will be used to create trainings similar to the Patients with Disabilities as Teachers (P-DAT) program and will address the needs expressed by key stakeholders. Based on this study’s findings, topics to cover include patient-centered communication techniques; Information on local, regional and national resources and discussion of the importance of patients obtaining information about housing (independent living if possible), sexuality, recreation and employment. This training will enable healthcare professionals to become more comfortable with and welcoming to IWAs who are transitioning from pediatric care. Based on our findings, we posit that increased interaction between providers and IWAs will yield greater comfort during these interactions. Finally, as our study indicates that most areas that need addressing are similar among the clinicians and allied health professionals, a common training curriculum can be created and implemented with minor modifications for each professional group.
Funding for this study was provided by the Accelerator grant from Lehigh University's Office of the Vice Provost for Research. We thank the Medical Home Project, Grace Murphy and Mariangela Perrella for their assistance and support with this study. We also thank the study participants for taking the time to provide their valuable insights for our study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
Citation: Wakeel F, Jain S, Connors V, Blasko A, Berman J, Morin K (2024) Stakeholder Perspectives on Needs of Young Adults with Autism in Health Care Transition. Autism-Open Access. 14:398.
Received: 31-May-2024, Manuscript No. AUO-24-31970; Editor assigned: 03-Jun-2024, Pre QC No. AUO-24-31970 (PQ); Reviewed: 17-Jun-2024, QC No. AUO-24-31970; Revised: 24-Jun-2024, Manuscript No. AUO-24-31970 (R); Published: 02-Jul-2024 , DOI: 10.35248/2165-7890.24.14.398
Copyright: © 2024 Wakeel F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.