
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2024)Volume 15, Issue 4
Background: Subarachnoid block is most widely used block all over world amongst all the practices of anesthesia. Thoracic spinal anesthesia a new armamentarium in regional anesthesia has replaced general anesthesia in many cases. But to start this understanding of anatomy of thoracic region is very important. Available studies showed anatomical structures of western world only. India being largest population in the world needs data’s of MRI studies of the persons residing here. This study was done to understand the essentials for thoracic spinal anesthesia by MRI studies.
Materials and methods: The study was done in a tertiary care center with teaching facilities after taking approval from ethical committee and with patient’s consent that this data will be used for study and research purpose. 35 patients were included in the study and MRI study was done with 3.0 Tesla machine in supine position. All the scans retrospectively and calculations were performed at T5, T10 and L1 level of spinal cord.
Results: The anatomy of thoracic spinal canal was studied using magnetic resonance imaging in 35 patients at the MRI facility. All the study subjects underwent MRI in supine position, as most of MRI machines are compatible with supine and not sitting position during procedure.
We can conclude after comparison that the difference between dura mater and spinal cord is more at above measured thoracic level as compared to lumbar areas. This dura to cord distance is maximum at T5 level followed by T10 level and least at L1 level.
Conclusion: We can conclude that distance between dura mater to spinal cord is maximum at T5 level, followed by T10 level. This distance can be safely used for thoracic anesthesia by the expert anesthesiologist.
Anesthesia; Thoracic spinal canal; Spinal anesthesia; Magnetic resonance imaging
BMI: Body Mass Index; MRI: Magnetic Resonance Imaging; SD: Standard Deviation
The regional anesthesia is the most common modality used in majority of operative procedures all over the world and more so is the sub arachnoid block. There are anatomical differences amongst various race and ethnicity. Delving in to scope and safety profile of thoracic spinal anesthesia, urged us to study precise anatomy of spinal cord and surrounding structures. Anatomical details were explained in details in various books, but search for radiological description relevant for anesthesiologist were scarce. The idea for study was developed to ascertain the various radiological anatomical details relevant to an Anesthesiologist and aid in defining safety margin for thoracic spinal anesthesia.
The term “Thoracic spinal anesthesia” was first coined by Jonnesco [1]. The established practice of giving Subarachnoid block beyond the termination of spinal cord for the fear of neurological injury was challenged with advent of new era of thoracic spinal anesthesia. In 2005 van Zundert, et al. [2], conducted laparoscopic cholecystectomy by giving thoracic spinal anesthesia in a patient with severe lung disease. Recently British Journal of anesthesia published an article after compiling available literature on segmental spinal anesthesia [3]. There are many ongoing research and studies in the field of segmental spinal anesthesia. The data pertaining radiological details relevant to anesthesia has only been limited to western world, in studies by Lee, et al. and Imbelloni, et al., [4,5]. In India there has been a growing interest in this field but very scarce studies exist to support and advocate the technique and safety of segmental spinal anesthesia.
The anatomy of thoracic spinal canal was studied using magnetic resonance imaging in 34 patients at the MRI facility. All the study subjects underwent MRI in supine position, as most of MRI machines are compatible with supine and not sitting position during procedure.
The study was done in a tertiary care center with teaching facilities after taking approval from ethical committee and with patient’s consent that this data will be used for study and research purpose. 35 patients were included in the study and MRI study was done with 3.0 Tesla machine in supine position. All the scans retrospectively and calculations were performed at T5, T10 and L1 level of spinal cord. All the demographic details were also recorded.
Patients who were included were patients of age group 18 to 60 years of either sex with no structural abnormality of spine. We excluded patients with spine abnormalities like kyphosis, scoliosis, BMI more than 35 or less than 20.
All the calculations were done by a senior Radiology consultant with experience of 25 years in this field. We calculated average length of thoracic spinal canal (from upper border of T1 vertebrae to upper border of L1 vertebrae), the distance between the skin and posterior dura, skin and spinal cord. The three groups in this study depicts the distance between the dura and spinal cord, at that particular level as mentioned in group name i.e. at T5, T10, and L1 respectively. Calculations were also performed at the angle which is followed while performing lumbar and thoracic puncture during subarachnoid block.
This study included a total of 35 study subjects, among which 19 were male and 16 female patients in age group of 25 to 60 years of age. MRI scans were done in supine position and measurements at MRI console (Figure 1).
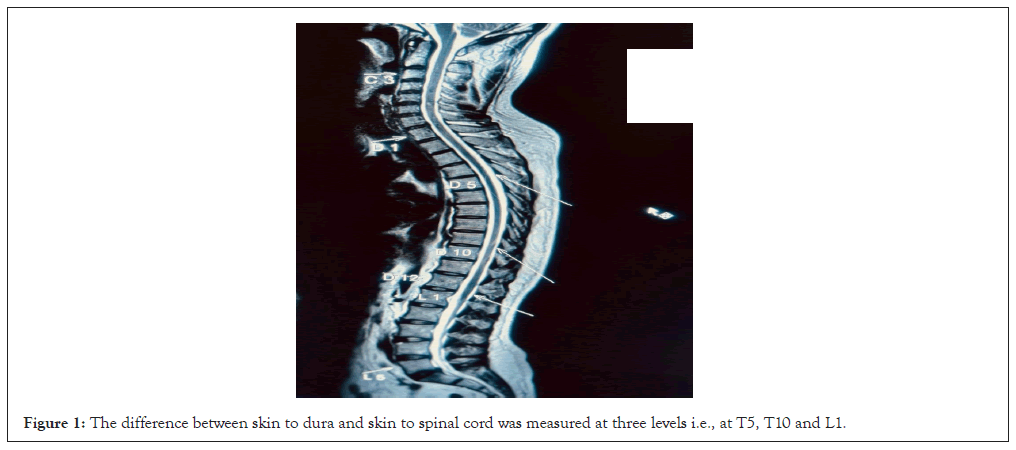
Figure 1: The difference between skin to dura and skin to spinal cord was measured at three levels i.e., at T5, T10 and L1.
An average length of thoracic spinal canal was calculated by taking into account the distance between upper border of T1 vertebrae and upper border of L1 vertebrae.
The mean distance between dura and spinal cord at both T5 and T10 level of spinal cord was more than Lumbar (L1) level.
The Table 1 presents data for 3 groups. Group 1 i.e distance at T5 level, with 35 participants, had a mean ± SD score of 6.5 mm ± 1.5 mm, ranging from 4.1 mm to 10.7 mm. Group 2 i.e distance at T10 level, also comprising 35 participants, had a mean ± SD score of 4.2 mm ± 0.9 mm with values ranging from 3.0 to 5.9 mm. Group 3 i.e distance at L1 level with 35 participants as well, had a mean ± SD score of 3.0 mm ± 0.9 mm, ranging from 1.8 mm to 4.9 mm. The overall mean ± SD score for all groups combined (Total) was 4.6 mm ± 1.8 mm, with individual scores ranging from 1.8 mm to 10.7 mm.
| Group | N | Mean ± Standard deviation | Minimum | Maximum | p-value |
|---|---|---|---|---|---|
| T5 | 35 | 6.5 ± 1.5 | 4.1 | 10.7 | <0.001** |
| T10 | 35 | 4.2 ± 0.9 | 3.0 | 5.9 | |
| L1 | 35 | 3.0 ± 0.9 | 1.8 | 4.9 |
Note: (**): Signifies highly significant p-value.
Table 1: Measurements at various spinal cord levels (all distances calculated in millimeters).
The p-value for the comparison between the groups was <0.001, indicating a significant difference in means across the groups. When values of difference at T5 and T10 were individually compared with values at L1, the p-value was found to be <0.001 thus concluding a significant difference among groups.
We can conclude after comparison that the difference between dura and spinal cord is more at above measured thoracic level as compared to lumbar areas. The Tukey Honestly Significant Difference (HSD) test was used for multiple comparisons between the groups. The results show significant differences between all pairs of groups (Group T5 vs. Group T10, Group T5 vs. Group L1 and Group T10 vs. Group L1) with p-values <0.001. The mean differences, standard errors and 95% confidence intervals are provided for each pair, indicating the magnitude and direction of the differences (Table 2).
| Multiple comparisons | ||||||
|---|---|---|---|---|---|---|
| Tukey HSD (Honestly Significant Difference) | ||||||
| Group | Mean | Standard error | p-value | 95% Confidence interval | ||
| Difference | Lower | Upper | ||||
| Bound | Bound | |||||
| Group T5 | Group T10 | 2.32 | 0.27 | <0.001** | 1.68 | 2.97 |
| Group L1 | 3.55 | 0.27 | <0.001** | 2.9 | 4.19 | |
| Group T10 | Group L1 | 1.22 | 0.27 | <0.001** | 0.58 | 1.87 |
Note: (**): Signifies highly significant p-value<0.001.
Table 2: Comparison of mean difference of distance between dura and spinal cord at three different levels.
We also managed to compare length of thoracic spinal canal among different sex distribution (Table 3).
| Sex | Mean | Standard deviation | p-value |
|---|---|---|---|
| Male | 279.71 | 1.028 | <0.001 |
| Female | 259.85 | 1.285 |
Table 3: Comparison of length of Thoracic spinal canal in mm.
The p-value was found to be highly significant implying a substantial difference of length between both gender groups.
This study was done to overcome the myths about segmental spinal anesthesia, which is a novel concept in the field of central neuraxial blockade. Segmental spinal anesthesia i.e., blockade of a particular segments with the use of very low dose of local anesthetics need punctures above the conventional levels of subarachnoid block for the surgeries of upper abdomen and thorax. Use of very low concentration of local anesthetics can allow us to achieve better hemodynamic stability and respiratory comfort. But the dreaded fear of neurological injury while performing Subarachnoid Block (SAB) at thoracic level was a constraint in the widespread use of this technique. In recent years various studies were published demonstrating and emphasizing the safety profile of this technique.
The radiological measurements done in this study gave us an insight and clarity that this technique is safe and reliable as the distance between dura and cord is enough to avoid any chances of injury to cord by spinal needle. We also had a chance to get a glimpse of anatomical details in Indian population, about which we had no published data earlier. One most important factor to be taken into consideration in Indian scenario is the cost, so proper and careful execution of this technique will definitely reduce the financial burden in a resource limited country.
Studies by Imbelloni, et al. [5], showed that average height of males and females is significantly different than our population. Jonnesco [1], performed spinal punctured for the first time in history at high thoracic T2 levels for the anesthesia of cranium, neck and upper limbs and found it to be safe. Recently a study published in BJA, compiling all the studies on segmental spinal anesthesia and found it to be comparable to general anesthesia [3].
Studies to understand the anatomy of thoracic spine was done in the past by Lee, et al. [4]. He performed his study in 19 healthy volunteers and found position of spinal cord anteriorly in thoracic region and posteriorly in lumbar region contrary to the popular belief.
We also found in our studies of 35 patients of Indian population that spinal cord is almost anterior in thoracic region in supine position giving ample space for spinal anesthesia and it is at the dorsum aspect in lumbar region. At T5 level we got maximum distance of 10.5 mm in one patient and minimum distance of 4.1 mm, indicating presence of ample space for instillation of drugs for subarachnoid block without damaging the spinal cord.
Imbelloni, et al. [5], also studied medial sagittal section at T2, T5 and T10 in 50 healthy volunteers and found that posterior dural-spinal cord distance is significantly greater at the mid-thoracic region (5th thoracic=5.8 +/- 0.8 mm) than at the upper (2nd thoracic=3.9 +/- 0.8 mm) and lower thoracic levels (10th thoracic=4.1 +/- 1.0 mm) (P<0.015). There were no differences between interspaces T2 and T10. There was no correlation between age and the measured distance between the dura mater and the spinal cord. The entry angle of the needle at T2 was 9.0° ± 2.5°; at T5, 45.0° ± 7.4° and at T10, 9.5° ± 4.2°.
Tkiguchi, et al. [6], measured the shift of cauda equine significantly anterior from supine to lateral position with leg flexed using MRI. They also showed dynamical movement of the spinal cord and cauda equine due to changing position. The most significant movements were noted by changing from supine to lateral decubitus position and fully flexed legs at the L2/3 and L1/2 levels, respectively. So they assumed more anterior displacement of spinal cord. The spinal cord follows the straightest line through the imposed geometry of the spinal canal. We also recommend to puncture dura at mid thoracic level in lateral or sitting position.
Accordingly, there is relatively more posterior separation of the cord and surrounding thecal tissue at midthoracic levels in the apex of the thoracic kyphosis. Placing a patient in a position that accentuates the thoracic curvature of the spine (i.e., Sitting head-down) increases the posterior separation of the spinal cord and dural sheath at thoracic levels.
It is also seen by the Imbelloni, et al. [5], that only 29% anesthesiologists were able to put spinal anesthesia at right place moreover around 71% times the space selected is higher [7]. We also scanned L1 level to study the available space for spinal puncture. It is seen in our study that L1 space, preferred by anesthesiologist to perform the block, is having very less space between dura and spinal cord. So actually majority of us have punctured dura at higher level, above the termination of cord unknowingly.
Incidences of dural perforation during epidural catheter placements are quite high in thoracic space. Although incidence of perforation varies. It is seen in previous studies that epidural space at thoracic level is narrower than lumbar region, so incidence of dual perforation is higher in thoracic region than lumbar area [5,8,9]. But the distance between skin to posterior dura is longer in thoracic region than lumbar region, giving a safety feature to the anesthetists. It is also seen in literature that neurological injuries during accidental dura perforation is negligible at thoracic level.
Average length of thoracic canal in both male and female subjects were found to be less than in studies by Lee, et al. [4], it may be of significance in calculating intrathecal dose of the drug to be injected which may be different depending on ethnicity and race with marked variation in anthropometric measurements [5,8]. Although a large multicentric study involving different geographical regions will be needed to compare the variation.
Limitation of the study
It was that it could be conducted in supine position only because in India 99 percent centers are not having machines which can do MRI in sitting position.
The sample size of the study was small, a large subset of population can also be studied using multicentric approach so results can be more reliable and practical.
Thoracic spinal anesthesia although a new evolving technique amongst anesthesiologists which is a promising alternative to general anesthesia in many surgeries. We in India are doing practices of thoracic spinal anesthesia according to studies and demographic profile published in western world. Being largest populated country there is always need of study of essentials for thoracic spinal anesthesia through MRI studies. We found a safe distance between duramater and spinal cord maximum at T5 level followed by T10 level and least at L1 level. This distance can be safely used by an experienced anesthesiologist to give thoracic spinal anesthesia. In order to exclude myths of dura puncture during thoracic spinal anesthesia beyond conventional levels more studies with supportive demographic evidence is warranted in Indian and Asian subcontinent population.
There is no conflict of interest in this study.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Chandra R, Misra G, Pokharia P, Singh PK (2024) Study of Thoracic Spinal Canal in Indian Population with the 3.0 Tesla Magnetic Resonance Imaging: Exploring the Safety Profile of Thoracic Spinal Anesthesia. J Anesth Clin Res. 15:1148.
Received: 26-Jul-2024, Manuscript No. JACR-24-31794; Editor assigned: 29-Jul-2024, Pre QC No. JACR-24-31794 (PQ); Reviewed: 13-Aug-2024, QC No. JACR-24-31794; Revised: 20-Aug-2024, Manuscript No. JACR-24-31794 (R); Published: 27-Aug-2024 , DOI: 10.35248/2155-6148.24.15.1148
Copyright: © 2024 Chandra R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.