Pancreatic Disorders & Therapy
Open Access
ISSN: 2165-7092
ISSN: 2165-7092
Case Report - (2024)Volume 14, Issue 6
Introduction: Pancreatic trauma without injuries to other organs is uncommon and the integrity of the main pancreatic duct is the critical factor in the management and outcome of these patients. Severe injuries or hemodynamic instability require emergent surgical intervention. In contrast, conservative strategy demands close monitoring and regular reassessment to detect any deterioration or complications that may need a change in the treatment plan. We present a case of a grade III pancreatic trauma in a stable and very young patient, successfully treated conservatively.
Case presentation: A 25-year-old male patient presented to the emergency department in context of thoracic and abdominal trauma, due to blunt trauma caused by machine compression. Patient’s symptoms were not severe. On physical examination, his vital signs were within normal limits, with complains of upper quadrants pain but no peritoneal signs. Computed tomography scan showed a complete laceration of the proximal region of the head of the pancreas, with minimal free fluid. Conservative treatment was decided. Magnetic resonance cholangiopancreatography was also performed, revealing two pancreatic fractures with an imperceptible Wirsung duct in practically the entire pancreas, probably collapsed, calling into question the hypothesis of sectioning. Between fractures, there is a segment of necrotic pancreas. The patient remained asymptomatic, with favourable laboratory and imaging evolution. After 5 months, magnetic resonance cholangiopancreatography showed a scar in the body of the pancreas, with no collections.
Conclusions: Non-operative approach plays an important role in the conduct of pancreatic trauma, aiming to preserve function while minimizing the risks associated with surgical interventions.
Blunt abdominal trauma; Pancreatic duct injury; Endoscopic treatment; Non-operative management; Retro peritoneum trauma
Pancreatic trauma occurs infrequently, representing about 0.2% of cases of blunt trauma and 1%-12% of penetrating trauma [1]. Additionally, isolated pancreatic injury is even more rare, comprising less than 3% of cases [2]. Despite advances in trauma and critical care management, pancreatic injuries are still associated with high morbidity and mortality, showing no significant improvement during the past decades [3]. One significant contributing factor is delayed diagnosis, due to the nonspecific or even absent signs and symptoms [1]. The complexity arises from the retroperitoneal location of the pancreas, which provides some protection but can also obscure clinical findings. Furthermore, there is a lack of significant management experience among trauma surgeons. Management of pancreatic trauma depends on several factors, including the hemodynamic stability of the patient, the presence of concomitant organ injury, the location of parenchymal injury, the integrity of the pancreatic duct and the presence of complications, such as necrotic acute pancreatitis, abscesses, fistulas or pancreatic pseudo-cysts [1]. In young and healthy populations, with hemodynamic stability, no signs of peritonitis and no obvious active bleeding on abdominal Computed Tomography (CT) scan, conservative treatment could be considered, with the possibility of emergency surgery if necessary [2]. We report a case of pancreatic duct disruption caused by blunt trauma that was treated conservatively, providing a new option for clinical practice. This case highlights that conservative treatment under close observation is feasible.
A 25-year-old male presented to the emergency department in context of thoracic and abdominal trauma. He experienced an accidental blunt trauma caused by machine compression between a beam and a wall, at work. He complained about chest and abdominal pain, but no dyspnea, nausea, vomiting or other symptoms. His past medical history was unremarkable. Vital signs were within normal limits. On physical examination, his abdomen was rigid and painful in the upper quadrants with rebound tenderness present in these regions. There was no evidence of wounds and no flank or periumbilical bruising (Grey-Turner and Cullen's sign, respectively). Complete blood tests showed normal haemoglobin level (14.7 g/dl) and normal white cell count (7.4 × 109/l). C-reactive protein was not elevated, and lactate level (0.6 mmol/l) was normal. Electrolyte levels, urea and creatinine were all within normal ranges. Liver function tests were abnormal elevated Alanine Transaminase (ALT) and Aspartate Transaminase (AST), respectively (161 U/l, range 4-33 and 125 U/l, range 4-50). He had elevated lipase (258 U/l, range 13-60) and amylase levels (65 U/l, range 13-53). A thoracic CT scan without lesions. CT scan of the abdomen showed complete laceration of the pancreatic parenchyma, with a hypodensity of the pancreatic parenchyma in the neck/ proximal region of the pancreatic body (Figure 1).
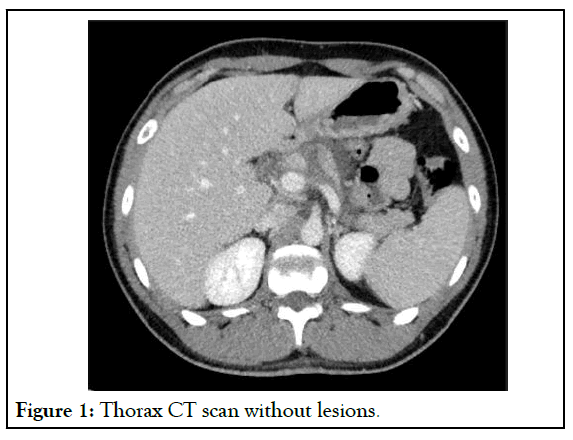
Figure 1: Thorax CT scan without lesions.
Also, minimal peripancreatic fluid was observed as well as fluid in the anterior pararenal space, descending along the paramesocolic gutters. A multidisciplinary team discussed and decided to admit him on an intensive care unit, allowing close and continuous monitoring. Additional measures included pain control, intravenous fluid resuscitation, total parenteral nutrition and antibiotic therapy. The patient remained hemodynamically stable and an abdominal CT scan 24 hours after admission was comparable. On the 3rd day of hospitalization, a Magnetic Resonance Cholangiopancreatography (MRCP) scan revealed two pancreatic fractures with an imperceptible Wirsung duct in practically the entire pancreas, probably collapsed, calling into question the previous hypothesis of sectioning (Figure 2).
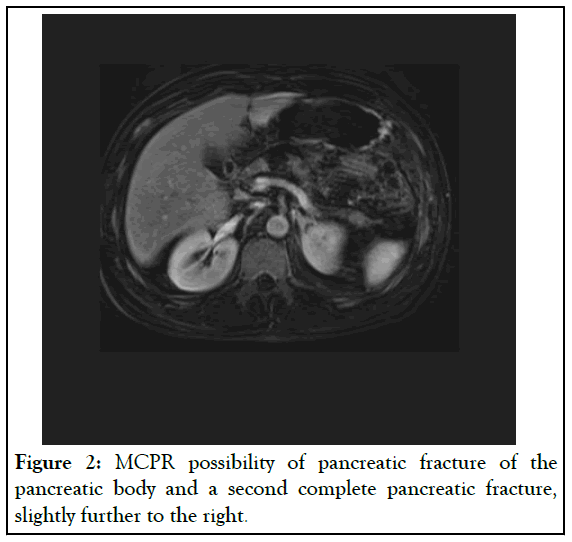
Figure 2: MCPR possibility of pancreatic fracture of the pancreatic body and a second complete pancreatic fracture, slightly further to the right.
Between the two fractures, there is a segment of necrotic pancreas in the tail with no contrast uptake (Figure 3).
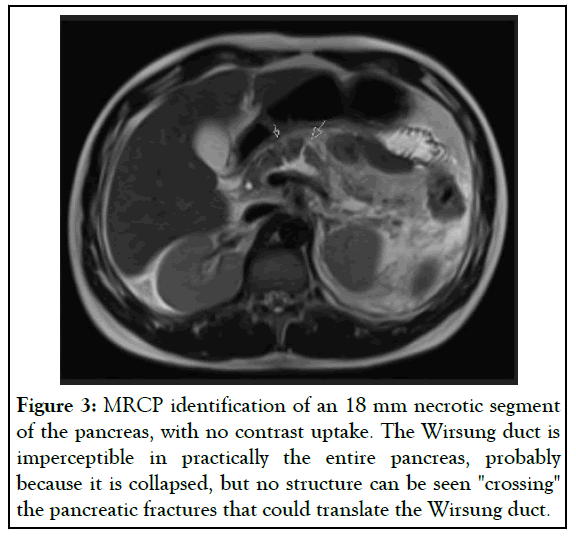
Figure 3: MRCP identification of an 18 mm necrotic segment of the pancreas, with no contrast uptake. The Wirsung duct is imperceptible in practically the entire pancreas, probably because it is collapsed, but no structure can be seen "crossing" the pancreatic fractures that could translate the Wirsung duct.
In laboratory terms, the amylase and lipase values increased up to the 4th day of hospital stay (maximum lipase level of 2026 U/l) and have decreased since this date. On the 8th day of hospitalization, Endoscopic Retrograde Cholangiopancreatography (ERCP) was executed although unsuccessfully. It was not possible to cannulate the Wirsung's duct, so neither sphincterotomy or endoprosthesis implantation was performed. As the patient persisted stable, with no major symptoms and favorable laboratory and imaging results, the resolution was to continue with conservative management. Prolonged hospitalization for 35 days, with various imaging reassessments, but no complications or intercurrences. After 5 months of discharge, MRCP showed a scar in the body of the pancreas and pancreatic tail atrophy, with no collections. One-year follow-up, without complaints.
The pancreas, a retroperitoneal organ, is placed in front of the first and second lumbar vertebrae, which provides a deep and hidden location. Consequently, direct action with compression of the upper abdomen against the spine, mostly sustained in the pancreatic body, is the most common mechanism of injuries [2,4]. Approximately 60% of pancreatic injuries are caused by vehicle crashes as a result of impact against the steering wheel in adults or with bicycle handlebars in children, very similar to machine compression observed in our case [1]. As precepted by this kinetic mechanism, other organs are naturally involved, such as the spleen, liver, or kidney, in 50%-98% of cases [5]. The diagnosis of pancreatic injuries poses challenges, often demanding a multimodal approach [4]. It is crucial to obtain an early diagnosis and CT scan of the abdomen provides the most reliable method for diagnosis and recognition of a pancreatic injuries [4]. Thus, if a pancreatic lesion is suspected, a CT scan must be performed. It should be the initial modality of choice and the sensitivity and specificity reported in pancreatic trauma was between 70% and 80% [6]. Adopting a multimodal and sequential imaging strategy can improve outcome in pancreatic trauma and, to optimize visualization of Wirsung's duct, ERCP or MRCP are useful techniques [4,5]. On the other hand, laboratory tests, particularly serum amylase or lipase levels, play a limited and controversial role in the diagnosis of pancreatic trauma [2]. Amylase levels cannot exclude pancreatic injury during the initial assessment of trauma patients, since their post-traumatic values are influenced by multiple factors, including time since trauma, associated hypotension, craniofacial and bowel trauma [4]. Notably, the degree of amylase elevation does not necessarily reflect injury severity [4]. In an attempt to standardize management in pancreatic trauma, several classification systems have been presented. The main common factor among these is the focus on the presence of injury to the pancreatic duct and its significance as a major prognostic factor [4]. The American Association for the Surgery of Trauma (AAST) Pancreas organ injury scale, published in 1990, is currently the most widely used grading system. According AAST, pancreatic trauma is classified into five grades (Table 1).
| Grade | Description of Injury |
|---|---|
| I | Hematoma with minor contusion or superficial laceration without duct injury. |
| II | Major contusion or laceration without duct injury. |
| III | Distal transection or deep parenchymal injury with duct injury. |
| IV | Proximal transection or deep parenchymal injury involving the ampulla (and/or intrapancreatic common bile duct). |
| V | Massive disruption of the pancreatic head ("shattered pancreas"). |
Table 1: American Association for the Surgery of Trauma (AAST) pancreas organ injury scale.
Grades I and II do not involve the main duct and are considered low-grade injuries. Grades III, IV and V involve the main duct and constitute high-grade injuries [7,8]. Based on the available evidence, drainage is recommended for low-grade injuries and resection with drainage for grade III or higher [3]. Our patient had a grade III pancreatic injury, as per the AAST. However, management approaches for pancreatic injuries remain controversial, primarily based on small retrospective studies without randomized studies addressing this issue [2,3]. Factors such as the site of injury, its type, and the surgeon’s experience play important roles in defining an appropriate strategy [5,9]. Traditionally, grade III pancreatic injuries necessitate surgical resection due to transection of main pancreatic duct in the body or tail of the gland, nevertheless this approach carries substantial morbidity [4]. The current recommendation is typically to resect the distal part, however, recent publications have revealed that drainage alone of the pancreatic bed may be a viable option, even for high-grade injuries [9,10]. Mohseni et al., presented a retrospective study, including a total of 4098 patients with grade III and IV injuries and compared outcomes between resection versus non-resection management [10]. The pancreatic resection group was not associated with a significant decrease in mortality, but it is associated with a significant increase in hospital length of stay. In recent years, the use of ERCP has increased as both a diagnostic tool and a treatment option, with promising results [4]. Particularly for blunt pancreatic injuries with ruptured main pancreatic ducts, placement of an endoprosthesis to facilitates drainage of pancreatic juice into the duodenum may have a role, as the leakage of corrosive pancreatic juice is a main factor contributing to late complications. Although the experience is still very limited to a few cases, the use of endoscopic stenting of the pancreatic duct for the successful treatment of pancreatic duct disruption has been increasingly reported [4]. Endoscopic stent treatment may avoid emergency pancreatic resection and it could become as an adjunct of the nonoperative approach [10]. From 2007 to 2013, Björnsson et al., found that no patients with grade III pancreatic injury have been treated with resection at their institution and describe three cases treated primarily with endoscopic stent placement [4]. In this case it was not effective because Wirsung’s duct was inaccessible. Mei et al., recently narrated a case of conservative treatment of a pancreatic duct disruption in the head and neck caused by trauma that healed spontaneously with no significant complications [2]. Siboni et al., analyzed 388137 patients with blunt abdominal trauma, with 12112 patients (3.1%) presenting pancreatic injury [3]. Isolated pancreatic injury occurred in 2528 (0.7%) and only a small percentage (17.3%) were high-grade. Overall, most patients (74.1%) were managed nonoperatively, namely 48.5% of grade III and 40.9% of grade IV and V. Nonoperative management of minor pancreatic injuries is associated with lower mortality and shorter hospital stay than operative management. However, in severe trauma (grade IV and V), nonoperative management is associated with higher mortality and longer hospital stay. The overall mortality rate was 2.4%, while in severe pancreatic trauma it was 3.0% [3]. It should be noted that the largest experience in the nonoperative strategy is in the pediatric population and it is worth considering whether this data could be extrapolated to the adult patients [11]. Nevertheless, the limited experience available for adult blunt pancreatic trauma patients, although limited, suggest the possibility and safety of a nonoperative approach [8,11]. It is important to note that conservative management may not be suitable for all cases of pancreatic trauma. Severe injuries, multiple concomitant injuries, vessel injuries, or hemodynamic instability require emergent surgical intervention. The optimal treatment strategy can only be formulated after a comprehensive evaluation of the patient’s vital signs, abdominal examination, degree of pancreatic injury and the presence of concomitant organ injury are considered comprehensively [4]. Additionally, close monitoring and regular reassessment are essential during conservative management to detect any deterioration or signs of complications that may necessitate a change in the treatment plan. The most common complications are: Fistula formation which occurs in up to 20%, intra-abdominal abscesses in 20%-25%, pancreatitis around 10%and pseudocyst in 3% [1,4]. The complication rate increases with delayed diagnosis [4]. Whether caused by the injury itself or surgical treatment, pancreatic trauma has a high morbidity risk, and pancreatic surgeries during the acute phase carry high mortality rates. The mortality rate of pancreatic trauma can reach up to 30% and associated morbidity up to 45% [1]. In conclusion, conservative management plays an important role in the treatment of pancreatic trauma, aiming to preserve pancreatic function while minimizing the risks associated with surgical interventions. This is achieved through a combination of interventions, including pain control, intravenous fluid resuscitation, nutritional support, close surveillance, including monitoring of vital signs and close surveillance using imaging techniques such as abdominal CT scans [3,8,12]. By implementing a comprehensive approach that includes supportive care, monitoring and non-surgical interventions, healthcare professionals can optimize outcomes and improve the prognosis for patients with pancreatic trauma.
Blunt pancreatic trauma is a rare and challenging condition. Although different surgical procedures are available to manage patients with pancreatic duct disruption, they all carry high morbidity and mortality rates. Therefore, a more conservative approach may be suitable in selected cases. Recently, endoscopic pancreatic stent placement has proven to be an option as an initial management, supporting nonoperative approach and avoiding resections. The evidence-base for decision-making remains insufficient and the complexity of pancreatic injuries demand updated guidelines, to progress from diagnosis to treatment approach.
AF is responsible conception and design of the article and for writing the manuscript and revisions. DM and CT participated in the design of the article. WM and HL are responsible for surgical care of the patient and critically revision of the article. AC, MM, JS and BP are responsible for critically revised the article. MO is director of the department and participated in the revision of the article.
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [Pubmed]
Citation: Ferreira ARO, Martins D, Tavares C, Louro H, Malta W, Costa A, et al. (2024). Successful Conservative Management of Traumatic Pancreatic Duct Injury: A Case Report and Clinical Update. Pancreat Disord Ther. 14:331.
Received: 01-Nov-2024, Manuscript No. PDT-24-34918; Editor assigned: 04-Nov-2024, Pre QC No. PDT-24-34918 (PQ); Reviewed: 18-Nov-2024, QC No. PDT-24-34918; Revised: 25-Nov-2024, Manuscript No. PDT-24-34918 (R); Published: 02-Dec-2024 , DOI: 10.35841/2165-7092.24.14.331
Copyright: © 2024 Ferreira ARO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.