Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Research Article - (2022)Volume 11, Issue 2
Background: Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) is a common disease in clinic of urology. Although the etiology of CP/CPPS is unclear, accumulating evidences reveals the central mechanisms like neuromodulation, neural plasticity and brain reorganization play a vital role in the pathophysiological mechanisms. As is acknowledged as a non-invasive and accurate instrument, resting-state Magnetic Resonance Imaging (MRI) has been applied to investigate brain abnormalities of structure.
Objective: The aim of this study is to assess the brain structural alterations in the patients of CP/CPPS evaluated by measuring the brain gray matters through MRI.
Materials and Methods: 50 patients of CP/CPPS and 50 matched healthy controls were recruited to scan T1- weighted MRI. Voxel-Based Morphometry (VBM) was applied to identify brain regions correlated with scores of clinical scales. Total Gray Matter Volume (GMV) and cortical thickness analysis were carried out.
Results: The positively altered regions of gray matter density were mainly concentrated in the cortical regions surrounding the basal ganglia and the lateral ventricles bilaterally while negative changes of gray matter density were mainly located in the gray matter areas of lateral cerebrum (P<0.05). The mean values of gray matter density in these abnormal regions correlated with the scores of clinical scales.
Conclusion: The patients of CP/CPPS had structural abnormalities in the pain modulation system. These alterations might trigger the pathogenesis and development of CP/CPPS.
Chronic prostatitis/chronic pelvic pain syndrome; Gray matter density; Voxel-based morphometry; Magnetic resonance imaging
Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) is a common male urogenital disease observed in clinical practice of urology [1]. The patients of CP/CPPS occupy a large proportion of population, occurring in approximately 50% of men at particular time point during their lifetime [2]. According to the definition of the National Institutes of Health (NIH), the typical clinical symptoms of CP/CPPS includes chronic pelvic pain symptoms persisting more than three months during the past six months without any other evident causes, along with the symptoms like lower urinary tract symptoms and/or sexual dysfunction [3]. It was estimated that only 5% to 10% of prostatitis patients have acute or chronic bacterial infection, whereas the majority of men with prostatitis (about 90%–95%) suffer from chronic pelvic pain without any evidence of infection [4]. Except causing chronic pain in various areas of the pelvis and genital, CP/CPPS constantly leads to negative cognitive, behavioral, sexual, emotional and psychiatric comorbidities like anxiety and depression, which substantially diminishing the quality of life [5,6]. CP/CPPS is also related with other functional somatic syndromes such as irritable bowel syndrome, interstitial cystitis, chronic fatigue syndrome and fibromyalgia.
The etiology of CP/CPPS is still indistinct. Accumulating studies proposed it should be multifactorial mechanisms like pathogen infection, neuroendocrine, immune function, oxidative stress and emotional factors getting involved in the pathogenesis of CP/CPPS [5-7]. Since current treatments concrete on clinical symptoms, the major therapeutic interventions for CP/CPPS include α-blockers, antibiotics, pain killers and replacement therapy [8]. Owing to the heterogeneity of CP/CPPS, there is no monotherapy containing both pharmacological and non-pharmacological treatment modalities competent to offer reliable benefits for patients of CP/CPPS [9]. Hence, CP/CPPS is becoming a controversial issue, and doubts have been raised concerning its clinical diagnosis and treatment [2].
Obviously, CP/CPPS is also a kind of chronic pain disorders. Human neuroimaging studies examining brain properties in patients with chronic pain have unequivocally established that different chronic pain conditions are associated with distinct brain properties [10]. It has been reported that there are specific patterns of functional, pain-related brain activation and anatomical brain reorganization in patients of CP/CPPS, which was thoroughly associated with clinical pain intensity [11]. Magnetic Resonance Imaging (MRI) evaluation intensely broadens our mind of the brain in the fields of both function and structure over the last decade. Voxel-Based Morphometry (VBM) is a volumetric technique by means of T1-weighted MRI scans to distinguish the structural differences in the level of voxel between matched sets [12]. With the application of this volumetric method, the whole brain could be analyzed by statistically comparing the grey matter volume or density in cortical and subcortical regions after data preprocessing [13]. Grey Matter Volume (GMV) is the product of cortical thickness and cortical surface area [14]. There were seldom studies mentioned the alterations in brain structure of the investigation of CP/CPPS.
In our preceding work, we found that the altered functional connectivity in the patients of CP/CPPS by analyzing the brain network in the resting-state [15]. We agreed with the theory that the pain of CP/CPPS had less association with the organ prostate whilst the origin of CP/CPPS should attribute to the alternations of the nerve system. Herein, we further hypothesized there should be central mechanisms like central neuromodulation and neural reorganization relevant to pathogenesis of CP/CPPS. To figure out the changes in the patients’ brains of CP/CPPS, we utilized the technique of T1-weighted MRI scans to investigate the alternations of neural structure in the CP/CPPS patients with spontaneous pelvic pain during resting-state. Mutual the scores of subjective clinical scales with the analysis of objective structural MRI data, we concluded the major alterations and their clinical significances of brain gray matters.
We collected a cohort consisting of 50 male right-handed patients of CP/CPPS and 50 healthy right-handed age and gender matched healthy controls (Table 1). The patients of CP/CPPS were directly recruited by oral inquiry and well-versed in our project’s aim and related consequence in the routine urological clinic of Huashan Hospital, Shanghai, China. The group of healthy controls was recruited through advertising. To reduce the potential impact of senile brain atrophy on structural brain imaging, only aged from 20 to 50 years volunteers were requested to enroll in [16]. The participants in the healthy control group denied any related symptoms like spontaneous pain, mental illness, and acute or chronic physical diseases. Corresponding to the characterization of CP/CPPS, this disease was diagnosed by excluding other illness sharing similar symptoms. Physical examinations, clinical scales, routine urine test regular microbiological cultures and microscopic analysis of urine, Tran’s Rectal Ultrasonography (TRUS) were applied in the procedures of diagnosis. The exclusive criteria included any acute or chronic infectious diseases, other chronic pain diseases, internal organic diseases, history of malignant tumors, and chronic diseases that might contribute to peripheral nerve injury like diabetes mellitus and hypertension. Moreover, if the volunteers had the contraindications to fMRI like installation of metal dentures which cannot be taken away, installation of pacemakers that cannot pass MRI examination, claustrophobia, and so on, they were also be eliminated. All the patients declared not take any medications for CP/CPPS before or stop taking the drugs to treat CP/CPPS for more than a month, and they denied the other discomforts at any other body parts. After attaining the written informed consent, all of the participants were requested to fill in one National Institutes of Health Chronic Prostatitis Symptom Index (NIH-CPSI) scale and one Hospital Anxiety and Depression Scale (HADS). The higher scores of NIH-CPSI scale reflected the worse prostatitis symptoms the patients were enduring, and the higher scores of HADS described the worse psychological states of the patients. NIH-CPSI scale contains a Numeric Rating Scale. For pain evaluation, the NRS is a segmented numeric version of the Visual Analog Scale (VAS) in which a respondent selects a whole number (0–10 integers) that revealed the intensity and severity of spontaneous pain [17].
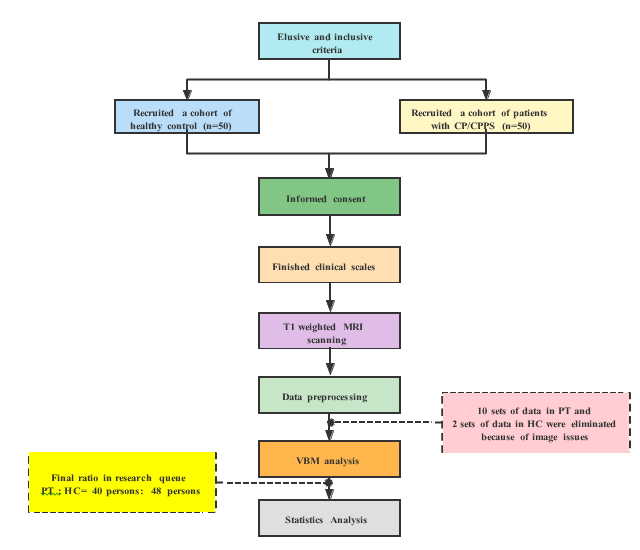
Figure 1: The flow chart of study design.
We originally recruited a cohort of healthy control (50 persons) and patients of CP/CPPS (50 persons). Nevertheless, after the procedure of data preprocessing, we examined the quality of images. As illustrated in the flow chart, owing to image distortion and invalid format, 10 sets of data in patient group and 2 sets of data in healthy control were unfortunately excluded, which affected on the final numbers of people engaged in each group. PT: patient group, HC: healthy control.
The data acquisition of resting-state T1 weighted MRIThe resting-state T1 Weighted MRI data were attained by using a 3.0 T MRI scanner (MR750, GE Healthcare, and Waukesha, WI, USA) with an eight-channel phase array head coil at the Jingan District Centre Hospital, Shanghai. First of all, localization sequence was employed in our study. The localization sequence was the Spin Echo (SE) sequence T1-weighted sequence in the sagittal position. The detailed parameters included: Repetition Time (TR)=440 ms, Echo Time (TE)=11 ms, slice thickness=6 mm, Field Of View (FOV)=24 × 24 cm2, matrix size=256 × 192. The acquisition of structural image data took the middle layer of the positioning sequence as the reference. The slices were adjusted to be parallel to the AC-PC line as the structural scanning. T1-weighted three-dimensional volumetric spoiled gradient echo (SPGR) categorize the separate participants, it was feasible for the authors to approach the personal information during or after data collection.
The data analysis of preprocessing and VBMMRI convert was applied to convert all the DICOM files in format to NIFTI files. The whole-brain VBM approach was performed in VBM8 toolbox to analyze the GMV based on SPM12 [18]. To preprocess the T1-weighted MRI data, tissue segmentation and normalization by using a custom template generated with the DARTEL Toolbox were the main steps [19]. The normalized gray and white matter segmented images were modulated in non-linear only and smoothed by using a Gaussian kernel with a FWHM of 8 mm. All segmentations were visually inspected prior to analysis. 10 sets of data in patient group and 2 sets of data in healthy control were eliminated because of image distortion and invalid format. Thus, there were 40 sets of patient group’s vs 48 sets of healthy control available in the patient group, eventually. All the exact volume data of gray matter, white matter and Cerebra Spinal Fluid (CSF) were well recorded to analyze. The abnormal brain regions of gray matter density were divided into increased areas and decreased areas. Subsequently, we extracted the mean gray matter density of both increased areas and decreased areas. Linear regression was used to validate the correction of the scores of clinical scales and the values of abnormal brain regions.
Statistics analysisA two-sample t-test was conducted based on the measurement data (age, duration of illness, NRS scores, NIH-CPSI scores, and HADS scores) by SPSS 17.0, and results were scheduled as ̅ ± S (Table 1). A two-sample t-test was conducted after VBM analysis. Family Wise Error(FWE), as multiple comparison correction, corrected the values of gray matter density (voxel p<0.01, cluster p<0.01). The statistical images were superimposed on the standard spatial template for presentation. Active clusters larger than 20 voxels were demonstrated on the calibrated standard brain map with pseudo-color, and their MNI coordinates, positions, and voxel sizes of peak intensity were listed in a table by Xj View 95 software in the Table 2. A two-sample t-test was conducted to compare the exact volume data of gray matter, white matter and cerebrospinal fluid. Significant difference was set at P<0.05. Linear regression analysis was conducted with SPSS 11.0 as dependent variables to the scores of clinical scales and the mean values of abnormal brain regions. The significant difference was set at P<0.05. The outcomes of linear regression analysis were displayed by GraphPad 8.0.
We recruited an observational cohort involved in 100 male, right-handed, and age-matched participants (P=0.6423) as shown in Figure 1. In the patient cohort (Table 1), the mean duration of disease was approximately 23 months which was consistent with the definition of chronic pain. In order to reduce the possible influence caused by senile brain atrophy, we limited the age of the participants from 20 to 50 years old. The total scores of the NIH-CPSI indicated the cohort of patients suffered from this illness deeply because the total score above 18 reveals the severe situation of CP/CPPS. The scores of NRS contained in the NIH-CPSI were 5.22 ± 2.22, which described the patients met with the extent of pain in mild to moderate when CP/CPPS attacked. Meanwhile, we also utilized the NRS to exclude the possibility of spontaneous pain in the applicants of healthy cohort. Since it was acknowledged to all that the scores of HADS subscale would not be significant unless the score was over 7, the major psychological characteristics of the participated patients was anxiety, of which the subscale scores were 9.15 ± 4.40. Although the scores of HADS depression subscale (6.17 ± 4.14) were not more than the threshold of 7, we should continue to follow up the patients’ condition of illness. Hence, this study further concentrated on the emotional symptom of anxiety rather than depression in patients of CP/CPPS.
Table 1: The features of participants.
| CP/CPPS patients (n=40) |
Healthy control (n=48) |
P value |
|
|---|---|---|---|
| Gender | Male | Male | - |
| Age/years | 36.63 ± 10.63 | 38.63 ± 11.05 | 0.6423 |
| Duration of disease/months | 23.53 ± 7.56 | 0 | <0.001 |
| NIH-CPSI score (1+2+3+4+5+6+7+8+9) | 29.44 ± 10.76 | 0 | <0.001 |
| Pain and discomforts (1+2+3+4) | 15.83 ± 7.25 | 0 | <0.001 |
| NRS (4) | 5.22 ± 2.22 | 0 | <0.001 |
| Lower urinary tract symptoms (5+6) | 4.66 ± 3.31 | 0 | <0.001 |
| Impact on quality of life (7+8+9) | 9.15 ± 2.71 | 0 | <0.001 |
| Severity of symptoms (1+2+3+4+5+6) | 20.49 ± 8.75 | 0 | <0.001 |
| HADS (anxiety) | 9.15 ± 4.40 | 0 | <0.001 |
| HADS (depression) | 6.17 ± 4.14 | 0 | <0.001 |
| HADS (total) | 15.32 ± 7.99 | 0 | <0.001 |
The Abnormal Brain Regions by the Analysis of VBM The detailed anatomical location of the abnormal brain regions was demonstrated in Table 2 and Figure 2. The positively altered regions of gray matter density were mainly compound of left and right postcentral gyrus, right putamen, left pallidum, left temporal mid gyrus, left temporal superior gyrus, right calcarine, left thalamus, left lingual gyrus, right thalamus and so on, which concentrated in the cortical regions surrounding the basal ganglia and the lateral ventricles bilaterally. Meanwhile, there were also some areas of gray matter presenting negative changes of gray matter density, containing right temporal mid gyrus, right angular gyrus, right occipital mid gyrus, left occipital mid gyrus, right frontal inferior lobe, right precentral gyrus, left and right thalamus, left and right frontal superior lobe, right frontal mid lobe, and so on, which were located in the gray matter areas of lateral cerebrum.
Regions in yellow to red represented the areas of general increase in gray matter density whilst blue to green areas indicated lower gray matter density. PT: patient group, HC: healthy control.
Table 2: The detailed anatomical location of the abnormal brain regions.
| Region Label |
Cluster/voxels |
Peak t-value |
MNI Coordinates |
|||
|---|---|---|---|---|---|---|
| x | y | z | ||||
| Positive | Postcentral_L | 190 | 7.483 | -33 | -26 | 44 |
| Putamen_R | 842 | 7.347 | 29 | -11 | 14 | |
| Pallidum_L | 403 | 7.062 | -23 | -11 | -3 | |
| Temporal_Mid_L | 235 | 7.035 | -38 | 5 | -29 | |
| Temporal_Sup_L | 123 | 6.777 | -44 | -6 | -15 | |
| Calcarine_R | 573 | 6.657 | 15 | -77 | 18 | |
| Thalamus_L | 164 | 6.551 | -11 | -12 | 0 | |
| Lingual_L | 111 | 6.367 | -15 | -77 | 2 | |
| Postcentral_R | 193 | 6.252 | 32 | -26 | 47 | |
| Negative | Temporal_Mid_R | 7361 | -11.123 | 63 | -42 | 11 |
| Angular_R | 7361 | -10.549 | 56 | -57 | 33 | |
| Occipital_Mid_R | 7361 | -8.275 | 38 | -81 | 26 | |
| Temporal_Mid_L | 9397 | -10.684 | -62 | -50 | 11 | |
| Angular_L | 9397 | -10.166 | -53 | -62 | 26 | |
| Occipital_Mid_L | 9397 | -8.586 | -44 | -80 | 27 | |
| Frontal_Inf_Tri_R | 1259 | -8.202 | 51 | 44 | 0 | |
| Frontal_Inf_Tri_R | 1259 | -7.454 | 57 | 24 | 9 | |
| Precentral_R | 1259 | -6.732 | 56 | 8 | 39 | |
| Thalamus_R | 1404 | -6.73 | 2 | -14 | 11 | |
| Thalamus_L | 1404 | -6.544 | -12 | -29 | 12 | |
| Frontal_Sup_2_L | 110 | -6.399 | -26 | 63 | -8 | |
| Frontal_Mid_2_R | 144 | -6.285 | 41 | 41 | 35 | |
| Frontal_Mid_2_R | 144 | -5.958 | 39 | 54 | 17 | |
| Frontal_Sup_2_R | 141 | -6.211 | 24 | -11 | 72 | |
The Alterations of Gray Matter Volumes We extracted the related parameters of gray matter volumes in both healthy control and patients of CP/CPPS. Several aspects of factors may result in the alterations of g normalized gray matter or white matter or Cerebro Spinal Fluid (CSF) volume, including blood flow, cell size, synaptic densities, interstitial fluid and so on. There were no significant differences in normalized gray matter or white matter or Cerebro Spinal Fluid (CSF) volume. Nevertheless, as the combination of gray matter volume, white matter volume and Cerebro Spinal Fluid (CSF) volume, the difference of TIV in this study might reveal the heterogeneity of participants. The Total Intracranial Volume (TIV) between two group revealed a significant difference (P<0.01). The mean TIV in the patient group was 1500.75 ± 129.57 mL whilst the mean TIV in the healthy control was 1601.75 ± 166.98 mL.
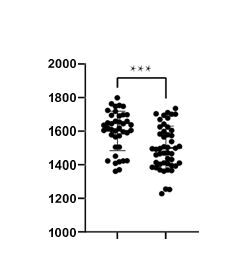
Figure 2: Comparison of tiv between the groups of pt and hc (p<0.01). Pt: patient group, hc: healthy control.
The Correlation of Abnormal Brain Regions and Clinical Scale Scores the mean values of increasing gray matter density revealed a positive correlation to the total scores of NIH-CPSI (r=0.3935, P<0.05), which revealed these regions played a particular role in the exacerbation of prostatitis-like symptoms. Since the mean values of decreasing gray matter density were taken as absolute mean value in order to demonstrate the values in the same coordinate system, the mean values of decreasing gray matter density should be recognized as negative correlation to the total scores of NIH-CPSI (r=0.3219, P<0.05). As these involved brain areas were thought to function in the modulation and inhibition of pain, the correlation indicated the loss control of pain might also cause the complex somatic symptoms of CP/CPPS. Correspondingly, the mean values of decreasing gray matter density also indicated negative correlation to the scores of HADS anxiety subscale (r=0.3190, P<0.05). Some sub regions of the negatively abnormal brain areas like and thalamus also respond to emotional regulation, so their dysfunction could arouse anxiety tendency of patients. The mean values of increasing gray matter density were positively correlated with the score of HADS anxiety subscale (r=0.3139, P<0.05). These activated areas like basal ganglia and frontal lobe are associated with anxiety, consistent with our outcomes. The scores of HADS subscale would not be convincing unless the scores were over 7. The scores of HADS depression subscale were not involved in the correlation analysis.
CP/CPPS is a common type of male urological condition, affecting 5%–10% of male population, accompanied by obscure pathogenesis, lack of effective therapies, and significantly social burden [20]. Accumulating evidences revealed CP/CPPS may be connected to the altered brain activity and excitability, and brain neuroplasticity participated in the pain modulation of CP/CPPS [21-23]. Neuroplasticity is an essential property of all sensory systems throughout the brain, which is a neural activity induced by long-term changes to neuronal circuits through recurrent experiences [24]. Central sensitization is a phenomenon of synaptic plasticity and increased neuronal responsiveness in central pain pathways after painful stimulation, and it is the consequence of physiological neuroplasticity [25]. Synaptic plasticity could sensitize the central nociceptive system, triggering hyperalgesia and chronic pain [26]. Thus, chronic pain is directly related with brain’s functional and structural changes reflecting neuroplasticity, which contains the structure of thalamus, midbrain, and extensive areas of cerebral cortex [27]. As demonstrated, most of abnormal regions involved in the primary somatosensory (S1) cortex, secondary somatosensory (S2) cortex, thalamus, cingulated gyrus, Peri Aqueductal Gray (PAG) and frontal lobe, are the members of the “pain matrix “which are recognized as areas related with the perception of pain [26]. There was increased gray matter density in the S1 cortex in comparison of healthy control. Among the patients of migraine, chronic low back pain and chronic headache, it was also found that patients had greater cortical thickness and increased connectivity at S1 cortex compared to the control group [28-30]. As an essential sensory processing region, the S1 cortex not only dominates the perception of pain, comprising discrimination and localization, but also gets involved in peripheral-stimulation-induced neuronal activities in downstream brain regions associated with pain signals [31]. Individuals with larger S1 cortex tends to present hypersensitivity to pain [32]. However, whether larger S1 cortex is the cause or consequence in the pathogenesis of CP/CPPS still needs further investigation. By contrast, the decreased gray matter density in the S2 cortex was found in this study. In the other chronic pain disorders like Central Post Stroke Pain (CPSP) and Classic Trigeminal Neuralgia (CTN), the same phenomenon was also found [33,34]. S2 cortex gets involved in the sensory-discriminative dimension perceiving the sense of intensity, quality, location, and duration of pain [35]. When the input sensory nerve function changes, the activity of the sensory-discriminative dimension is upregulated or downregulated to adapt to the altered signals in order to suppress pain [35,36]. This could be interpreted as advanced neuroplasticity compensation for pain impression with its negative influences on the individual patients rather than a simple response to a specific stimulus [37]. The regions of decreasing gray matter also contained bilateral thalamus, representative the responsibility of the thalamus in chronicity of CP/CPPS. The thalamus is a key region in the modulation of nociceptive information through the pain transmission pathway [38]. Thus, the thalamus is acknowledged to be associated with spontaneous and evoked pain in chronic conditions like diabetic painful neuropathy and chronic low back pain [39,40]. In the animal model of Post-Traumatic Stress Disorder (PTSD), the significant brain atrophy was detected in the bilateral thalamus, suggesting severe stress may affect the pain threshold [41]. The paraventricular nucleus of the thalamus was proved to integrate cortical and hypothalamic signals to modulate the behavioral responses associated with anxiety [42]. This enlightened the decreasing gray matter regions of bilateral thalamus might be a cause of arousing the anxiety in the patients of CP/CPPS. The regions of decreasing gray matter got involved in the PAG. The PAG is an essential modulator of pain involved in endogenous pain inhibition and facilitation which is supposed to be functional in fear and pain perception [43]. PAG could mediate pain control through its ant nociceptive endogenous opioid and non-opioid, so PAG has a general contribution to the pathogenesis of various disease states, including anxiety and depression except for chronic pain [44]. In many other chronic pain diseases like chronic lower back pain, irritable bowel syndrome and fibromyalgia syndrome, lower activated PAG or its disruption of descending pain modulation were found to play a vital role in their pathophysiology [27,45,46]. As an important part of decreased gray matter density areas in this study, the dysfunction of PAG might have an imperative impact on the promotion of somatic symptoms and psychological
Changes in the patients of CP/CPPS. Nevertheless, the PAG is advised to be separated into sub regions (ventrolateral, dorsolateral, and lateral) that are specifically responsible for differentiated functions including anxiety, pain, autonomic nervous system, sexual behavior, and analgesia [47]. It should be meaningful to further investigate the accurate anatomical and cellular mechanism in the development of CP/CPPS. In this research, we also exhibited an enlarged gray matter density of right putamen, suggesting the character of the basal ganglia in patients of CP/CPPS. The deep gray matter basal ganglia are vital in functions of integrating motivation, sensory, motor, cognitive and procedural learning [48]. Putamen critically responds to anticipation of reward [49]. Larger gray matter volume in right putamen was also observed in the patients of Social Anxiety Disorder (SAD) [50]. Anticipation of social punishment versus reward was correlated with greater putamen activation in the patients of SAD compared to healthy controls [51]. It might be because larger caudate was related with increased functional connectivity to regions that functions social stimuli, and it might facilitate the saliency of social for individuals with an inhibited temperament, which could promote them into SAD [52]. Intriguingly, it was consistent with anxiety which was the psychological characteristics of patient group in this study. The potential mechanism of brain reorganization in the CP/CPPS is indistinct, but it is might be interrelated to the number and size of neuronal or glial cells and their synapses, altered interstitial fluids, blood flow probably or a combination of these, attributing to the alterations of neural excitability, vascular constriction or dilation, and neural degeneration. Moreover, pain-induced alterations in the brain varies from the duration of pain, with increased gray matter volume and amplified connectivity in initial periods of chronic pain prior to decreased gray matter volume with high persistence and greater intensity of chronic pain [53]. Following up is needed to observe the alterations of brain structure and emotion in the course of the disease.
Although chronic pain is associated with reduced gray matter volume in many cortical and subcortical brain regions, there is increasing evidence that these structural alterations are partially reversed as pain is alleviated through drug intervention or spontaneous relief, such as chronic back pain and post-traumatic headache [54-56]. Other studies have found that decreased gray matter volume in fibromyalgia patients is related to decreased water content, not nerve loss [57]. Based on the above findings, it revealed that for CP/CPPS patients with changes in gray matter density or gray matter volume, only “early detection, early diagnosis and early treatment” can achieve the maximum therapeutic benefits.
The present study has a few limitations. First, we only recruited 50 patients and only 40 sets of data were analyzed at last. The small sample size may have limited the statistical power. Second, in this study, the main emotion disorder was anxiety while the patients seldom revealed symptoms of depression, which may be because the short duration of illness.
In conclusion, GMV analysis revealed an abnormal pain perception system, either by decreased descending pain inhibition or increased pain facilitation may be responsible for the symptoms of pain anxiety in CP/CPPS. These finding might be potential parameters for assessing severity of CP/CPPS and prospective biomarkers for clinical observation before and after intervention.
Ethics approval and consent to participate
This study has been approved and will be supervised by the Ethics Committee of Huashan Hospital, Fudan University (Ethics Approval No. 2021–772.) and the Ethics Committee of Jing’an District Central Hospital, Fudan University (Ethics Approval No. 2020–05). All enrolled patients will sign written informed consent prior to sample collection.
The datasets used and analyzed in the current study are available from the corresponding author on reasonable request.
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
[Crossref] [Google Scholar] [Indexed]
Citation: Sun C, Hu Q, Xia G, Tan Y, Ge S, Guo Y (2022) The Alterations of Brain Gray Matters in the Patients of Chronic Prostatitis/ Chronic Pelvic Pain Syndrome Evaluated by Magnetic Resonance Imaging. J Hotel Bus Manage. 11:256.
Received: 18-Feb-2022, Manuscript No. ANO-22-15108; Editor assigned: 21-Feb-2022, Pre QC No. ANO-22-15108 (PQ); Reviewed: 07-Mar-2022, QC No. ANO-22-15108; Revised: 11-Mar-2022, Manuscript No. ANO-22-15108 (R); Published: 18-Mar-2022 , DOI: 10.35248/2167-0250.22.11.256
Copyright: © 2022 Sun C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Sources of funding : NO