International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Original Research Article - (2021)
Background: Neurorehabilitation is facing a unique challenge as COVID-19 circumstances magnify the access and resource barrier in healthcare provision; and are causing disruption in the continuity of care of children with disability. An affirmative action is required as a ‘Disability-inclusive response to the COVID-19 crisis.’ This study thus aimed to determine if Telerehabilitation (TR) model of service delivery is a feasible and effective alternative for pediatric neurophysiotherapy.
Methodology: This is a clinical trial conducted on children diagnosed with developmental delay or neurological condition and referred for Physiotherapy at a tertiary care center. Clinical consultation was provided remotely with the use of real time interactive technology. Outcome indicators used were: 1)Timely receipt of physiotherapy services; 2) Child’s clinical outcomes; and 3) Familiy’s acceptability and satisfaction with the provision of TR.
Results: With regards to feasibility, the most common issues faced during TR sessions were technical; lack of time with mother; child’s medical illness, etc. Children’s clinical outcomes showed improvement reported as ‘acquisition of developmental skills’ and ‘the use of appropriate functional behaviors to meet their needs’. Families showed satisfaction with TR services however, expressed the need for in-person sessions.
Conclusion: In the current scenario, TR may enhance the capacity of families to meet the needs of their child with a disability by connecting them with health care providers, resources and supports; thus ensuring continuity of care. While guidelines to tackle this unprecedented situation continue to develop, TR demonstrates the potential as an alternative rehabilitation strategy thereby ameliorating the impact of social distancing on underprivileged children. However, some psychosocial factors act as barriers to feasibility of TR in pediatric population.
Telerehabilitation; Pediatric; Neurophysiotherapy; Disability; COVID-19
Neurological disorders in pediatric age group encompass a variety of congenital or acquired conditions related to brain or peripheral nervous system; and include brain injuries, cerebral palsy, spinal injuries, neuromuscular disorders and musculoskeletal conditions. Pediatric neurorehabilitation is designed to promote development and improve quality of life of infants and children who have been identified as having a disability or developmental delay [1]. The primary goal of pediatric neurorehabilitation services is to enhance the functional development of young children with disabilities; and also to enhance the capacity of families to help their child learn, achieve developmental milestones, and participate in home and community activities. Early intervention services for children from birth through two years of age are mandated by Part C of the Individuals with Disabilities Education Act (IDEA) [2].
Neurorehabilitation is a spiral management process in which a treatment program is initiated and then constantly revised and updated, based on therapy-mediated improvements [1]. It is effective when the assessment and treatment are initiated at an early stage; and continued with an appropriate and timely followup. It requires a long term approach where the therapy aims to ensure continuity of care all the way from injury onset to the highest possible level of recovery of function; and also address the medical complications of the injury or illness.
Neurorehabilitation is considered as an integral component of neurology services, because of the morbidity and disability occurring due to neurological disorders. However, challenges of accessibility to these services invariably go hand in hand with disability. Various physical, social, and environmental factors create barriers to routine care for children with disabilities, especially in the low or middle income countries [3]. However, COVID-19 pandemic has further intensified the inequalities in accessing health services and information. Social distancing measures implemented to control the spread of infection have magnified the environmental barriers and have disproportionately impacted persons with disabilities [4]. To make the matter worse, many children with disabilities have co-existing health conditions such as poor built and nutritional status; compromised pulmonary functions that make them more susceptible to contracting the virus; experiencing more severe symptoms upon infection; and leading to elevated levels of death. Foreseeing the future too, new regulatory policies at national and hospital level may imply such as continued social distancing and restricted exposure of children to social places; depriving these children from essential health care services. Neurorehabilitation is thus facing a unique challenge as COVID-19 circumstances magnify the access and resource barriers in healthcare provision and is causing disruption in the continuity of care.
As mentioned previously in the RPWD act (2016) and emphasized in the current situation, persons with disabilities in need of health services should not be deprived; and health care providers must proactively reach to address accessibility barriers in response to service delivery gap. An affirmative action is required as a ‘Disability-inclusive response to the COVID-19 crisis’ [4,5].
As such in the times of global contagion like COVID-19 followed by global lockdown, the neurorehabilitation process has countlessly evolved in its delivery process with support from advances in technology. A number of approaches emerged at various places each with its own rationale.
While guidelines to tackle this unprecedented situation continue to develop, Telerehabilitation (TR) is already being adopted as promising practices around the world. TR is a delivery model that uses digital/telecommunications technologies to provide therapeutic and rehabilitation services from a remote location [6]. TR is a relatively new and developing field of telehealth [7]. In the literature, TR demonstrates the potential to deliver pediatric neurorehabilitation services effectively and efficiently. TR has the potential to build capacity among caregivers and local providers as well as promote family-centered services through remote consultation [7-9]. TR can be provided within a child’s home or community setting with no travel necessary for families. In the current scenario, TR may enhance the capacity of families to meet the needs of their child with a disability by connecting families and caregivers with health care providers, resources and supports, thus ensuring continuity of care. TR could prove as an effective rehabilitation strategy thereby ameliorating the impact of social distancing on underprivileged children. With an increase in the various neurological disorders in this population and the need for continuity in care in their long protocol of rehabilitation, TR needs to be considered as one of the effective and innovative solutions in the context of COVID-19.
This study thus aimed to determine the outcome of a telerehabilitation model for pediatric neurophysiotherapy in a tertiary care hospital. The specific objectives outlined are:
1. To determine the feasibility of TR model for pediatric neurophysiotherapy.
2. To determine the clinical outcomes of TR model for pediatric neurophysiotherapy.
3. To determine the acceptability by caregiver/family of the children with neurophysiotherapy needs.
Research question: What is the feasibility and utility of telerehabilitation model in pediatric neurophysiotherapy?
Research hypothesis: Telerehabilitation model of service delivery is a feasible and effective alternative for pediatric neurophysiotherapy in the context of COVD-19 crisis.
Review of literature: The literature search conducted for the present study focused on ‘telerehabilitation in pediatric conditions’ and ‘telerehabilitation in India’. Systematic reviews in clinical rehabilitation services and prospective studies indicate that telemedicine offers great opportunities to healthcare in general and for rehabilitation services [7-12]. However, the effectiveness of TR to improve health and therapeutic outcomes is an emerging field of research. TR could be particularly beneficial for resource constrained countries like India, where rehabilitation is compromised due to lack of access to and dearth of resources for services and skilled professional care [13].
Advantages of TR
1. The biggest advantage of this model is reducing treatment gap by providing health service at the doorstep, especially to unreached needy patients [14].
2. Cost-effective treatment: It reduces the need for patients to travel to the rehabilitation center to receive services and in general reduces the costs of both healthcare providers and patients compared with traditional inpatient or person-to-person rehabilitation [10].
3. Improvement in clinical process and clinical outcomes [15].
Barriers in implementation
1. The most common issues faced during TR sessions can be technical such as power failures, low bandwidth and poor internet connectivity, with power outages in resource constrained countries [13]. This is compounded by old devices, such as the laptop or personal computer, which can hinder the audio-visual clarity at both ends. In addition, the computer literacy of patients and caregivers can also pose as a challenge.
2. Lack of awareness of TR and its scope of practice amongst health professionals [16,17].
3. Shortages of personnel trained in TR [16,17].
Thus, from previous research, TR has the potential benefits for both the patient and the healthcare systems. Despite increased reporting about TR research, many clinicians are still not using it which may be due to lack of knowledge, technical skills, understanding or its accessibility. Clinicians who have used it in the past have been driven by local need and availability of infrastructure. TR has considerable potential to address the treatment gaps, but while this is theoretically feasible, attempts to implement it in public sector facilities have not been very successful.
Strategies in successful implementation of TR require trained users to ensure optimization of use; workplace change and investment in technology [18,19]. These can be enlisted as below:
1. Health professional development
2. Building capacity of local providers through consultation with remote experts
3. Formulating rules and regulations to govern TR services
4. Provision of infrastructure and technical facilities
5. Developing provider and caregiver expertise and experiences with technology
6. Non-technical skills training to build confidence
Feasibility and utility of TR in India
A retrospective file reviewed teleneurorehabilitation consultations provided through Telemedicine Center at a quaternary hospital-based research center in south India between August 2012 and January 2016 [20]. This study aimed to analyze the socio-clinical parameters, feasibility, and utility of teleneurorehabilitation services in India. Adult patients with central nervous system- related disorders such as stroke, cerebral palsy, and tubercular meningitis with sequelae or neuromuscular disorders such as Guillain–Barre Syndrome and Duchenne muscular dystrophy received consultation. The findings suggest that teleneurorehabilitation services are feasible, effective, and less resource intensive in delivering quality telemedicine care in India.
Another study demonstrated the potential to use TR to improve access and reduce costs associated with receiving care for osteoarthritis for patients living in rural communities [21]. This study found the use of TR via videoconferencing to be more effective than a well-designed progressive home exercise program with weekly telephone consultations to reduce pain and improve function.
To summarize the existing literature indicates that
• TR has the potential to enhance rehabilitation service provision for children having neurological disability or developmental delay by enabling access to services unavailable within local communities and by complementing existing services. Yet, at present limited evidence is available to guide the specific needs of children with disability. There is a need to collect experiential and evidence-based data on the quality of rehabilitative care in pediatric neurophysiotherapy.
• It is well established that differences between countries such as supportive system influence the patterns of this delivery model.
TR service model is feasible in India; however, more clinical studies are required to elucidate its full utility at different levels and in different parts of the country.
• Neurological rehabilitation is in many ways different from the other branches of physical rehabilitation. Current evidence of TR in neurological conditions is scarce in our country. Research is needed to determine the requisite skills and qualities of neurorehabilitation providers using TR, assessments, interventions, strategies and techniques that can be effectively delivered through TR, as well as optimal technologies for the delivery of neurorehabilitation services using TR.
• TR is not suggested to replace available face-to-face clinical services, but rather to provide access to specific disciplines or specialized providers not available within a community due to time, distance and cost related barriers. As TR services continue to grow as a complement to traditional face-to-face clinical services, there is an increasing need to standardize appropriate clinical uses, reimbursement, and health care policy regarding the use of TR. TR is a new and emerging way to deliver Physiotherapy in a remote fashion and evidence is still needed to support clinical and policy decision making.
In this global pandemic scenario, there is a paradigm shift towards an increasing need and use of TR; and is an extremely relevant area for Physiotherapy practice. With greater understanding, of the ways to promote its growth in use and acceptance, through this study we aimed to provide therapeutic support in the context of COVID-19
Study type
Clinical trial
Study design
Prospective quasi-experimental (pre-post design).
Study setting
Physiotherapy department of a tertiary care hospital.
Study duration
May 2020 to December 2020 This trial was conducted prior to the changes in public health directives that allowed for a gradual return to in-person care.
Intervention
TR service was provided by a physiotherapist as clinical consultation. Each session was provided on one-to one basis; customized, tailored to individual child needs; with real time, interactive medium of technology; and one or many sessions as appropriate.
Participants
The target population entitled to receive TR included all the patients diagnosed with developmental delay or disability such as cerebral palsy, spinal cord disorders, any other infectious, traumatic or genetic neurological conditions, etc.; and referred for Physiotherapy assessment and/or intervention. This also included children diagnosed as ‘at-risk for developmental delay’ and children who are self-referred.
Participants were recruited with a convenient sampling technique. Pre-registered patients were contacted through telephone and their willingness for and feasibility to participate in TR was determined. Newly referred patients were similarly enquired and enrolled for TR. Any patient/caregiver not willing to participate, not having adequate access to devices or tele-facilities was excluded from TR.
Procedure
Approval for the study was obtained from the Institutional Review Board. This clinical trial was designed according to the latest guidelines on pragmatic trials, using the gold-standard CONSORT guidelines and the telerehabilitation conceptual framework as evident in the literature. Also, guidelines were derived from the established physiotherapy protocol of the hospital. (Figure 1)
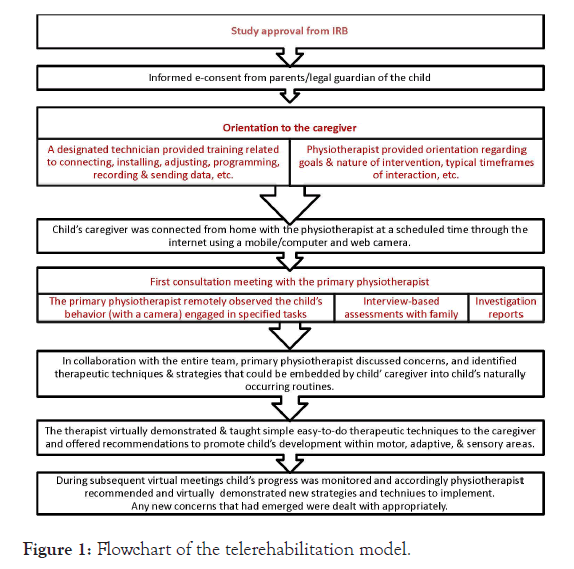
Figure 1: Flowchart of the telerehabilitation model.
Children were enrolled in the study following informed consent by their parent or guardian and participant’s assent (wherever applicable). Informed consent included permission to record the child’s videos during the session.
For the child a primary caregiver was identified but the whole family had the access to the TR intervention. The procedure of TR including orientation to technological tools was provided to the primary caregiver. A designated technician provided training related to connecting, installing, adjusting, programming, recording and sending data, etc. Physiotherapist provided orientation regarding goals and nature of intervention, typical timeframes of interaction, etc.
Child’s caregiver was connected from home with the physiotherapist at a scheduled time through the internet using a mobile or computer and web camera.
During first consultation meeting, the primary physiotherapist remotely observed the child’s behavior (with a camera) engaged in specified tasks. This information was supplemented by interviewbased assessments with family and any investigation reports, if available.
In collaboration with the entire team, primary physiotherapist discussed concerns and identified therapeutic techniques and strategies that could be embedded by child’ caregiver into child’s naturally occurring routines. The therapist virtually demonstrated and taught simple easy-to-do therapeutic techniques to the caregiver and offered recommendations to promote child’s development within the motor, adaptive, and sensory areas. During subsequent virtual meetings, child’s progress was monitored and accordingly physiotherapist recommended and virtually demonstrated new strategies and techniques for child’s caregiver to implement. Any new concerns that had emerged were dealt with appropriately.
Minimum one session per week and then further session/s on a family-identified needs-basis and flexible access as per parent needs were conducted.
This primary TR model planned to include occasional travel requirements for families and providers for direct hands-on assessment and training by the experts.
A time-log of virtual meetings and periodic monitoring of child’s clinical findings were maintained.
Resources
Personnel: Providers of this delivery model were the pediatric neurophysiotherapists of K J Somaiya college of Physiotherapy, India. These physiotherapists were already trained and experienced in assessment and management of pediatric neurological conditions. Additional training was provided by the chief investigator for orientation to TR related to its specific therapeutic and technical aspects. Technical help was taken as and when appropriate from the designated engineer.
Interdisciplinary model: Physiotherapy discipline-specific interdisciplinary model was employed. In this teaming model, providers worked towards shared outcomes incorporating elements such as more frequent formal and informal communication between providers and utilization of “cotreatments” for collaboration among providers. Assessment and child outcomes were functional and integrated across multiple domains. Primary service provider took lead in implementation of plan and worked with family/child on discipline-specific outcomes.
Consultative service delivery model: Through remote consultation, TR aimed to build capacity among caregivers and promote family-centered services. The nature of this consultation involved assessment, monitoring, therapeutic care and home-based activities. This model focused interventions toward the child’s caregivers to transfer knowledge and skills that will support the child’s development including any direct hands-on interventions by the caregivers. Using the technique of coaching within a consultative model, the Physiotherapist incorporated both “hands-on” and “hands-off” intervention; and used direct service for assessment and modeling of therapeutic techniques and instructional methods to promote the child’s skill development. Physiotherapist advised the parents to become experts and worked together with them to identify learning opportunities within a child’s natural environments; taught therapeutic techniques to embed within daily routines; collaboratively problem-solved, coordinated care, and identified community and family resources. Consultative services were used to enhance a caregiver’s capacity to embed learning opportunities throughout a child’s naturally occurring routines to promote skill development and generalization of skills across environments. In essence, the intervention concentrated on strategies designed to effect functional improvement.
Family-centered services: Physiotherapy goals reflected the needs and priorities identified by the family, and physiotherapists would work with families as partners towards shared goals.
Setting: TR services were provided within a child’s natural environment or “settings that are natural or normal for the child’s age peers who have no disabilities” such as the home or community settings with no travel necessary for families.
Equipment
a) Mobile videoconferencing that uses a cell phone with videoconferencing capabilities to transmit audio and video over a Wi-Fi or cellular network was used. Where available, cell phones were tethered to a laptop computer and served as a modem for internet-based videoconferencing. High-speed internet connectivity was desirable. Ideally, the device with the facility to zoom the camera so as to observe the child’ close-up as well as at a distance within his/her environment was preferred.
b) While deciding the mode of delivery, minimal infrastructure requirements, and lower costs for equipment and connectivity was taken into consideration. Initial investment was required for the purchase of equipment; professional training; production of technological resources and later for the maintenance and technological upgrades.
c) The best technology option was decided for the individual child by considering the available devices and facility within the home environment of the child (e.g., residential service plan); and also digital capabilities of the caregiver.
d) Aids required for therapy were used as available with the child at home.
Instruments: Parents/caregiver reported behavioral scales as per the child’s clinical condition were used to determine the clinical outcomes. Standardized; and easy to administer (with minimum training requirement) scales were used.
Outcome indicators: This was a descriptive study using a mixed qualitative and quantitative design. A semi-structured proforma (appendix 1) was developed that included open and closed ended questions around a guiding framework to facilitate data collection. Questions were designed to gather information about the
1. Timely receipt of physiotherapy services calculated as percentage of eligible children with neurorehabilitation needs for whom an evaluation and assessment; and TR meetings are conducted in a timely manner.
2. Child’s clinical outcomes assessed as ‘acquisition of developmental skills’ and ‘the use of appropriate functional behaviors to meet their needs’. This was determined from direct/ virtual observation by the primary physiotherapist; and parents reported behaviors and questionnaires (customized as per the child’s clinical condition).
3. Family’s acceptability and satisfaction with the provision of TR services.
Data analysis
Descriptive statistics including percentage and frequency distribution was performed for demographic characteristics (Table 1) and responses for closed-ended questions (frequency and type of TR consultation) (Tables 2&3). Qualitative observations were performed for comparative analysis on child’s clinical outcomes pre and post TR. Thematic analysis was performed for open ended questions.
| Characteristic | Mean | SD |
|---|---|---|
| Age (in years) | 3.02 | 2.1 |
| Gender | Male | Female |
| 11 (52.3%) | 10(47.6%) | |
| Primary caregiver | Mother | Other |
| 20(95.2%) | 1(4.8%) (both parents) | |
| Clinical condition | Cerebral Palsy | Other |
| 18(85.71%) | 1(4.8%) (DMD), 3(14.28%) (at risk of developmental delay) | |
| Enrollment | Pre-registered | Newly referred |
| 20(95.2%) | 1(4.8%) |
Table 1: Demographic characteristics of the children and caregivers
| Number of sessions | Preliminarysession | Completed 5 sessions | Ongoing | Discontinued |
|---|---|---|---|---|
| n=38 | 14(66.6%) | 14(66.6%) | 7(33.3%) | |
| Nature of consultation | Enquiry for TRÂ | Assessment | Monitoring | Therapy |
| n=38 | 27(71%) | 21(55.2%) | 19(50%) |
Table 2: Time log of virtual consultation
| Sr. No. | Facilitators | Barriers |
|---|---|---|
| 1 | Availability of internet | Primary caregiver is mother and has a dual responsibility of domestic work and child care |
| 2 | Availability of smartphones | Time coordination issues between mother’s domestic work and child’s sleep-wake cycle |
| 3 | Minimum therapy charges | Child falling sick more often (lack of regular medical follow-up) |
| Â 4Â Â Â Â Â | No travel requirements | Relocated to a village (network issues) |
| 5 | Minimum investment of resources | Unavailability of device (only one cell phone with working father) |
| 6 | Lack of technical skills of the caregiver |
Table 3: Feasibility of TR
The face of neurorehabilitation has changed rapidly as the lockdown and public restrictions are imposed since the outbreak of COVID-19. A number of telerehabilitation approaches emerged in various places each with their own rationale and strategies which will influence our practice in the coming years and have lasting effects on the field. Along with the great diversity in TR practices, the fact that TR is currently understudied in children supports the need of the current study. The overarching goal of this study was to assess the feasibility and outcome of adoption of TR in the delivery of pediatric neurophysiotherapy during the changing practice environment.
Previously, telemedicine/rehabilitation functioned as an adjunct to traditional in-person healthcare access. In the era of COVID-19 and beyond, telemedicine can no longer be considered as a ‘complement’ to in person care; rather, it should be viewed as an ‘alternative’ to in-person care. Now, all issues related to TR must be revisited and viewed through a new perspective with TR currently being the primary means and likely to remain a highly relevant means because its use is likely to be sustained at a much higher rate post-COVID-19 even as traditional in person healthcare visits resume.
Modernization of health-care related treatments and service paralleled by evolution of technology has been a great support for healthcare professionals. Through video conferencing facility it is possible to visually and verbally connect on one to one basis in real time; and to effectively communicate and treat a variety of patient groups. This technology-based practice is an extremely relevant area for physiotherapists offering new possibilities for discovering and implementing optimized intervention strategies. Due to easy availability of smartphones and internet connectivity, TR can be viewed as an enabler of change because of its high reach and lowcost solution. However, in developing countries many challenges are still being faced in terms of provision and accessibility to stable technology such as inadequate and underdeveloped infrastructure; caregivers’ digital literacy; cultural issues, and financial implications which are also evident in the present study [22,23]. With regards to feasibility, the most common issues faced during TR sessions were technical such as unavailability of a device (only one cell phone available with working father; unavailability of smartphone, etc.); network issue; lack of technical skills of the caregiver; and also, family relocated to a village (network issues), etc. Considering that majoritily this sample of parents represents uneducated people, digital health literacy is an important factor along with the supports and resources needed to euip them that would impact the effective implementation of TR; and to have a satisfactory experience with TR. Currently providers were not able to address the accessibility issues with their patients even if the system was designed correctly. These factors can be implicated to hinder successful implementation of TR and are similar to those reported in other developing countries.
Access to healthcare is a significant metric for healthcare outcomes [24]. Out of the 38 patients who enquired for physiotherapy services, 66.6% of children received PT through TR during the pandemic lockdown. Our healthcare institution is an academic institution; and facilities depend greatly on graduate medical trainees. Prior to this pandemic, TR was not integrated into the routine healthcare delivery. Also, no awareness campaign or digital marketing of TR service was done to promote participation of patients in this new service model. This could have significantly impacted the access to TR for populations who often rely on traditional in-person healthcare. With TR now being the primary- and often only-means of access, these barriers must be systematically addressed and new solutions for maintaining and improving healthcare equity delivered via TR need to be in place.
The key aspects of this TR intervention program tended to target parents, used a coaching approach, focused on improving children’s behavioral functioning and were offered at least once a week. The therapeutic activities performed with the children emphasized various neuro-developmental facilitation approaches delivered by the caregiver. This is consistent with the recommended components of therapeutic plan for children with neurological conditions. Additionally to minimize the barriers and optimize care, a family-centered approach which includes families in setting goals and selecting interventions was advocated. In essence, parents became an active partner in their child’s therapeutic care and also reported enhanced parenting skills.
During the COVID-19 lockdown, TR strategy aimed to reduce gaps in access to healthcare service and enabled therapists to remotely engage and deliver patient care outside of the medical setting, thus eliminating the issue of distance between therapist and patient. Along with ensuring continuity of care, this opportunity to provide rehabilitation within the patient’s own social and cultural environment should lead to greater functional outcomes. Qualitative observations about children’s clinical outcomes showed improvement reported as ‘acquisition of developmental skills’ and ‘the use of appropriate functional behaviors to meet their needs’.
Research has also found that TR cuts down the associated costs and time spent traveling; and also reduces the risk of exposure to communicable diseases especially during a pandemic. This outcome of TR, though reported in the literature is not analyzed in the present study.
However, some challenges exist in this emerging field of TR. Parents articulated barriers they experienced in accessing therapeutic care via telerehabilitation. This insight additionally stresses the importance of recognition of factors unique to pediatric population.
Parents noted a desire for more therapy sessions for their children but described barriers to obtaining appropriate services that were internal or external to the family unit. Barriers internal to the family unit emerged from both the parents and the child. In responding to open-ended questions, the most frequent challenge reported was lack of time with the mother. Primary caregiver was mother and has a dual responsibility of domestic work and child care. Time coordination issues between mothers’s domestic work and child’s sleep-wake cycle, in particular was a challenge. Also, due to lack of regular medical follow-up in this current pandemic situation, children were falling sick more often and this too resulted into cancellation of scheduled appointments.
These children were previously receiving a home exercise program as a component of the intervention or sometimes the main mode of intervention. Although, the majority of the parents reported their children were supposed to be performing Home Exercise Program (HEP), most identified a number of internal barriers preventing consistent follow-through on the recommended protocol. Parents reported that follow-through and adherence were both challenging and burdensome. While well intentioned, parents reported they often did not have time or were simply too tired to participate in the child’s therapy session. The reasons given for non-adherence varied from time constraints to fatigue and medical illness on the part of the child. This finding is consistent with previous research reporting low HEP adherence among caregivers of children with disabilities and that 50% of parents likely do not adhere with prescribed therapeutic regimes [25,26].
Family centered care has become the most commonly used model of care around which to structure parents’ involvement in their child’s health care in both developed and developing countries [27]. However, therapeutic non-compliance in the home-based settings has been associated with underutilization of therapeutic services and needs to be addressed through greater understanding and discussions with parents. While providing therapeutic care, therapists also suggested ways to overcome some of the barriers parents experienced while better integrating the needs and challenges of the families and children into the development of the plan of care.
Parents’ perceptions of the usefulness of TR: Parents reported that physical therapy with TR employed during lock down has been fundamental in their child’s progress; it is motivating; and has been essential and an alternative to face-to-face outpatient service. Families show satisfaction with TR services; however, expressed initial hesitancy questioning the effectiveness of TR and the need for in-person sessions. It is not entirely unexpected that there would be concerns about TR, mainly as it eliminates physical contact which is an integral part of physiotherapy practice in general and a fundamental need for pediatric neurophysiotherapy in particular. As noted in the responses, parents perception of TR is another key consideration that would impact implementation, especially perception of effectiveness. TR is not simply a matter of moving to a new platform; it requires a cultural transformation in how the parents view physiotherapy- a profession traditionally viewed as being hands on and physical. Families of children with neurotherapeutic needs have extensive experience with the healthcare community that may affect their expectations [28]. Expectations of healthcare communities accumulate from one visit to the next. This sample of children had taken regular therapeutic and multidisciplinary services in person prior to telerehabilitation. They felt disadvantaged in providing the level of care they are familiar with by being unable to do hands-on manual assessment and treatment. This further reinforces the need for physiotherapists to recognize parents’ perceptions about TR. Therefore, expectations of TR services and goals for the child need to be discussed with all parents to form an appropriate plan of care. Overlooking these important steps could lead to poor quality of care, poor sustainability, inadequate satisfaction from parents and professionals.
To summarize, the present study provides preliminary evidence on the feasibility and utility of TR as a new service delivery model for pediatric neurophysiotherapy. Its benefits and impact, limitations, barriers and needs, and recommendations for the current and future adoption of TR services with a concentration in evidence-based pediatric neurophysiotherapy are discussed. Although several reviews have examined the historical use and effects of telehealth, to the best of our knowledge, this is the first published study which reports its current status in the pandemic situation and in an understudied population. Another important highlight of the study is homogeneity of the sample with respect to clinical condition and socioeconomic status. However, we acknowledge small sample size as the major limitation of the study. Also given the inherent limitation of distance in TR mode, clinical outcomes could be determined only through qualitative observations and not by objective measurement tools. Another consideration is that the study analysis was completed within the lockdown period itself. Given the recency of this situation, the long term outcomes as well as those outcomes which cannot be assessed online could not be a part of this study’s findings.
Certainly, telerehabilitation holds promising potentials and success for the rehabilitation of children with neurological conditions. In the current scenario, TR enhances the capacity of families to meet the needs of their child with a disability by connecting them with health care providers, resources and supports, thus ensuring continuity of care. While guidelines to tackle this unprecedented situation continue to develop, TR demonstrates the potential as an alternative rehabilitation strategy thereby ameliorating the impact of social distancing on underprivileged children. However, challenges exist on how TR can bridge a gap between physical contact needed for certain assessments and interventions by the physiotherapists; and also, some psychosocial factors act as barriers to feasibility of TR in pediatric population.
Implications for clinical practice: The findings may enable therapists to develop more effective plans of telehealth and telecare that take into consideration the context within which the child and family exist. Additionally therapists should employ strategies to improve adherence to home exercise programs such as embedding programs in the social contexts of the child and family. It is clear that with the recent advancement in technology, and the increasing availability of low-cost platforms for telerehabilitation services the field will continue to expand in the future. The combination of evidence-based methodologies with cost-effective services will serve as a basis for further expansion of vital telerehabilitation services and increase utility and perceived effectiveness of the therapy delivered via TR, may also increase reimbursement by health insurance providers. Government highlights for our way forward, we need to improve sustainability and value by establishing a baseline, and developing consistent outcome measures and indicators to track the impact of telerehabilitation on working practices, productivity and resource use.
Implications for research: More clinical studies are required to elucidate full utility of TR at different levels and in different parts of the country. Research is needed to determine the requisite skills and qualities of neurorehabilitation providers using TR; assessments, interventions, strategies and techniques that can be effectively delivered through TR; as well as optimal technologies for the delivery of neurorehabilitation services using TR. Future research is required to better understand the characteristics of effective TR interventions specific to pediatric population and with an emphasis on clinical outcomes and cost-effectiveness. In uncertain times and need for social distancing, implementation of TR sevices is spiking in healthcare. However, speeding up implementation of this new modelof care and cutting corners due to urgency is nor recommended. We must research and be diligent. The future threads to this discussion will be interesting to follow. (add this as a seperate paragraph)
Authors declare that there are no conflicts of interest.
No funding is received for the conduct or publication of this study.
Questionnaires, e-consent form and database of the participants is available from the corresponding author upon request.
Authors acknowledge the children, their caregivers and the therapists for their valuable participation; and the principal and research committee of K J Somaiya college of Physiotherapy for their support in the conduct of the study.
Citation: Akulwar-Tajane I, Bhatt GD (2021) Telerehabilitation: An Alternative Service Delivery Model for Pediatric Neurorehabilitation Services at a Tertiary Care Center in India. Int J Phys Med Rehabil. 9.S4:001.
Received: 13-Jan-2021 Accepted: 27-Jan-2021 Published: 03-Feb-2021 , DOI: 10.35248/2329-9096.21.s4.001
Copyright: © 2021 Akulwar-Tajane I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited