
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Research Article - (2022)Volume 12, Issue 1
Background: Opioid-Induced Constipation (OIC) is one of the most common types of complications affecting patients following opioid treatment for cancer pain. Lactulose has been shown to be an effective drug for managing OIC symptoms in clinics. Acupuncture is a non-invasive approach for relieving constipation and pains. However, the co-applications of Acupuncture and Lactulose for OIC have been rarely evaluated.
Materials and methods: To confirm the advanced therapy effects of Acupuncture and Lactulose co-application, 80 OIC patients in Hebei Province Hospital of Chinese Medicine are included in the randomised clinical trial. Two groups were assigned, including the co-application group with Manual Acupuncture and oral lactulose (AC-LA group) and the control group of pure oral Lactulose Administration (LA group). Forty patients are allocated into each group randomly. Scores of pain, symptoms, and Quality Of Life (QOL) at Day 0 (the day before treatment), Day 7, and Day 14 of treatments are recorded to evaluate the outcomes of OIC therapy in both the AC-LA and LA group.
Results: Compared with pure oral lactulose treatment, the combined Manual Acupuncture sessions produced a higher effective rate after seven days (LA 60.53% vs. AC-LA 89.47%, P<0.001) and 14 days (LA 76.32% vs. AC- LA 92.11%, P=0.081) of treatment. The overall symptom scores of the AC-LA group reduced by more than the LA group following one week (LA 18.5% vs. AC-LA 33.6%, P<0.05) or two weeks (LA 39.5% vs. AC-LA 55.8%, P<0.05) of treatment with Manual Acupuncture. Along with the reduced overall symptom scores, the symptoms of defecation straining, harder stool, extended defecation time and intervals, and the feeling of incomplete defecation were relieved in both LA and AC-LA groups. Acupuncture enhanced the remission effects of each constipation sub- symptoms. Though the KPS quality of life scores did not improve significantly, additional acupuncture treatment helped relieve pain in cancer patients (Day 0 6.89 ± 1.66 vs. Day 14 6.05 ± 1.43, P=0.020).
Discussion and conclusion: As a non-invasive approach, acupuncture put on add-up effects for oral lactulose treatment in relieving Opioid-Induced Constipation symptoms. The co-application of acupuncture and lactulose is a considerably better strategy for pain and constipation management of cancer patients in clinics.
Acupuncture; Opioid-Induced Constipation; OIC; Lactulose; Constipation symptom; Pain; Quality of life
Cancer pain is one of the most suffering symptoms that reduce the life quality of patients [1]. Opioids are recommended as one of the main painkillers for clinical management of moderate to severe cancer pains according to the three-step analgesic ladder principle proposed by World Health Organization (WHO) [2]. Acknowledging opioids' advanced performance in relieving pains, their side effects, including nausea, vomiting, and constipation, are frequently observed in about 90% of patients [3], whereas Opioid- Induced Constipation is the most common intestinal side-effect that reduces patients' quality of life after long-term opioid application [4]. These adverse effects will further restrict the continuous opioid application for cancer pain management. Therefore, along with opioids, oral lactulose is commonly prescribed to prevent or improve the symptom of Opioid-Induced Constipation (OIC) [5].
Acupuncture as a traditional Chinese approach has been known and applied as a non-invasive method for cancer pain treatment and is also reported to be an effective therapy way for relieving constipation symptoms [6]. However, rare studies have evaluated the synergic effects of acupuncture on lactulose treatments of OIC. Our recently published meta-analyses [7], of acupuncture therapy on OIC patients indicated that pure acupuncture treatment showed comparative effects as the lactulose administration. At the same time, the co-application of both strategies significantly reduced the symptoms of OIC than lactulose alone. However, there were only two of included studies [8,9] in this meta-analysis had applied both acupuncture and lactulose in combination; Both of them conducted Electronic Acupunctures but not the traditional Manual Acupuncture. To further confirm the add-on effects of acupuncture, especially the Manual Acupuncture in clinical treatments of OICs, we conducted this randomised clinical trial to address these aims.
Study subjects
In total, 80 OIC patients receiving opioids with the symptoms of constipation in Hebei Province Hospital of Chinese Medicine, China, from September 2018 to August 2019, were included in the study.
Patients were allocated into the AC-LA group (combined treatments of oral lactulose and Manual Acupuncture) and LA group (oral lactulose treatment only) with the random number table. Each group contains 40 OIC patients regardless of the cancer subtypes. Patients were followed up for two weeks till the end of the treatment. Two patients of each group were lost from following up on their requirements without obvious malignant symptoms or other side effects. At the end of following up, 38 patients of each group completed the treatments and the outcome assessments, which were included in the final datasets for data analyses.
Diagnostic and including criteria
The included OIC patients were diagnosed by two experienced practitioners independently following Camilleri’s multidisciplinary working group consensus statement [10]. In simple, the patients after at least seven days of opioid treatments, showed constipation symptoms: 1) Bowel movement frequency was reduced; 2) Developed or increased defecation difficulty or straining; 3) Feeling of incomplete rectal evacuation; 4) Harder and drier stool. Diagnoses of all included cases were agreed upon between the two practitioners.
All included OIC participants were malignant cancer patients diagnosed with photographic and pathological proofs. The expected survival lifetime of the participants was at least three months, without apparent dysfunction in the heart, liver, kidney, and bone marrow. To avoid the potential adverse outcomes during the investigation, the participants aged 19-80 years with the quality of life score, Karnofsky (KPS) score, of at least 60, were selected. The included patients developed OIC symptoms after their first administration of opioids according to the OIC diagnostic criteria, without a history of laxative application before the investigation. OIC patients with 1) Other intestinal diseases such as intestinal obstruction, 2) History of laxative application within 1 week of OIC diagnosis, 3) Female patients in the periods of menstruation, pregnancy, or lactation, and 4) Other patients unable to cooperate with the treatments were excluded.
Treatment
Patients in both the LA and AC-LA groups took 15 ml Lactulose Oral Solution (0.667 g/ml lactulose, H20065730, Hanmi Pharm Co., Ltd.) 3 times a day, for 14 days. In addition, patients in the AC-LA group received Manual Acupuncture therapy at the acupoints of bilateral ‘Zusanli’, ‘Shangjuxu’, ‘Xiajuxu’, ‘Taichong’, and ‘Tianshu’. The therapy session was conducted once a day for 14 days. The duration of each session was 20 min. Before each acupuncture session, the needles (with a diameter of 0.3 mm and 40 mm in length, Suzhou Medical Appliance Factory) and acupoints were routinely sterilised. For each session of treatment, patients lay in a supine position, and acupunctures were conducted by inserting the needles into the acupoints with finger pressure in a vertical direction referencing to the skin. The needles were left at the acupoints for 20 min when ‘De Qi’ sensations were achieved; needle twisting and lifting was manipulated every 10 min for stimulation. Patients in the LA group received sham acupuncture with the same frequency and duration.
Pain assessment
Pain status before and after treatments at Day 0 and Day 14 was scored with the Numerical Rating Scale (NRS) [11,12] in a 0-10-point range. Score 0 referred to ‘no pain’, while score 10 represented ‘the worst pain ever possible'. Score 1-3 points were ranked as mild pain, which did not influence normal daily life. Score 4-6 points indicated moderate pain that disturbed sleep and daily activities, and analgesics may be required. Score 7-10 points were severe pain, causing autonomic nerve dysfunctions, for which the application of analgesics is a must. Pain NRS scores were recorded in a patient self-reported manner.
Constipation symptom assessment and therapeutic effect evaluation
The constipation symptom scores were recorded and evaluated based on the Constipation Symptom Questionnaire produced by the Chinese Society of Colorectal Surgery (CNSCRS) [13]. The symptom scale of constipation was assessed on five items, defecation straining or difficulty, stool property, defection duration, discomfort or incomplete defecation, and frequency of defecation (times per day). Stool property scores were evaluated following Bristol Stool Scale [14]. For other items, the symptom was scored in a range of 0-3, indicating the occurrence rate of none, occasionally, sometimes, and frequently. The summarized points of all five items are recorded as the total symptom score.
The therapeutic efficacy after one week and two weeks of treatments were ranked as Cured, Obvious efficacy, effective, and ineffective according to the ‘Guidance principle of clinical study on new drug of traditional Chinese medicine’s [15]. The criteria for each category are listed in Table 1.
| Therapy efficacy | Cured | Remarkably effective | Effective | Ineffective |
|---|---|---|---|---|
| Symptom changes | Regular defecation and stool property, or recovered to the condition before sickness | Symptoms are remarkably relieved; Defecation interval and stool property are close to normal; or stool is slightly dry and defecation interval is within 72 hours. |
Defecation interval is shortened by 1 day, symptom of dry stool is improved. | No improvement in constipation symptoms |
Table 1: Definition and criteria of therapy efficacy following Opioid-Induced Constipation (OIC) treatments.
Quality of life evaluation
The Karnofsky Scale (KPS) was used for life quality assessment of OIC patients on Day 0 (before treatment), Day 7, and Day 14 of treatments. In simple, KPS is on a 0-100 scale with an interval of 10 points [16]. A score of 100 points is the highest score that represents good life quality without any complaints or evidence of health problems, while the score of 0 points means the status of death. The score range of 80-100 is a sign of normal life quality in carrying regular work and daily activities, without the requirement of any special care. People with 50-70 points are not able to carry on work or normal activities, may require additional care or assistance occasionally. The groups of people with 10-40 points are disabled or very sick, particular cate or hospitalisation are necessary.
Data analyses
Data were recorded in Excel and analysed with SPSS 17.0. For numerical data, the difference between two groups (AC-LA vs. LA group) was subjected to a student t-test. Comparisons among multiple groups (Day 0, Day 7, and Day 14) were tested with one-way ANOVA. Categorical data comparisons between groups were evaluated with the Chi-squared test. The significant levels of statistical tests were set as 0.05.
Within 76 included patients completed the treatments for 14 days, 38 patients received only oral lactulose treatment (LA group), and another 38 patients were treated with both oral lactulose and Manual Acupuncture (AC-LA group). There were 44 male patients (21 in the LA group, 23 in the AC-LA group) and 32 female patients (17 in the LA group, 15 in the AC-LA group). They were cancer patients with the opioid administration for pain relief. The average age of patients in the LA group was 61.82 ± 9.31, while the mean age of the AC-LA group was 66 ± 9.99. No statistically significant difference was identified between the ages (P=0.063) and genders (P=0.648) of LA and AC-LA groups.
Among the patients receiving 14 days’ treatments, the dominant cancer types were lung cancer (27 cases) and cancers of the digestive system (34 cases), followed by gynaecological cancers (5 cases) and other types including soft tissue sarcoma, kidney cancer, brain cancer, etc. (Table 2). The distribution of cancer types in the LA and AC-LA group was of no statistical difference.
| Treatment groups | Cancer types | Total | Chi-square test | P | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Digestive system cancer | Gynecologic cancer | Other cancers | ||||||||||
| Lung cancer | Stomach | Esophageal | Colon | Rectum | Pancreas | Liver | ||||||
| LA group | 14 | 6 | 1 | 2 | 5 | 2 | 2 | 3 | 3 | 38 | 1.957 | 0.582 |
| AC-LA group | 13 | 6 | 3 | 3 | 3 | 1 | 0 | 2 | 7 | 38 | ||
Note: LA group: Treatment with oral lactulose; AC-LA group: Treatment with both oral lactulose and manual acupuncture.
As it’s shown in Table 3, there were no cured cases on Day 7 in both LA and AC-LA groups. In respective, 23 patients showed effective symptom relief after seven days of oral lactulose administration (LA group), while 34 patients with additional Manual Acupuncture sessions (AC-LA group) at Day 7 got remarkably effective (14 cases) remission or effective remission (20 cases) of the constipation symptoms. The overall effective rate in the AC-LA group (89.47%) was higher than in the LA group (60.53%) (P<0.001). After 14 days of treatments, the effective rate of the LA group increased to 76.32%, with 8 cases showing remarkably effective remission and 21 patients showing effective remission. Simultaneously, the effective rate of the AC-LA group had risen to 92.11%, with two cured cases, 14 remarkably effective cases, and 19 effective remissions. The overall effective rate in the AC-LA group was still higher than in the LA group, though the statistical test did not show obvious significance (P=0.081).
| Days of treatment | Treatment groups | Patient number | Cured | markedly effective | effective | Ineffective | Overall effective rate | Chi-square | P |
|---|---|---|---|---|---|---|---|---|---|
| Day 7 | LA group | 38 | 0 | 0 | 23 | 15 | 60.53% | 20.578 | <0.001 |
| AC-LA group | 38 | 0 | 14 | 20 | 4 | 89.47% | |||
| Day 14 | LA group | 38 | 0 | 8 | 21 | 9 | 76.32% | 6.736 | 0.081 |
| AC-LA group | 38 | 2 | 14 | 19 | 3 | 92.11% |
Note: LA group: Treatment with oral lactulose; AC-LA group: Treatment with both oral lactulose and manual acupuncture.
Table 3: The efficacy of acupuncture treatments at day 7 and day 14.
The changes in symptom scores following treatment with lactulose or combined treatment with acupuncture are shown in Table 4. The overall symptom at Day 7 and Day 14 of treatments in both the LA group and AC-LA group were improved with reduced symptom scores in comparison to Day 0. The overall symptom score of the LA group reduced by 17.5% on Day 7 and 39.1% on Day 14. Symptom scores of the AC-LA group produced a reduction of 33.6% and 55.8% in overall symptom scores at Day 7 and Day 14, respectively. The overall symptom scores in the AC-LA group after seven days (P=0.001) or 14 days (P=0.003) of treatment were lower than LA group, indicating the improved therapeutic effects of combing lactulose with acupuncture.
| Items | Treatment group | Number of patients | Day 0 | Day 7 | Day 14 |
|---|---|---|---|---|---|
| Defecation straining | LA group | 38 | 2.63 ± 0.49 | 2.16 ± 0.64* | 1.76 ± 0.85*^ |
| AC-LA group | 38 | 2.5 ± 0.51 | 1.84 ± 0.68* | 1.21 ± 0.81*^ | |
| P value (LA vs. AC-LA) 38 |
0.253 | 0.04 | 0.005 | ||
| Stool property | LA group | 38 | 2.24 ± 0.63 | 1.71 ± 0.80* | 1.53 ± 0.73* |
| AC-LA group | 38 | 2.39 ± 0.72 | 1.66 ± 0.63* | 1.45 ± 0.60* | |
| P value (LA vs. AC-LA) | 0.313 | 0.751 | 0.607 | ||
| Defecation time | LA group | 38 | 2.21 ± 0.66 | 1.76 ± 0.75* | 1.29 ± 0.65*^ |
| AC-LA group | 38 | 2.16 ± 0.68 | 1.37 ± 0.67* | 0.82 ± 0.73*^ | |
| P value (LA vs. AC-LA) | 0.734 | 0.018 | 0.004 | ||
| Incomplete defecation | LA group | 38 | 1.71 ± 0.61 | 1.58 ± 0.68 | 0.89 ± 0.69*^ |
| AC-LA group | 38 | 1.79 ± 0.53 | 1.11 ± 0.73* | 0.58 ± 0.55*^ | |
| P value (LA vs. AC-LA) | 0.549 | 0.005 | 0.031 | ||
| Defecation interval | LA group | 38 | 2.00 ± 0.70 | 1.71 ± 0.57 | 1.11 ± 0.56^ |
| AC-LA group | 38 | 2.29 ± 0.61 | 1.34 ± 0.75* | 0.87 ± 0.74*^ | |
| P value (LA vs. AC-LA) | 0.058 | 0.018 | 0.12 | ||
| Overall symptom score | LA group | 38 | 10.79 ± 1.44 | 8.92±1.67* | 6.58 ± 2.24*^ |
| AC-LA group | 38 | 11.13 ± 1.23 | 7.39 ± 2.14* | 4.92 ± 2.42*^ | |
| P value (LA vs. AC-LA) | 0.269 | 0.001 | 0.003 | ||
Note: *P<0.05 compared with Day 0; ^ P<0.05 compared with Day 7. Data were shown in means and standard deviations. P values among different days were tested with one-way ANOVA, while data between groups were analysed with t-test. LA group: Treatment with oral lactulose; AC-LA group: Treatment with both oral lactulose and manual acupuncture.
Table 4: Constipation symptom scores at day 7 and day 14 of treatment with acupuncture.
For sub-items of constipation symptoms, defecation straining, stool property, defecation time, incomplete defecation, and defecation intervals of AC-LA group with acupuncture treatment were improved obviously at both Day 7 and Day 14 of treatment, compared to Day 0 (P<0.05). The scores of sub-symptoms apart from stool property were further improved at Day 14 in reference to Day 7 (P<0.05). In the LA group, the application of lactulose also reduced the symptom scores of defecation straining, stool property, and defecation time after 1 or 2 weeks of treatment; however, the feeling of incomplete defecation and defecation interval did not improve obviously at Day 7 or at both Day 7 and Day 14 of administration. In overall, the efficacy of co-applied acupuncture and lactulose were better than merely lactulose administration in relieving the symptoms of defecation straining, defecation time, incomplete defecation, and defecation intervals. However, additional acupuncture did not enhance the therapeutic effect of lactulose on stool property.
Besides the improved symptoms and increased effective rate, the pain intensity of patients at Day 14 was also reduced with additional acupuncture treatment (Day 0 6.89 ± 1.66 vs. Day 14 6.05 ± 1.43, P=0.020), as it was shown in Figure 1. In contrast, the pain intensity of patients treated with oral lactulose only did not show a statistically significant reduction in pain scores (Day 0 6.21 ± 1.66 vs. Day 14 5.95 ± 1.64, P=0.490). In the aspect of quality of life, the KPS scores of both the LA group and AC-LA group with or without acupuncture increased slightly at both Day 7 and Day 14 of treatments without statistical significance (Table 5).
| Treatment group | Number of patients | Day 0 | Day 7 | Day 14 | P (ANOVA test within Day 0,7 and 14) |
|---|---|---|---|---|---|
| LA group | 38 | 68.42 ± 5.47 | 69.47 ± 8.04 | 70.00 ± 6.58 | 0.587 |
| AC-LA group | 38 | 67.11 ± 6.11 | 68.68 ± 8.11 | 69.47 ± 8.37 | 0.387 |
| P value (LA vs. AC-LA) | 0.326 | 0.671 | 0.761 | ||
Table 5: Quality of life (KPS) scores following combined acupuncture treatment.
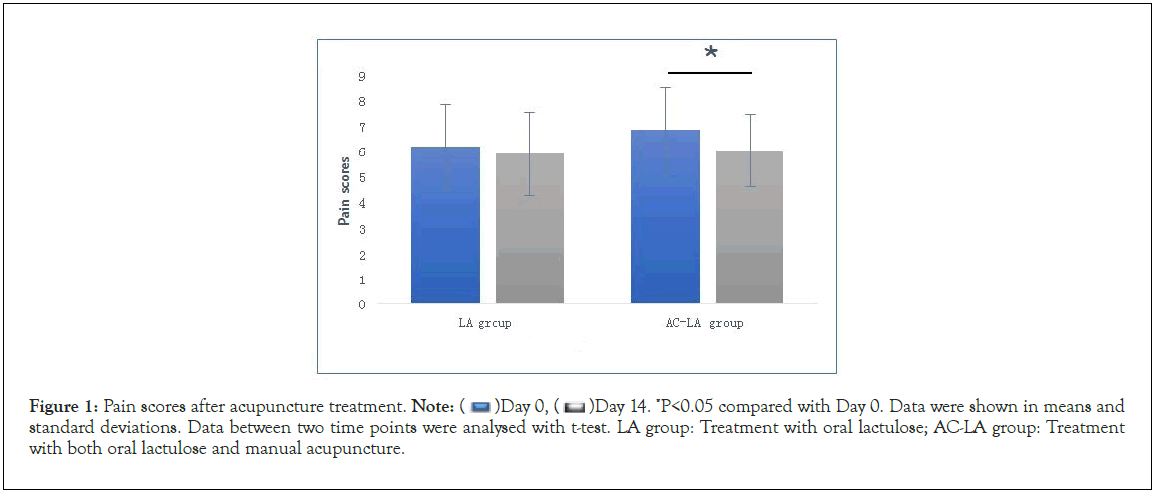
Figure 1: Pain scores after acupuncture treatment. Day 14. *P<0.05 compared with Day 0. Data were shown in means and standard deviations. Data between two time points were analysed with t-test. LA group: Treatment with oral lactulose; AC-LA group: Treatment
with both oral lactulose and manual acupuncture.
Day 14. *P<0.05 compared with Day 0. Data were shown in means and standard deviations. Data between two time points were analysed with t-test. LA group: Treatment with oral lactulose; AC-LA group: Treatment
with both oral lactulose and manual acupuncture.
The current study, for the first time, confirmed the synergic effects of traditional Manual Acupuncture on oral lactulose treatment of Opioid-Induced Constipation. Electronic Acupuncture (EA) and Transcutaneous Electrical Nerve Stimulation (TENS) have been reported to enhance the clinical therapy of laxatives or other medications in the management of OIC [7-9]. However, the apparatus for EA or TENS may not be widely available to practitioners. Manual or Manual Acupunctures with only needles are more accessible for applications in most undeveloped or developing countries. Considering the stimulation duration of each acupuncture session, EA is produced with a longer time of 20- 30 min, while the active stimulation time of Manual Acupuncture is only about a few seconds apart from the indwelling intervals [17]. Therefore, some studies suggest that EA provides superior or faster analgesia effects than Manual Acupuncture (MA) [18,19]. However, there are still no consistent conclusions that can be made on the advanced performance of EA over MA [17], since many other studies comparing EA and MA regarding their analgesia functions in relieving pains or other distressing symptoms do not identify any clear difference [20,21]. Our present clinical trial with Manual Acupuncture confirmed the findings from the previous metaanalysis that co-application of acupuncture with oral medication enhanced laxatives’ therapeutic effects on OIC. In terms of applying acupuncture as a supportive approach for relieving OIC, Manual Acupuncture is suggested to be a comparative or replaceable method for EA or TENS.
In evaluation of the therapeutic effects of acupuncture, besides the practical ways, the most promising variability of clinical acupuncture application depends on selecting acupoints or acupuncture points. In this current study, bilateral ‘Zusanli’ (ST36), ‘Shangjuxu’ (ST37), ‘Xiajuxu’ (ST39), ‘Taichong’ (LR3), and ‘Tianshu’ were used for Manual Acupuncture sessions. Among them, ‘Zusanli’, ‘Shangjuxu’, and ‘Tianshu’are the most frequently applied acupuncture points in clinical treatments of functional constipation based on intelligent big data analyses [22]. They are also the critical acupoints for regulating the autonomic nervous system and intestinal peristalsis [23]. An additional combination of Taichong (LR3) and Xiajuxu (ST39) helps stimulate intestinal movements, improve gastric emptying, and relieve abdominal distention and pains [24]. Synergistic effects of combined acupoints (Taichong LR3 and Taixi KI3) have been observed in activating brain regions compared to single acupoint stimulation [25]. Our results also support the claim that the combination of multiple acupoints is a relatively advanced way for fast relieve of the symptoms of constipation with 7 days than single acupoint treatment at Tianshu (ST25) with therapeutic effects typically observed after 14 days of treatments [9].
Limitations
Manual Acupuncture (MA) is a safe approach; however, managing the technique of proper Manual Acupuncture at the right acupoints needs professional training and preferred long-time experience. Inter-personal variability between different practitioners may bring potential biases in the outcome evaluation of individual cases. Improvement of quality of life scores (KPS) following both lactulose or combined acupuncture-lactulose treatments were not observed. To avoid potential malignant outcomes during the investigation, the patients with relatively 'good' status with a KPS score of at least 60 were included for the trial. The relatively high KPS score impeded the observation of improved life quality for cancer patients. At the average age above 60 with moderate-severe cancers in different organs or tissues, the overall quality of life is difficult to be promoted into a status of being able to conduct normal activities and taking care of themselves [16]. Therefore, in future trials with an attempt of declaring the changes in life qualities of patients with severe diseases, the including criteria need to be adjusted or switching to other scales with more detailed items for scoring the quality of life, like Patient Assessment of Constipation Quality of Life Questionnaire (PAC-QOL) [26].
Acupuncture is a safe and straightforward approach that can enhance the therapeutic effects of oral lactulose treatment in relieving Opioid-Induced Constipation symptoms. The coapplication of Manual Acupuncture not only speeds up the symptom remission of OIC but also promotes the pain-relieving effects. Therefore, the co-application of acupuncture, showing a synergic effect on lactulose therapy of OIC, is a considerably better strategy for pain and constipation management of cancer patients in clinics.
CH leads the enrolment of patients and conduction of treatment of two groups. YL leads the data collection, data analyses, and manuscript writing. HF supervised the project and contributed to the patient enrolment. DL, ZD, PM, LWa, and LWe contribute to the diagnoses and inhospitable care of the patients. All authors contributed to project design and manuscript revising and have agreed on the manuscript context and the submission to the journal.
This work was supported by the Scientific Research Project of Hebei Administration of Traditional Chinese Medicine (Grants No. 2019030). YL was supported by BHF Program Grant RG/15/12/31616. The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
This clinical investigation protocol had been reviewed and approved by the medical ethics committee of Hebei Province Hospital of Chinese Medicine, Shijiazhuang, China (No. HBZY2019- KY-185-01). All participants and their families agreed to the consent of taking part in this clinical trial with signed agreement forms. All the procedures in this investigation were conducted according to the principles of the Declaration of Helsinki.
We have no competing interests to disclose.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [Pubmed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Han C, Liu Y, Li D, Du Z, Ma P, Wang L, et al. (2022) Synergic Effects of Acupuncture and Clinical Lactulose Therapy on Opioid-Induced Constipation. J Clin Toxicol. 12:503.
Received: 31-Jan-2022, Manuscript No. JCT-22-15762; Editor assigned: 02-Feb-2022, Pre QC No. JCT-22-15762 (PQ); Reviewed: 14-Feb-2022, QC No. JCT-22-15762; Revised: 21-Feb-2022, Manuscript No. JCT-22-15762 (R); Published: 28-Feb-2022 , DOI: 10.35248/2161-0495-22.12.503
Copyright: © 2022 Han C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.