Journal of Women's Health Care
Open Access
ISSN: 2167-0420
ISSN: 2167-0420
Research Article - (2019)Volume 8, Issue 2
Background: Practicing in a setting where survival of preterm labor is unknown and at best a guess is usually challenging particularly in counseling patients about the outcome of the preterm neonate. The objective of this study was to determine gestational age specific survival of preterm deliveries and its determinants in three teaching hospitals of Addis Ababa University College of health science.
Methods: A prospective cross sectional descriptive study was conducted on newborns delivered from January 1 to June 30, 2017 before gestational age of 37 completed weeks at the three teaching hospitals.
Results: Among 9927 neonates delivered during the study period, 415 (4.2%) were preterm. Of the preterm neonates 407 fulfill the inclusion criteria and analyzed. The cumulative survival rate for preterm babies at the three teaching hospitals is 74.4%. The survival rate of preterm neonates is zero %, 9.1%, 31.8%, 55.2%, 57.6%, 77.4%, 90.4%, 98.6% and 98.8% for GA of 28, 29, 30, 31, 32, 33, 34, 35, and 36 weeks respectively. Majority of neonatal deaths occurs with in the first 2 days (52.5%) and two third (67.1%) of the deaths occurs with in the first 3 days. Birth weight of 1500 grams or above (AOR 3.5, 95% CI 1.5-8.1, P <0.01), GA increment by one week (AOR 2.4, 95% CI 1.9-3.2, P<0.001) and married mother (AOR 3.9, 95% CI 1.2- 12 P< 0.05) are associated with a better chance of neonatal survival in this study. Neonates who required resuscitation after delivery have lower probability of survival (AOR 0.3, 95% CI 0.12-0.64, P< 0.01). Significant association were not found between neonatal outcome and sex of the neonate, parity, duration of labor, duration of ROM, preeclampsia, IUGR, administration of dexamethasone and other maternal socio demographic factors when adjusted for other confounding factors.
Conclusion: Preterm neonates delivered prior to 31 weeks of GA have very low survival rate. So instead of iatrogenically delivering newborn prior to this GA, especially for fetal indication, efforts to push pregnancy at least till 31 weeks should be encouraged for better neonatal outcome. Critical attention should be paid on resuscitative intervention and the first 3 days of life to mitigate factors contributing to high preterm babies’ loss at this particular time. A study to assess the quality of care and cause of very low survival rate of preterm infants is recommended.
Preterm; Survival; Addis Ababa
ABD: Assisted Breech Delivery; ANC: Antenatal Natal Care; AOR: Adjusted Odd Ratio; BLH: Black Lion Hospital; CS: Caesarian Section; EDHS: Ethiopian Demographic Health Survey; GA: Gestational Age; GDM: Gestational Diabetes Mellitus; GMH: Gandhi Memorial Hospital; IAI: Intra Amniotic Infection; LMP: Last Normal Menstrual Period; NICU: Neonatal Intensive Care Unit; PROM: Premature Rupture Of Membrane; PTB: Preterm Birth; SVD: Spontaneous Vertex Delivery; US: Ultrasound; WHO: World Health Organization; ZMH: Zewditu Memorial Hospital
Preterm birth (PTB) is defined by WHO as all births before 37 completed weeks of gestation or fewer than 259 days since the first day of a woman’s last menstrual period. The WHO definition does not define a lower gestational age limit for reporting [1,2]. It includes both spontaneous and provider-initiated births prior to 37 completed weeks. Approximately 45-50% of preterm births are idiopathic, 30% are related to preterm rupture of membranes (PROM) and another 15-20% is attributed to medically indicated or elective preterm deliveries [3].
Preterm birth has been an under recognized and underfunded global health issue, partly because of a lack of data on the worldwide extent of the problem. The new report by the US March of Dimes Foundation, based on data from WHO, attempts to address this deficit by providing the first global and regional estimates of the prevalence of preterm birth. The figures are alarming. In 2005, 13 million preterm babies were born worldwide 85% of these births (11 million births) occurred in Africa and Asia. Africa (11.9%), North America (10.6%), and Asia (9.1%) have the highest rates of preterm birth [4]. Where good-quality trend data are available, preterm births also seem to be increasing in numbers [4].
Mortality due to complications of prematurity is the leading cause of neonatal death, and the second leading cause of death for children under age five [5]. Of the estimated 6.3 million children under 5 who died in 2013, 15.4% were due to complications of preterm birth [5]. Achieving Millennium Development Goal to reduce child mortality is therefore in large part dependent on reducing mortality related to premature birth.
Twenty eight completed weeks is considered as GA of viability in Ethiopia and some developing country. Does a preterm baby delivered at this GA have reasonable chance of survival in our setting? Most of the time we used data from developed countries for counseling mothers due to lack of studies in our settings. But there is significant gap in survival rate between different settings. For example, over 90% of extremely preterm babies (<28 weeks) born in low-income countries die within the first few days of life yet less than 10% of babies of this gestation die in high-income settings, a 10:90 survival gap [6]. In Japan and Sweden survival rate of 54 and 53% were reported with aggressive resuscitation at GA 23 weeks which increases to 77 and 67% at GA of 24 weeks respectively. In other settings with good data at this GA (23 weeks) survival is usually below 50%. In most sites of USA and Norway above 50% survival is achieved at GA of 24 weeks (56-60%). Most of other developed countries achieved this beyond GA of 25 weeks [7-17]. In many developing countries, infants born at 32 weeks of gestation have little chance of survival. In contrast, the survival rate of infants born at 32 weeks in developed countries is similar to that of infants born at term [11]. In one meta-analysis in 4 east Africa countries 94.2% of PTB beyond 34 weeks survived while only 52.6 % of those born before 34 weeks survived [12].
To the author’s knowledge in Ethiopia there is only one study done about neonatal survival in preterm neonates. But it is a retrospective study and many charts were not found and only those admitted to BLH NICU were included to the study. In this retrospective chart review of 397 preterm infants, admitted from July 1, 2011 to June 30, 2012 G.C to the neonatal unit of TAH, reported overall survival of 69.3%. Survival of infants below 28 weeks of GA is 40%, survival for infants between 28-31 weeks of GA is 54.5%. For those between 32-34 weeks of GA is 74.6% and the survival rate for late preterm infants (35-36+6 days) is 100%.GA, birth weight, gender and place of delivery are among the factors associated with survival of preterm infants.
Like other developing countries there is no adequate national or institutional data about chance of survival for babies delivered prematurely. Practicing in a setting where survival of preterm labor is unknown and at best a guess is usually challenging particularly in counseling patients about the outcome of the preterm neonate. This study will generate the evidence of gestational age specific survival in three teaching hospitals that can be used as a baseline. It will also give additional information about prevalence of preterm births in the three teaching hospitals which may give better information about the magnitude of the problem for giving adequate attention and allocating adequate budgets and infrastructures for better care for preterm babies for planners and programmers.
The study was a prospective cross-sectional descriptive survey conducted in Addis Ababa, the capital city of Ethiopia. Specifically, it was carried out in three teaching hospitals from January 1 to June 30, 2017 G.C Tikur Anbesa hospital, Gandhi memorial hospital and Zewditu memorial hospital. GMH and ZMH are teaching hospitals affiliated with Addis Ababa University however managed by Addis Ababa city Health administration bureau. The hospitals offer antenatal, delivery and post natal services to pregnant women coming from all over Ethiopia following the referral system set out by Federal Ministry of Health.
A self-prepared, structured and pre tested questionnaire was used to collect data from the consenting mothers. Residents and midwives working in the respective hospitals were oriented on how to administer the questionnaire for the consenting women. All neonates delivered prior to 37 completed weeks of GA from reliable LNMP or calculated from US done prior to 22 weeks of GA were included to the study group. Preterm neonates who were born with gross congenital malformations known to be incompatible with life, failure to get neonatal outcome after three attempts every week for 28 days, births for whom GA could not be determined were excluded from the study. Neonatal status was checked weekly through phone call till 28 days from delivery date. Data was entered, cleaned and analyzed using SPSS version 20.0 statistical software and presented in descriptive and tabular forms. Statistical analysis was made using chi- square test, fisher’s exact test Kaplan Meier survival analysis and binary logistic regression to reach at a conclusion.
During the six months study period, 9927 neonates were delivered in the three teaching hospitals. Among this 415 neonates were delivered prior to 37 weeks. The outcome of five neonates could not be ascertained due to one is from street with no phone contact and the other four their phones were not working after many attempts. Three cases had lethal congenital anomaly per country’s protocol (one anencephaly and two chiari II malformation). The remaining 407 cases were analyzed (Figure 1).
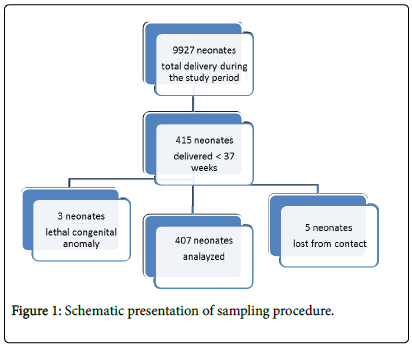
Figure 1: Schematic presentation of sampling procedure.
The socio demographic characteristics of the respondents are described in Table 1. Majority (86%) of the women were in the age group of 20 to 34 years. The minimum age among the participants was 17 and the maximum was 42 with the mean age being 27 years. Among the respondents, 22 (5.4%) were below 20 years of age and 35 (8.6%) were 35 years of age or older.
| Variables | Categories | Alive (%) | Dead (%) | Total (%) |
|---|---|---|---|---|
| Place of delivery | BLH | 81 (72.3) | 31 (27.7) | 112 (27.5) |
| ZMH | 91 (71.7) | 36 (28.3) | 127 (31.2) | |
| GMH | 132 (78.6) | 36 (21.4) | 168 (41.3) | |
| Total | 304 (74.7) | 103 (25.3) | 407 (100) | |
| Address | Addis Ababa | 286 (74.3) | 99 (25.7) | 385 (94.6) |
| Out of Addis Ababa | 18 (81.8) | 4 (18.2) | 22 (5.4) | |
| Age | <20 years | 17 (77.3) | 5 (22.7) | 22 (5.4) |
| 20-34 years | 263 (75.1) | 87 (24.9) | 350 (86) | |
| 35 or above | 24 (68.6) | 11 (31.4) | 35 (8.6) | |
| Ethnicity | Oromo | 66 (72.5) | 25 (27.5) | 91 (22.4) |
| Amhara | 140 (77.3) | 41 (22.7) | 181 (44.5) | |
| Tigre | 32 (60.4) | 21 (39.6) | 53 (13) | |
| Others | 66 (80.5) | 16 (19.5) | 82 (20.1) | |
| Marital status | Single | 26 (65) | 14 (35) | 40 (9.8) |
| Married | 278 (75.7) | 89 (24.3) | 367 (90.2) | |
| Religion | Orthodox | 217 (75.1) | 72 (24.9) | 289 (71) |
| Muslim | 66 (71) | 27 (29) | 93 (22.9) | |
| Protestant | 21 (84) | 4 (16) | 25 (6.1) | |
| Occupation | Housewife | 171 (73.4) | 62 (26.6) | 233 (57.2) |
| Government employee | 47 (77) | 14 (23) | 61 (15) | |
| Private employee | 65 (79.3) | 17 (19.7) | 82 (20.1) | |
| Daily labourer | 21 (67.7) | 10 (32.3) | 31 (7.6) | |
| Educational level | Illiterate | 49 (73.1) | 18 (26.9) | 67 (16.5) |
| Read and write | 19 (63.3) | 11 (36.7) | 30 (7.4) | |
| Primary education | 125 (77.6) | 36 (22.4) | 161 (39.6) | |
| Secondary education | 59 (68.6) | 27 (21.4) | 86 (21.1) | |
| Tertiary education and above | 52 (82.5) | 11 (17.5) | 63 (15.5) |
Table 1: Socio demographic characteristics of pregnant mothers with preterm delivery in the three teaching hospitals, Addis Ababa, 2017.
A vast majority of respondents were from Addis Ababa (94.6%), married (90.2%), and housewives (57.2%). About thirty nine percent (39%) of respondents had completed primary school, 15.8% had no formal education and only 15.3% had attended higher education.
Among the 355 mothers who gave birth to 415 preterm infants in the three teaching hospitals, 44.2% of mothers were prim gravid, 52.6% were multigravida and the remaining 3.2% were grand multipara. Among 407 infants 200 (49.1%) were delivered by SVD, 193 (47.4%) by CS 5 (1.2%) by ABD and the remaining 9 (2.2%) infants were delivered by instrumental delivery. Majority of infants 303 (74.5%) were delivered as singletons while 104 (25.5%) were delivered as twins. Majority of the preterm infants 168 (41.3%) were delivered at GMH, whereas 127 (31.2%) and 112 (27.5%) of infants delivered at ZMH and TAH respectively.
Among 407 preterm infants 256 (62.9 %) were due to spontaneous preterm labor and in 151 (37.1%) cases induction or cesarean section was done for maternal or fetal indications. Majority of the mothers have either medical or obstetric complications like preterm PROM (23.1%), Preeclampsia (32.9%), IUGR (11.1%), multiple pregnancy (25.5%), Intra amniotic infection (2.2%), and Diabetes mellitus (1.7%). Both preeclampsia and IUGR were found in 10.7% of cases.
During the six months study period, among a total of 9927 newborns, the number of preterm deliveries were 415. The prevalence of preterm delivery was 4.2%. From the 407 newborns who fulfill the inclusion criteria, 230 (56.5%) were late preterm infants (34+0-36+6 weeks), 90 (22.1%) moderate preterm and 87 (21.4%) were very preterm infants, 219 53.8%) were males and 188 (46.2%) were females.
Among 407 preterm newborns 304 (74.7%) newborns were survived to 28th day while 103 (25.3%) neonates died. Almost one fourth (24.3%) of neonatal deaths occurs within the first 24 hours of delivery while majority of neonatal deaths occurs with in the first 2 days (52.5%) and two third (67.1%) of the deaths occurs with in the first 3 days. Only 10 neonates (9.7%) died after day 6th days of life (Figure 2; Table 2).
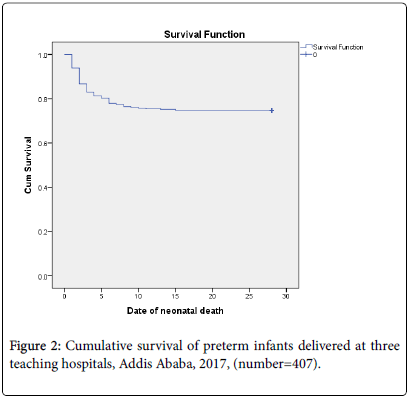
Figure 2: Cumulative survival of preterm infants delivered at three teaching hospitals, Addis Ababa, 2017, (number=407).
| Gestational age | Total N | N of Events | Censored | |
|---|---|---|---|---|
| N | Percent | |||
| 28 | 14 | 14 | 0 | 0.00% |
| 29 | 22 | 20 | 2 | 9.10% |
| 30 | 22 | 15 | 7 | 31.80% |
| 31 | 29 | 13 | 16 | 55.20% |
| 32 | 59 | 25 | 34 | 57.60% |
| 33 | 31 | 7 | 24 | 77.40% |
| 34 | 73 | 7 | 66 | 90.40% |
| 35 | 71 | 1 | 70 | 98.60% |
| 36 | 86 | 1 | 85 | 98.80% |
| Overall | 407 | 103 | 304 | 74.70% |
Table 2: Survival of preterm neonates delivered at three teaching hospitals for GA, Addis Ababa, 2017, (Number=407).
Neonatal survival significantly increase when GA increases 14 neonates died out of 14 preterm neonates delivered at GA of 28 (0% survival) weeks while only two neonate died at GA of 35 and 36 weeks from 155 preterm neonates (98.7% survival) (Figure 3).
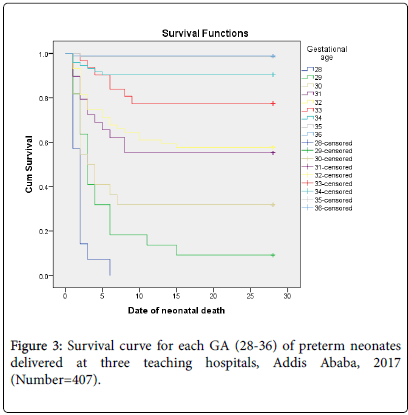
Figure 3: Survival curve for each GA (28-36) of preterm neonates delivered at three teaching hospitals, Addis Ababa, 2017 (Number=407).
In this study GA is the most important predictor of neonatal survival. Every one week increment of GA, neonatal survival increases by 2.5 folds (COR-2.45, 95% CI 2.04-2.9, P<0.01). Preterm neonates born between GA of 32 and 34 weeks have 4.5 times higher survival rate (COR-4.5, 95% CI, 2.4-8.5, P <0.01) and neonates born at 34 weeks or above have 60.9 folds higher survival rate than preterm neonates born prior to 32 weeks (COR-60.9, 95% CI 27-137, P<0.01). Birth weight is the other independent variable found to have statistically significant association with neonatal survival. Neonates with birth weight of 1500 grams or above have significant association with survival (COR-20.3, 95% CI 11.5-35.6, P < 0.01) (Table 3).
| Birht wt WHO | Total N | Deaths | Survive | ||
|---|---|---|---|---|---|
| N | Percent | N | Percent | ||
| <1000 | 15 | 15 | 100% | 0 | 0.00% |
| 1000 -1499 | 86 | 56 | 65.10% | 30 | 34.90% |
| 1500 -2499 | 244 | 32 | 13.10% | 212 | 86.90% |
| ≥2500 | 62 | 0 | 0% | 62 | 100.00% |
| Overall | 407 | 103 | 25.30% | 304 | 74.70% |
Table 3: Survival and birth weight per WHO’s classification of preterm neonates delivered at three teaching hospitals, Addis Ababa, 2017, (Number=407).
Other independent variables found to have significant evidence of association with neonatal survival were multiple pregnancies (COR-4.2, 95% CI 2.6-6.8, P<0.01), antenatal corticosteroids (COR-2.6, 95% CI 1.6-4.1, P<0.01), 1st minute Apgar score of 7 or above (COR-9.9, 95% CI 4.2-23, P<0.01) and 5th minute Apgar score of 7 or above (COR-6.4, 95% CI 3.2-12.5, P<0.01).
IUGR (COR-0.3, 95% CI 0.2-0.6, P<0.01), need of resuscitations (COR-0.15, 95% CI 0.1-0.2, P<0.01) and NICU admission (COR-0.06, 95% CI 0.02-0.2, P<0.01) have significant association with poor neonatal survival.
But after controlling for other confounding variables multiple pregnancies, antenatal dexamethasone, Apgar score, duration of labor, IUGR and NICU admission has no statistically significant association.
After adjusting for other factors neonates delivered at TAH (AOR-5, 95% CI 1.8-13.5, P<0.01) and GMH (AOR-4.1, 95% CI 1.7-9.9, P<0.01) has better survival rate than ZMH. Married women (AOR-3.9, 95% CI 1.2-12, P<0.05), birth weight of 1500 grams or above (AOR- 3.5, 95% CI 1.5-8.1, P<0.01) and GA increment by one week (AOR- 2.4, 95% CI 1.9-3.2, P<0.001) are associated with better neonatal survival. The AOR for neonatal survival between 32 +0 and 33+6 weeks and 34 weeks or above are 2.9 (95% CI 1.2-6.7, P<0.05) and 30.87 (95% CI 9.6 -99.01, P<0.001) respectively compared to neonates delivered before 32 completed weeks. Neonates who required resuscitations after delivery are less likely to survive than who doesn’t (AOR-0.3, 95% CI 0.12-0.6, P<0.01). The following table shows some selected independent variables, which shows some association with crude OR and AOR after adjusting for confounding factors.
Other independent variables like socio demographic factors, parity, preeclampsia, IUGR, PROM, duration of ROM and duration of hospital stay, mode of delivery, and fetal sex have no association with neonatal survival in this particular study (Table 4).
| Independent variables | B | S.E. | Wald | Df | COR | P value For AOR | Exp (B) (AOR) | 95% C.I. for AOR | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| COR | 95% CI | Lower | Upper | - | |||||||
| Hospital (ZMH-constant) | - | - | 12.487 | 2 | - | - | 0.002 | - | - | ||
| TAH | 1.612 | 0.512 | 9.917 | 1 | 1 | .6-1.8 | 0.002 | 5.011 | 1.838 | 13.661 | |
| GMH | 1.404 | 0.451 | 9.68 | 1 | 1.5 | .8-2.5 | 0.002 | 4.072 | 1.681 | 9.862 | |
| Marital status | 1.358 | 0.582 | 5.451 | 1 | 1.7 | .8-3.4 | 0.02 | 3.89 | 1.244 | 12.168 | |
| PROM | 0.817 | 0.449 | 3.314 | 1 | 2.1* | 1.1-3.8 | 0.069 | 2.264 | 0.939 | 5.454 | |
| IUGR | -0.396 | 0.556 | 0.508 | 1 | .34*** | .2-.6 | 0.476 | 0.673 | 0.226 | 2 | |
| Multiple pregnancy | 0.866 | 0.479 | 3.267 | 1 | 4.2*** | 2.6-6.8 | 0.071 | 2.378 | 0.93 | 6.082 | |
| Birth weight ≥ 1500 grams | 1.261 | 0.424 | 8.86 | 1 | 20.3*** | 11.5-35.6 | 0.003 | 3.528 | 1.538 | 8.091 | |
| Corticosteroids | 0.178 | 0.399 | 0.199 | 1 | 2.6*** | 1.6-4.1 | 0.656 | 1.194 | 0.547 | 2.608 | |
| Duration of labor ≥ 12 hrs. | -0.458 | 0.565 | 0.657 | 1 | 2.9** | 1.4-6 | 0.418 | 0.632 | 0.209 | 1.915 | |
| 1st min APGAR (<5 constant) | - | - | 1.091 | 2 | - | - | 0.58 | - | - | - | |
| 5-6 | 0.865 | 0.852 | 1.03 | 1 | 1.98 | .9-4.6 | 0.31 | 2.374 | 0.447 | 12.612 | |
| ≥ 7 | 0.94 | 0.925 | 1.032 | 1 | 9.9*** | 4.2-23 | 0.31 | 2.56 | 0.417 | 15.701 | |
| Fifth min APGAR ≥ 7 | -0.967 | 0.683 | 2.003 | 1 | 6.4*** | 3.2-12.5 | 0.157 | 0.38 | 0.1 | 1.451 | |
| Resuscitation | -1.324 | 0.448 | 8.719 | 1 | .145*** | .1-.24 | 0.003 | 0.266 | 0.111 | 0.641 | |
| GA (28-31+6)-constant | - | - | 38.91 | 2 | - | - | 0 | - | - | - | |
| GAC (32-33+6) | 1.058 | 0.43 | 6.069 | 1 | 4.5*** | 2.4-8.5 | 0.014 | 2.882 | 1.242 | 6.69 | |
| GA ( ≥ 34) | 3.43 | 0.595 | 33.277 | 1 | 60.9*** | 27-137 | 0 | 30.874 | 9.627 | 99.013 | |
| Constant | -5.426 | 1.799 | 9.092 | 1 | - | - | 0.003 | 0.004 | - | - | |
Note: Significant at *-P value<0.05, **-P value<0.01, ***-P value<0.001
Table 4: Association between selected independent variables and neonatal survival in preterm neonates delivered in three teaching hospitals, Addis Ababa,2017 (number=407)
Subgroup analysis was done for preterm neonates delivered prior to 34 complete weeks of GA for selected variables. In addition to GA, multiple pregnancy (AOR-4.3 % CI, 1.4-12.7, P<0.05) and birth weight 1500 gram or above (AOR-4.3, 95% CI 2.1-8.6, P<0.001) were associated with better neonatal survival. Requirement of resuscitation is associated with poor neonatal survival. But statistically significant association was not found between neonatal survival and antepartum corticosteroid (AOR-0.5, 95% CI, 0.2-1.2, P=0.133), first and 5th min Apgar score and place of delivery.
This study provides the prevalence of preterm deliveries, survival rate for each GA and maternal and obstetric factors associated with survival of preterm neonates in the three teaching hospitals in Addis Ababa. The prevalence of preterm delivery in this study (4.2%) is lower than both national and global reports. One cross sectional study in Brazil showed a prevalence of 21.7 % [6]. A study done in USA had reported rates of PTB as 12.5% in 2004 and 12.8% in 2006 [10]. Similarly in developing countries the rate of PTB is higher than this report. In 2011 in Tanzania, the rate of PTB was reported as 11.4% [11-13]. In Ethiopia the prevalence of PTB was estimated to be 10.1% which was reported by the global action report on PTB in 2010 [14].
In general studies done in Ethiopia shows lower prevalence of PTB than other developing countries. This could be partly due to exclusion of preterm neonates due to difficulties in estimating GA. In one cross sectional study conducted in Addis Ababa in 2010 the prevalence of PTB was 7.1% which was lower than the global action on PTB report but higher than the report of this study [15,16]. Recently in 2016 Gebresilasie reported the prevalence of PTB in Gondar among 540 deliveries (4.4%) which was lower than previous reports but similar to this study [16]. The lower rate of PTB in this study may be also partly due to strict criteria for assessment of GA.
The gap in survival of preterm neonates between developed and developing countries were clearly seen in this study. In some countries like Japan, where at least some centers appears to be more aggressive in resuscitation at GA of 22 weeks, survival in one large multicenter series was 34% at the time of discharge from the NICU [12]. In this study comparable survival was achieved at GA of 30 weeks (31.8%). There were no survived neonates at GA of 28 weeks in this study. In one study done in Niger Delta University teaching hospital in Nigeria, among 152 preterm babies the overall survival rate was 65.9%. Survival rate was 11.1% before 28 weeks, 26% between 28 and 30 weeks and reaches 58% at 30 weeks. Even though the overall survival rate in this study is higher (74.7% vs. 65.9%), the survival rate of very preterm newborns were much lower in this report (0% vs. 11.1% before 28 weeks, 5.6% vs. 26% at 28-30 weeks, 31.8% vs. 58% at 30 weeks).
In Japan and Sweden survival rate of 54% and 53% were reported with aggressive resuscitation at GA of 23% which increases to 77 and 67% at GA of 24 weeks respectively. In most sites of USA and Norway above 50% survival is achieved at GA of 24 weeks (56-60%). Most of other developed countries achieved this beyond GA of 25 weeks [7,8,10-17]. Fifty percent of survival was achieved at GA of 31 weeks in this study (55.2%), by which time in developed countries survival is usually above 90%. This wide gap of survival rate of preterm neonates from developed countries is partly due to lack of mechanical ventilator and surfactant in the three teaching hospitals while the high rate of neonatal sepsis and asphyxia could also contribute.
In one meta-analysis in four east Africa countries, 94.6% of PTB beyond 34 weeks survived while only 52.6% of those born before 34 weeks survived [12]. The survival rate of late preterm neonates in our study were comparable (96.1% vs. 94.6%), but survival before 34 weeks is lower in our study (46.9% vs. 52.6%).
In one retrospective chart review done at TAH, cumulative survival rate was 69.3% and the survival rate for preterm infants <28, 28-31 and 32-34 weeks of GA were 40%, 54.4% and 76.6% respectively. Even though only 46% of charts were retrieved, the survival rate of very preterm neonates reported was higher than our study but it was comparable for moderate preterm neonates (40% at<28 weeks vs. 0% at 28 weeks, 54.4% vs. 28.7% at 28-31 weeks, and 76.6% vs. 76.1% at 32-34 weeks). The cumulative survival rate was better in our study (74.7% vs. 69.3%). Since 54% of preterm neonates were not analyzed it is difficult to use this figure reliably. So the exaggerated survival rate of extremely preterm and very preterm neonates may be due selection bias as all cases were not included in the study.
The above study also reported that birth weight, gender and place of delivery are among the factors associated with survival of preterm infants. In our study there was significant association between survival of preterm infants and GA, birth weight and place of delivery, but there was no statistically significant association with sex of the infant. Many studies show association of female sex with better survival. Deliveries at TAH and GMH have a better probability of survival than infants delivered at ZMH. This is partly due to the level of primary care providers in the NICU at ZMH are interns. But this needs a critical evaluation of the quality of care of all three centers before specific conclusion.
Other factor associated with neonatal survival was marital status. Preterm infants of married mothers are more likely to survive than others. Many studies showed that the still birth, neonatal and post neonatal mortality rates are higher among offspring of unmarried mothers. One study done in three sub- Saharan countries showed Burkinabe single mothers were 1.3 times more likely to have their child die as a neonate compared to their married counterpart [16].
In this study almost one fourth (24.3%) of neonatal deaths occurs within the first 24 hours of delivery while majority of neonatal deaths occurs with in the first 2 days (52.5%) and two third (67.1%) of the deaths occurs with in the first 3 days and this indicates that intensive cares and vigilance in the first 72 hours of life are crucial for the survival of preterm infants. This is similar to the above study done at TAH NICU which reported that 40.5% of preterm newborns died in the first 24 hours. This figures shows that initial care for the newborn infants is still suboptimal like in other developing countries.
This study also shows need of resuscitation during delivery was associated with poor survival chance. A retrospective study done in South Africa shows resuscitation at birth was associated with poor neonatal survival (0.46, 95% CI, 0.30-0.69, P<0.001) which is similar to this study [16]. In addition to the primary reason for need of resuscitations this may be partly explained by the routine use of 100% oxygen for neonatal resuscitation in all units of three teaching hospitals which is against WHOs recommendation. During ventilation of preterm babies born at or before 32 weeks of gestation, WHO recommended to start oxygen therapy with 30% oxygen or air (if blended oxygen is not available), rather than with 100% oxygen [15].
Many (at least 8) trials demonstrated that the use of low oxygen concentration or air for preterm babies resuscitated with PPV immediately after birth was associated with a 37% lower risk of overall or in-hospital mortality (RR 0.63, 95% CI 0.44-0.92). This shows the need to appropriate resuscitation skills and supplies in addition to maintaining normal temperature environment at the time of resuscitation, a critical issue to be looked into.
In summary this study shows lower prevalence of preterm birth compared to prior local and international estimates. Delivery prior to 31 weeks of GA have very low survival rate and increment of GA by one week significantly improves the survival rate of preterm infants. So Instead of induction or iatrogenic delivery of newborns, especially for fetal indication, efforts to push pregnancy at least till 31 weeks should be encouraged for better neonatal outcome. Majority of neonatal deaths occurs with in the first three days. Birth weight gestational age, marital status, place of delivery and need of resuscitation are factors with statistically significant association with neonatal survival. So, critical attention should be paid on resuscitative intervention and the first 3 days of life to mitigate factors contributing to high preterm babies’ loss at this particular time.
Ethics approval and consent to participate
Ethical clearance was obtained from the Ethical clearance committee of Addis Ababa University, college of health sciences. Communication to the medical director of each hospital was made through formal letter obtained from Department of Obstetrics and Gynecology, Addis Ababa University and permission was given to cascade the study. In order to keep confidentiality of any information provided by study subjects, the data collection procedure was anonymous. Participation was on voluntary basis after verbal consent and they could withdraw from the study at any time.
Consent for publication
Not applicable
Availability of data and materials
All datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors have no conflicts of interest.
This study was funded by Addis Ababa University, College of health sciences. The funding body had no role in the design of the study or in collection, analysis and interpretations of data.
Tilksew Dagnachew: made the design of the study, supervise data collection, analyzed and interpreted the data and was a major contributor in writing the manuscript.
Mahlet Yigeremu: made substantial contributions to conception and design, analysis and interpretations of data. Both authors read and approved the final manuscript.
I would like to express my deepest gratitude to Yirgu Gebrehiwot for being supportive particularly during data analysis.
Citation: Dagnachew T, Yigeremu M (2019) Survival of Preterm Neonates and its Determinants in Teaching Hospitals of Addis Ababa University. J Women's Health Care 8:461. doi:10.35248/2167-0420.19.8.461.
Received: 13-Feb-2019 Accepted: 23-Apr-2019 Published: 30-Apr-2019
Copyright: © 2019 Dagnachew T, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.