Review Article - (2018)Volume 1, Issue 1
Thrombospondins (TSP) are a group of multifunctional secretion proteins that consist of TSP-1 to TSP-5. TSP-1 is the first protein member of this family and a homotrimeric glycoprotein with a multifunctional domain. The aim of this study is to evaluate the level of TSP-1 and its impact on vessels in diabetic patients.
In 2016, 90 diabetic patients were selected from Golestan hospital and Emam Khomeini hospital, they were put into three different groups; 30 patients (FBS over 126 mg/dL) without a diabetic foot ulcer (DFU) (group 1), 30 diabetic patients (FBS over 126 mg/dL) with a DFU (group 2), 30 people without diabetes or DFU (group 3). In all patients, Hemoglobin A1c (HbA1c), blood sugar, and TSP-1 tests were performed.
Results: The mean amount of TSP-1 in group 1, 2, and 3 was 266.85 ± 88.75 ng/mL, 234.87 ± 129.8 ng/mL, and 1570.42 ± 1047.42 ng/mL, respectively. The average level of HbA1c in group 1 was 8%, in group 2 it was 10%, and in the normal group it was 5%. The results of the statistical tests indicated that there is a significant difference in TSP-1 level between the diabetic group without DFU and the diabetic group with DFU (p value=0.01).
Conclusion: Lack of TSP-1 expression is accompanied by VEGF high expression and reduction of TGF-Æ. Lack of TGF-Æ can cause immunological diseases, inflammation, growth diseases, wound healing reduction, and an increase in occurrence of tumors. High expression of VEGF leads to excessive proliferation of vessel endothelial cells. The result of the study indicated that TSP-1 has a significant role in inhibition of angiogenesis. As blood sugar and HbA1c levels increase, TSP-1 levels decrease, which causes foot ulcers due to vessel complications? However, these complications can be avoided by controlling diabetes.
One of the most important sources for producing energy in the body is glucose, it is used in most processes such as movement, brain function, and growth. With such an important role there are processes to help control glucose levels in the body. Insulin, produced from pancreas cells, is a key molecule that promotes glucose metabolism from blood to liver, fat, and muscle tissue. Diabetes is a disease in which the level of blood glucose is high, due to a disorder in insulin function. There are many types of diabetes the three most common types are: diabetes type 1, diabetes type 2 (insulin dependent), and gestational diabetes.
Type 1 diabetes
Type 1 diabetes is caused by a reduced or complete absence of insulin in the body, these patients are treated with insulin shots and other drugs to help the control of glucose levels. This type of diabetes accounts for 10% of all patients and it occurs mainly in childhood or before the age of 30 [1].
Type 2 diabetes
Diabetes type 2 makes up most of the other 90% of diabetic patients [2] and begins to manifest after middle age; however, in several countries such as Iran, the age of onset has decreased in recent years. Thirst, excessive hunger, polyuria, and high fasting blood sugar (FBS) (about 200 mg/L) are signs of diabetes type 2.
Gestational diabetes
Gestational diabetes is a temporary circumstance that occurs in about 2-4% of all pregnancies. Pregnancies over 35 years old and a high fetus weight are dominant factors for being afflicted with pregnancy diabetes. Over a prolonged time, diabetes can lead to several complications including amputation of limbs, heart and renal dysfunction, as well as optical and neurologic problems [3].
Prevalence of diabetes type 1 and 2 are increasing worldwide but in countries across North Africa and the Middle East these numbers are predicted to increase significantly more until the year 2030 [4]. According to the Diabetes International Federation, the prevalence of diabetes in North Africa and the Middle East will have the highest increase compared to all other regions of the world [5]. According to a study in France, over 0.5 million children, from ages 0-14 are afflicted with diabetes type 1 [6]. One of the important diabetic complications that can occur is the diabetic foot ulcer (DFU), which is caused by wound healing problems, it occurs in about 25% of patients. The severity of a DFU can be seen when we see that about 80% of foot ulcers are accompanied by lower leg amputation [7]. The DFU have several complications that can involve several mechanisms, such as neuropathy, increased biomechanical stress, peripheral arterial disease, deformity, and trauma [8]. This is not to mention that another serious risk is that these ulcers are often complicated by infection [9].
The diabetes disease is a heavy burden on society, with high costs to the patients as well as to the healthcare system [10]. As with all diseases an increase in awareness and regular checkups can help prevent many health risks [11], but other medical advancements for the afflicted are also necessary. In 1971, Folkman published a paper in the New England Journal of Medicine, which proposed the theory of angiogenesis, his study indicated that tumors do not grow more than a certain size unless their vessels increase. In his theory he described how tumors create new vessels by using angiogenesis factors, which he described, at the time, as a tumor angiogenesis factor. He explained that if we can inhibit angiogenesis, the tumors would remain small and in effect be less dangerous [12]. What Folkman was describing was thrombospondin-1 (TSP-1).
Thrombospondin-1 (TSP-1) is an adhesive glycoprotein that plays many roles including inhibition of angiogenesis, survival of endothelial cells, and lack of this protein causes hyper activity of angiogenesis [13]. TSP-1 is produced by alpha granules of platelets, which also contain fibrinogen and fibronectin which are effective in homeostasis and wound healing [14].
This study assessed the level of TSP-1 in DFU patients in comparison to diabetic patients without a foot ulcer. With the result of this study and many others we aim to find an appropriate solution for prevention of this complication, as well as improving the quality of patient care and understanding the effect of TSP-1 on DFU’s.
Inclusion criteria
In 2016, 90 patients were chosen for the study to evaluating the serum level of TSP-1 in DFU patients, specimens were taken in Golestan and Emam Khomeini hospitals. The patients then filled a questionnaire form including age, sex, family history, type of diabetes, and other medical information, with the guidance of a healthcare professional. In all participants, Hemoglobin A1c (HbA1c) and fasting blood sugar (FBS) tests, were performed. The study had three groups: Group 1 included 30 diabetic patients without a foot ulcer, Group 2 included 30 diabetic patients with a foot ulcer, and Group 3 included 30 individuals with normal FBS. Group 1 and group 2 participants had a HbA1c of over 6% and blood sugar of over 126 mg/dL, and group 3 had a HbA1c below 6% and FBS below 110 mg/dL.
Exclusion criteria
Patients who were under 20 years old and/or pregnant were excluded from the study as factors that could potentially bias the results.
Patient’s features
The mean age of the first group was 31.3 ± 2.4 years old with a maximum and minimum age of 35 and 28, respectively. The first group was made up of 66.66% (20) female and 33.33% (10) male. The mean age of the second group was 41.2 ± 2.3 years old and a maximum and minimum age of 45 and 38, respectively. Group 2 consisted of 66.66% (20) male and 33.33% (10) female. The mean age of the third group was 51.6 ± 7.7 years old and their maximum and minimum wages were 65 and 40 years old. Group 3 consisted of 83.33% (25) female and 16.67% (5) male. There was no significant correlation between the mean age (P value>0.5) or the sex of the three groups (P>0.5).
Serum level of thrombospondins were measured using a sandwich enzyme-linked immunosorbent assay (ZellBio GMbH kit, Germany). Blood sugar and HbA1c were measured by using pars azmoon (Iran).
Statistical analysis
Statistical package for social sciences (SPSS v.21, IBM Inc., Chicago, IL, USA) software was used for analyzing the data. Quantitative variables were described as mean and standard deviation while qualitative variables were described as frequency and percent. In addition, correlations among three groups were assessed by the Oneway ANOVA test.
Ethical considerations
All the patients filled the informed consent form and this study had no intervention in the treatment process. The study was approved by Tehran University of Medical Sciences and Ethics Committee of Tehran University of Medical Sciences. Participants answered the questionnaire anonymously and the participation in the study was voluntary.
The mean FBS in group 3 was 93.8 ± 9.1 mg/dL and the range of FBS level was 80 to 110 mg/dL. In group 1 the mean FBS was 190.1 ± 23.2 mg/dL with levels ranging from 148 to 223 mg/dL. In group 2 the mean FBS was 223.2 ± 34.8 mg/dL its range was from 173 to 278 mg/ dL (Figure 1). The significant correlation for FBS was tested for the three groups by One-way ANOVA test and Tukey's test (P value=0.01). Between group 1 and 2 compelling correlation was seen, showing that as the level of glucose increases, TSP-1 decreases; which causes an increase in angiogenesis as well as in the amount of patients with a DFU (Figure 1).
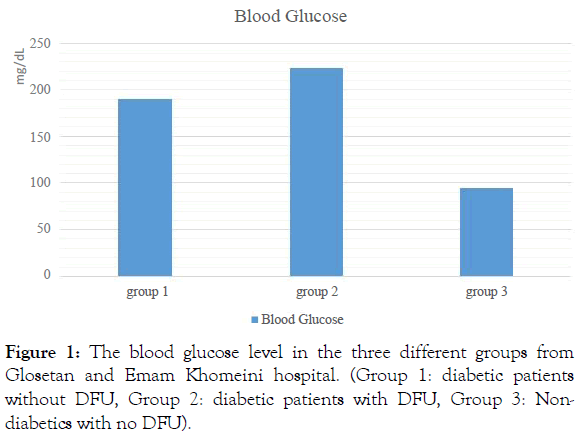
Figure 1: The blood glucose level in the three different groups from Glosetan and Emam Khomeini hospital. (Group 1: diabetic patients without DFU, Group 2: diabetic patients with DFU, Group 3: Non-diabetics with no DFU).
The mean HbA1c in group 1 was 8%, in group 2 it was 10%, and in group 3 it was 5%. The range of HbA1c percentage in each group was 7% to 12% in group 1, 7% to 15% in group 2, and 2% to 6% in group 3 (Figure 2). The statistical analysis by One-way ANOVA test and Tukey's test showed that the correlation for HbA1c among the three groups was significant (P value=0.01) (Figure 2).
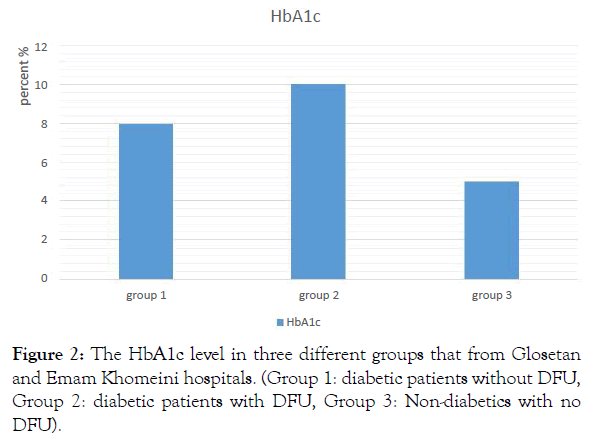
Figure 2: The HbA1c level in three different groups that from Glosetan and Emam Khomeini hospitals. (Group 1: diabetic patients without DFU, Group 2: diabetic patients with DFU, Group 3: Non-diabetics with no DFU).
On the other hand, by increasing HbA1c, TSP-1 decreases. The average level of TSP-1 in group 3 was 1570.42 ± 1047.42 ng/ml with a minimum and maximum amount of 427 and 3400 ng/mL, respectively. The average level of TSP-1 in group 2 was 234.87 ± 129.8 ng/ml with a minimum and maximum amount of 63.9 and 515 ng/ml. Finally, the average level of TSP-1 in group 1 was 266.85 ± 88.75 ng/ml with a minimum and maximum amount of 138 and 450 ng/ml (Figure 3).
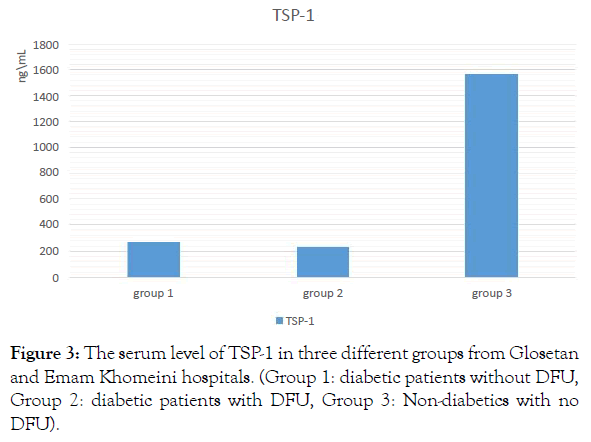
Figure 3: The serum level of TSP-1 in three different groups from Glosetan and Emam Khomeini hospitals. (Group 1: diabetic patients without DFU, Group 2: diabetic patients with DFU, Group 3: Non-diabetics with no DFU).
The Kolmogorov-Smirnov statistical test was used to indicate the normal or abnormal distribution of TSP-1; it showed a normal result(p value=3.076). In the following results, the rate of TSP-1 among different groups was evaluated by One-way ANOVA test, for statistical analysis of variance (ANOVA), which showed to be statistically significant (P value=0.5). The result of this test indicated that there was a significant difference between TSP-1 in groups 1 and 2 (p value=0.01). There is no important difference between group 2 (diabetic group with DFU) and group 3 (not diabetics with no DFU) (p value=0.987) (Table 1).
| Group 1 | Group 2 | Group 3 | |
|---|---|---|---|
| Number | 30 | 30 | 30 |
| Mean age ( years) | 25-30 | 25-35 | 25-35 |
| Mean FBS (mg/dL) | 190.1 ± 23.2 | 223.2 ± 34.8 | 93.8 ± 9.1 |
| Mean HbA1c (%) | 8 | 10 | 5 |
| TSP-1 (ng/mL) | 266.85 ± 88.75 | 234.87 ± 129.8 | 1570.42 ± 1047.42 |
Table 1: Demographic and analytic data in three different groups from Glosetan and Emam Khomeini hospitals. (Group 1: diabetic patients without DFU, Group 2: diabetic patients with DFU, Group 3: Non-diabetics with no DFU).
Diabetes is the most prevalent chronic metabolic disease, which can be described as an abnormality in carbohydrate, protein, and fat metabolism. Diabetes complications are numerous including heart and brain stroke, renal failure, amputation, blindness, and high blood sugar all of which have a detrimental impact on life quality [15]. Furthermore, treatment and diagnosis for the disease are expensive. The prevalence of diabetes type 2 is more than diabetes type 1, according to the World Health Organization (WHO), the estimated global prevalence of diabetes at present is around 9%, which shows a rapid increase over the last decade indicating an increase in prevalence [16]. About 8% of Iranian people (aged ≥ 60 years) were afflicted with diabetes in 2011, but studies show that this will increase to more than 20% in 2020 [17]. As these numbers are raising it is the job of medical professionals to research ways of improving the outcome of diseases, this study showed an important way that this could be done.
The average level of blood sugar among those afflicted with diabetes was too high and patients with a DFU had higher levels of blood sugar in comparison to group 1, which did not have a DFU. Statistical analysis, performed with the one-way ANOVA and subsequently Tukey's post hoc test, indicated that there was a significant difference in HbA1c among groups 1, 2, and 3 (P value˂0.05). Although, the HbA1c level was more in group 2 (DFU patients) than in group 1, there wasn’t any considerable difference between them.
Thrombospondins are a group of multifunctional secretion proteins that consists of TSP-1 to TSP-5. TSP-1 is the first protein of this family and a homotrimeric glycoprotein (450 KD) with a multifunctional domain. In addition, TSP-1 is a powerful mediator for increasing the apoptosis of endothelial cells through activation of the protein kinase path by mutations of CD36, P59FYN, and P38 [18]. Studies showed that TSP-1 have a significant role in a lot of diseases. For example, studies indicated that TSP-1 is a major regulator for activation of transforming growth factor beta (TGF-β), it is with activation of TGF-β signaling that makes fibroblasts activate and increase tissue reconstruction [19]. In addition, TSP-1 decreases the angiogenesis by binding to CD36 and also activates integrin messenger paths, which regulate inflammation, and inhibition of protease [20]. Therefore, it has can be seen that TSP-1 plays an important role in tissue reconstruction and preventing tissue damage.
A study in the United States demonstrated an inhibitory role of Cr3+ on the protein TSP-1 expression in hyperglycemic conditions, which may represent its anti-proliferative reaction. In addition, Cr3+ downregulated O-linked N acetylglucosamine (O-GlcNAc) signaling mechanisms and prevented reactive oxygen species generation. These outcomes of O-GlcNAc signal transduction provide an appropriated link through which Cr3+ may modulate abnormal VSMC function and oxidative stress response under hyperglycemic conditions [21]. Lack of TSP-1 expression is accompanied by a high expression of vascular endothelial growth factor (VEGF) [9]. This expression allows the vessels endothelial cells to migrate and proliferate, which represents a restorative role in diabetic patients. VEGF-A, VEGF-B, VEGF-C, VEGF-D, and VEGF-E and placenta growth factor are all members of the VEGF family of homodimer proteins [22]. Mostly parenchymal cells produce VEGF, but through the negative regulator heat shock protein 70, TGF-β can stimulate osteoblasts to synthesis VEGF, which then acts in a paracrine manner on adjacent vascular cells to regulate neovascularization [23,24].
TSP-1 is a protein that regulates the interaction between cell-cell and cell-matrix, and has increased action when there are damaged vessels wall and in the primary steps of atherosclerotic lesions where it stimulates the vessels smooth muscle cells (VSMC). Based on this information, it can be said that TSP-1 plays an important role in tissue damage related to diabetes. It is presumed that it also plays a role in tissue reconstruction, angiogenesis, and prevention of pervading infections.
This study reached a conclusion that TSP-1 has a significant role in the inhibition of angiogenesis, also by increasing blood sugar and HbA1c, TSP-1 decreases, causing vessel complications, tissue ulcers and neuropathy. In 1971, Folkman expressed that angiogenesis inhibitors have great potential for bio cancer treatment, of which the most important is thrombospondins [20]. In 2000, Dr. Sheibani and his cooperators evaluated TSP-1 level in vitreous and alkaline liquid, they realized that TSP-1 is a natural angiogenesis inhibitor which is reduced under hyperglycemic conditions [25]. On the other hand, TSP-1 effects on inflammation may cause diabetic foot ulcer as we can see from this studies results. This study is consistent with other similar studies showing that glucose levels in group 1, 2, and 3 have a considerable difference and patients with a DFU show a greater difference than those without a foot ulcer. TGF- β is a powerful regulated protein and it is necessary for metabolism, as it effects growth and gene expression. TSP-1, integrinavb6, integrinavb8, MMP-2, and MMP-9 are TGF-β regulating molecules [26]. A reduction of TSP-1 can be caused by a reduction of TGF-β. TGF-β is a multifunctional growth factor produced by myeloma cells, immune cells, bone, and bone marrow stromal cells [27].
Lack of TGF-β can cause immunological diseases, inflammation, growth diseases, wound healing reduction, and an increase in tumors. More activity of TGF-β can cause the development of fibrotic disease, scars in various organs, immune suppression and tumor progression [27].
According to the results presented in this study, it can be concluded that as TSP-1 in diabetic patients decreases there is a consequent increase in angiogenesis. Also, TGF-β, a tissue reconstruction factor, is can be reduced by a reduction of TSP-1. In addition, lack of TSP-1 is accompanied by VEGF high expression, which leads vessels endothelial cells to proliferate. Since the thrombospondin-1 plays a major role in inflammation; which may cause diabetic foot ulcers.
If we measured the TSP-1 serum level when we have an inflammation we may be able to use this in the diagnosis method of diabetic foot ulcers, or even develop it further to use as a preventive medicine. As a last note it is important to remember that prevention of diabetic foot ulcers can also be controlled in diabetics by suitable diet and regular checkups.
Citation: Alizadeh S, Beige ZB, Poor Heravi SA, Nejad FS, Shokri MM, Nazar M (2019) Study of Serum Thrombospondin-1 Level in Diabetic Patients with Diabetic Foot Ulcer. J Mol Pathol Biochem 1:102.
Received: 10-Jan-2019 Accepted: 31-Jan-2019 Published: 08-Feb-2019
Copyright: © 2019 Alizadeh S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.