Journal of Sleep Disorders & Therapy
Open Access
ISSN: 2167-0277
+44 1478 350008
ISSN: 2167-0277
+44 1478 350008
Research Article - (2020)Volume 9, Issue 6
Objective: Patients who underwent bilateral sagittal split osteotomy with mandibular setback had been evaluated using lateral cephalograms to identify sites of mechanical obstruction that predispose to airway obstruction. The bioadaptive changes that occur in the peri-airway structures in the post-operative period were evaluated.
Methods: The hard and soft tissue landmarks used in cephalometry were used to trace and measure the pharyngeal airway space (PAS) and changes in position of hyoid. Amount of mandibular setback, PAS width, PAS area and changes in the hyoid position were recorded. The difference in pre- and post-operative values measured from cephalometric tracings were analyzed statistically using repeated measure ANOVA.
Results: The results demonstrated a significant reduction in PAS width and area corresponding to the decrease in length of mandible after BSSO setback. The decrease in PAS width was found to be 41% of the amount of mandibular setback at 6 months. The mean mandibular setback recorded at 6 months was 8.2 mm. The mean reduction in PAS width registered at 3 and 6 months were 3.8 mm and 3.4 mm (p value 0.001),marginally reclaiming the PAS width at 6 months. The mean reduction in PAS area at 3 and 6 months were 1.6 cm2 and 2.1cm2 (p value 0.009) demonstrating no recovery in the PAS area. The hyoid was displaced posteriorly and inferiorly; the mean displacements in the posterior direction at 3 and 6 months were 2.6 mm and 2 mm (p value 0.013) and inferior direction were 3 mm and 4 mm.
Conclusion: Mandibular setback surgery has the potential for narrowing the pharyngeal airway space with a significant reduction in PAS width and area, that could predispose to OSA. The results demonstrate that bioadaptive changes of the hyoid are greater post-surgery and tend to settle in the direction of its pre-surgical position in the anteroposterior plane and drift inferiorly in the supero-inferior plane in an attempt to restore the airway space.
Mandibular setback surgery; Pharyngeal airway dimensional changes; Hyoid bone positional changes; Obstructive sleep apnea; Lateral cephalograms
Mandibular setback osteotomy produces changes in the skeletal and soft tissue components of the orofacial complex [1,2]. Compensatory alteration in the pharyngeal, supra hyoid, and infra hyoid musculature take place post-operatively [3,4]. It is possible that bilateral sagittal split osteotomy (BSSO) with setback may induce a non-adaptive and unfavorable oropharyngeal change, promoting or exacerbating a sleep related breathing disorder (SRBD) [5,6]. Changes in the position of the tongue and hyoid bone and consequent narrowing of the pharyngeal airway space (PAS), has been implicated in the development of obstructive sleep apnea (OSA) [7,8]. Soft tissue imaging of airway structures has been used to identify sites of mechanical obstruction that predispose to OSA [9]. The authors hypothesized that mandibular setback surgery in prognathic patients would produce bioadaptive changes of the hyoid bone and the associated structures, re-establishing the pre surgical dimensions of the pharyngeal airway in the long term. The study aims to examine the airway dimensional changes in patients undergoing bilateral sagittal split osteotomy with mandibular setback and the bioadaptive changes of the hyoid bone and soft tissues using lateral cephalograms.
Study design - Cross sectional observational study
The records of eight adult patients who underwent BSSO with mandibular setback and followed up for a period of 6 months were selected to evaluate for the changes in the PAS, hyoid bone position and sleep scores. The surgical procedure in all the selected cases consisted of BSSO with mandibular setback only. Procedures involving multiple osteotomies were excluded. All the patients had their osteotomy sites fixed with miniplates followed by maxillomandibular fixation (MMF) for 1 week postoperatively. All the patients required post-surgical orthodontics for correction of minor occlusal discrepancies. None of the patients had any surgical or growth-related relapse during the evaluation period. The hard and soft tissue landmarks used in cephalometry were used to trace and measure the hypopharyngeal airway space and changes in position of hyoid bone. Three patients with incomplete details and erroneous radiographs not prescribing to the set standards and requirements were excluded. The body mass index (BMI) values and the Epworth sleepiness scale (ESS) scores were retrieved from the patient’s dossier maintained in the department record library. Patients who had recorded a normal BMI were included in this study.
Cephalometry
Lateral cephalometric radiographs were obtained 1-monthpresurgery and 3- and 6-monthspost-surgery for all patients. The lateral cephalograms were taken with the Frankfort horizontal plane parallel to the floor. Subjects were asked to remain still and not to chew or swallow and to occlude their teeth. Four separate tracings for each lateral cephalogram were made, which were then overlaid for accuracy and reproducibility. All lateral cephalograms were traced randomly by a single evaluator with dates covered to eliminate bias and were measured within a weeks’ time to minimize errors due to time lag. The hard and soft tissue landmarks used in cephalometry were used to trace and measure the PAS and changes in position of the hyoid bone. The difference in pre- and post-operative values measured from cephalometric tracings were analyzed statistically using repeated measure ANOVA. Amount of mandibular setback, PAS width, PAS area and changes in the hyoid position in the anteroposterior and supero-inferior planes were recorded from cephalometric tracings. The hard and soft tissue cephalometric landmarks pertinent to this study are cataloged in Table 1.
Table 1: Hard and soft tissue cephalometric landmarks.
| 1 | Sella (S) | Centre of sella turcica |
| 2 | Nasion (N) | Most anterior point on the fronto-nasal suture |
| 3 | NSL | Line through N and S |
| 4 | Porion (Po) | The most superior point of the external auditory meatus |
| 5 | Orbitale (Or) | The most inferior point of the orbit |
| 6 | Anterior Nasal Spine (ANS) | The tip of the anterior nasal spine |
| 7 | Posterior Nasal Spine (PNS) | The most posterior point at sagittal plane on the bony hard palate |
| 8 | Pterygomaxillary point (Ptm) | The intersection between the nasal floor and the posterior contour of the maxilla |
| 9 | Gnathion (Gn) | The most inferior point on the mandibular symphysis |
| 10 | Gonion (Go) | The most posterior and interior point of the mandible |
| 11 | Pogonion (Pg) | The most prominent point on the chin |
| 12 | Hy | The most superior and anterior point on the body of the hyoid bone |
| 13 | ATA | Anterior tubercle of atlas |
| 14 | Cv2tg | Odontoid process of the second cervical vertebrae |
| 15 | Cv2ip | Most posterior and inferior point of the second cervical vertebra |
| 16 | OPT | Odontoid process tangent through Cv2tg and Cv2ip |
| 17 | Cv4ip | The most posterior and inferior point of the fourth cervical vertebra |
| 18 | Tb | The most posterior point of the tongue |
| 19 | MGF | Median glossoepiglottic fold |
| 20 | Phw | Posterior pharyngeal wall |
The points used for orientation and superimposition were i) a line connecting orbitale and porion referred to as Frankfort horizontal (FH) ii) a vertical line passing through Ptm termed as pterygomandibular vertical (PTV) iii) a cervical vertebra tangent connecting Cv2tg and Cv4ip (CVT) (Figure 1).
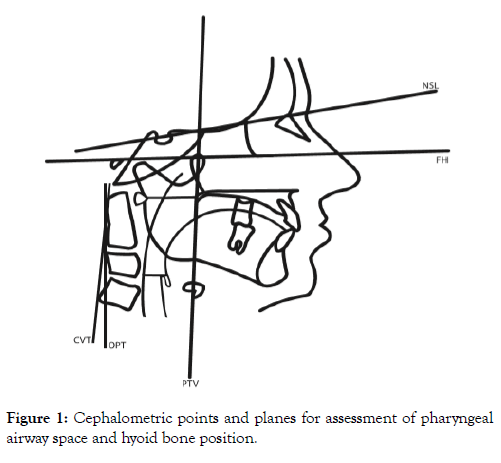
Figure 1: Cephalometric points and planes for assessment of pharyngeal airway space and hyoid bone position.
The PAS was outlined in cephalographic tracings using the method described by Tselnik et al. [1]. A line connecting the posterior nasal spine (PNS) and anterior tubercle of atlas (ATA) defined the superior border of PAS. A line drawn across the median glossoepiglottic fold (MGF) parallel to FH defined its inferior border. The posterior border of PAS was outlined by the posterior pharyngeal wall (Phw) and the anterior border; by the posterior tongue outline and the PTV. The amount of mandibular setback was calculated using differences in measurements taken on a line parallel to FH, between pogonion (Pg) and PTV on sequential radiographs. The PAS width was derived from a line connecting Tb and Phw drawn parallel to FH (Figure 2) A 3 mm2 grid superimposed over the PAS was used to calculate the area. The grid allows a simple, direct, convenient and reproducible measurement of the PAS area (Figure 3). The anteroposterior position of the hyoid bone was measured as the horizontal distance from Hy to CVT. The vertical position of the hyoid was measured as the perpendicular distance from Hy to FH (Figure 2).
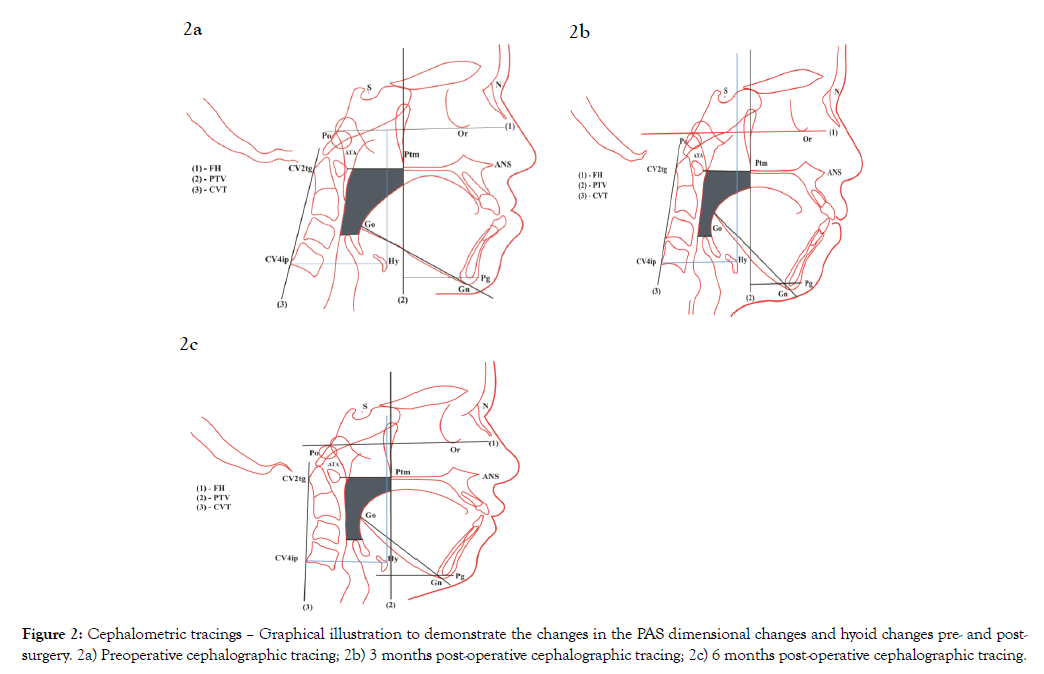
Figure 2: Cephalometric tracings – Graphical illustration to demonstrate the changes in the PAS dimensional changes and hyoid changes pre- and postsurgery. 2a) Preoperative cephalographic tracing; 2b) 3 months post-operative cephalographic tracing; 2c) 6 months post-operative cephalographic tracing.
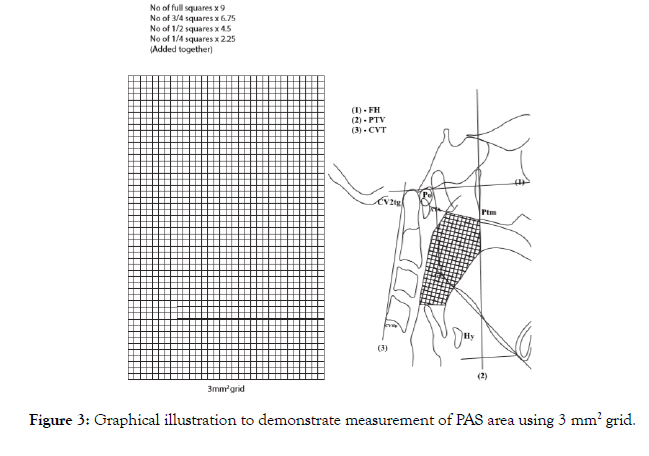
Figure 3: Graphical illustration to demonstrate measurement of PAS area using 3 mm2 grid.
BMI
Body mass index was calculated using the formula Weight (Kg) X 10000 / Height 2 (cm) for each subject. The BMI of the subjects ranged between 19-23.
Epworth sleepiness scale
The ESS scores prior to and after surgery were recorded using a standard questionnaire. This tool was used for clinical assessment to evaluate SRBD following surgery.
Statistical methods
The data were analyzed by repeated measure ANOVA. The data were expressed as mean and standard deviation. Pair wise comparison and p value of each variable were determined. Repeated measure analysis of this data was performed and a p value <0.05 was considered as statistically significant. Data analysis was performed using SPSS version 16.0.*SPSS Inc. Released 2007. SPSS for windows, Version 16.0. Chicago. SPSS Inc.
The results are summarized in Tables 2-6. The mean value of mandibular setback recorded at 6 months was 8.2 mm (range 7-12 mm) which denoted the mean decrease in length of the mandible. There was no surgical relapse noted at 3 and 6 months (Table 2). There had been a reduction in both PAS width and area corresponding to the decrease in length of mandible The mean reduction in PAS width (Tb-Phw) at 6 months follow up was 3.4 mm(range 2-4 mm), which was statistically significant ( p value 0.001) (Table 3). The PAS width change was 41% of the amount of mandibular setback. The mean reduction in PAS area at 6 months follow up was 2.1 cm2 (range 0.77-2.29 cm2) which was statistically significant (p value 0.009) (Table 4).
Table 2: Amount of mandibular setback compared with pre-operative values.
| Preoperative PTV-Pg measured in mm | Postoperative PTV-Pg at 3 months measured in mm | Mean difference | P value (Pair wise) | Postoperative PTV-Pg at 6 months measured in mm | Mean difference | P value (Pair wise) | P value (Repeated measure) |
|---|---|---|---|---|---|---|---|
| 51.4 ± 12.9(34-61) | 43.8 ± 12.1(28-54) | 7.6 | 0.001 | 43.2 ± 11.9(28-54) | 8.2 | 0.001 | <0.001 |
Note: PTV (pterygomandibularvertical): A vertical line passing through Ptm; Pg: Pogonion; mm: Millimeter; The data are expressed as means ± SD (range)
Table 3: Decrease in PAS width compared with pre-operative values.
| Preoperative PAS width (Tb-Phw) in mm | Postoperative PAS width at 3 months (Tb-Phw) in mm | Mean difference | P value (Pair wise) | Postoperative PAS widthat 6 months (Tb-Phw) in mm | Mean difference | P value (Pair wise) | P value (Repeated measure) |
|---|---|---|---|---|---|---|---|
| 16 ± 3.5 (11-17) | 12.2 ± 3.7 (8-17) | 3.8 | 0.003 | 12.6 ± 2.9 (9 -15) | 3.4 | 0.003 | 0.001 |
Note: mm: Millimeter; PAS: Pharyngeal airway space; Tb: The most posterior point of the tongue; Phw: Posterior pharyngeal wall; The data are expressed as means ± SD (range)
Table 4: Decrease in PAS area compared with pre-operative values.
| Preoperative PAS area in cm2 | Postoperative PAS area at 3 months in cm2 | Mean difference | P value (Pair wise) | Postoperative PAS area at 6 months in cm2 | Mean difference | P value (Pair wise) | P value (Repeated measure) |
|---|---|---|---|---|---|---|---|
| 13.7 ± 3.7(10.5 – 19.7) | 12.1±3.6(9.8 - 18.2) | 1.6 | 0.004 | 11.6±2.6(9.8-15.4) | 2.1 | 0.003 | 0.009 |
Note: PAS: Pharyngeal airway space; cm2: Square centimeter; The data are expressed as means ± SD (range)
Table 5: Posterior displacement of hyoid bone (Hy-CVT) compared with pre-operative values.
| Preoperative Hy to CVT measured in mm | Postoperative Hy to CVT at 3 months measured in mm | Mean difference | P value (Pair wise) | Postoperative Hy to CVT at 6 months measured in mm | Mean difference | P value (Pair wise) | P value (Repeated measure) |
|---|---|---|---|---|---|---|---|
| 54.8 ± 3.6 (51-60) | 52.2 ± 3.8 (49-58) | 2.6 | 0.003 | 52.8 ± 3.5 (49-57) | 2 | 0.047 | 0.013 |
Note: Hy: The most superior and anterior point on the body of the hyoid bone; CVT: Cervical vertebra tangent connecting Cv2tg and Cv4ip; mm: Millimeter; The data are expressed as means ± SD (range)
Table 6: Inferior displacement of hyoid bone (Hy- FH) compared with pre-operative values.
| Preoperative Hy to FH measured in mm | Postoperative Hy to FH at 3 months measured in mm | Mean diuerence | P value (Pair wise) | Postoperative Hy to FH at 6 months measured in mm | Mean diuerence | P value (Pair wise) | P value (Repeated measure) |
|---|---|---|---|---|---|---|---|
| 83.6 ± 5.5 (77-91) | 86.6 ± 6.2 (78-91) | 3 | 0.189 | 87.6 ± 4.9 (79-91) | 4 | 0.065 | 0.089 |
Note: Hy: The most superior and anterior point on the body of the hyoid bone; FH: Frankfort horizontalplane;
mm: Millimeter; The data are expressed as means ± SD (range)
The hyoid bone was displaced posteriorly in the anteroposterior plane. The mean displacement in this horizontal plane (Hy-CVT) was 2.6 mm (range 2 mm-4 mm) at 3 months and 2 mm (range 0-4 mm) at 6 months which was statistically significant (p value 0.013) (Table 5). In the supero-inferior plane, the hyoid bone was displaced inferiorly. The mean displacement in the vertical plane (Hy-FH) was 3 mm (range 0 -10 mm) at 3 months and 4 mm (range 0-9 mm) at 6 months (Table 6).
The ESS scores in the present study suggested that none of the patients had a predisposition to SRBD or OSA within the 6 months follow up period. The pre- and post-operative ESS scores were normal and ranged between 1 and 4.
The purpose of the study was to examine the airway dimensional changes in patients undergoing BSSO with mandibular set back surgery and the role of bioadaptive changes of the hyoid and associated structures in re-establishing the pre-surgical dimensions of the pharyngeal airway. The mean mandibular setback recorded at 6 months was 8.2 mm (range 7-12 mm) which indicated the mean decrease in length of the mandible. This study demonstrated a significant reduction in PAS width and area corresponding to the decrease in length of mandible after BSSO setback. The mean reduction in PAS width registered at 3 and 6 months were 3.8 mm and 3.4 mm (p value 0.001), marginally reclaiming the PAS width at 6 months. The decrease in PAS width (3.4 mm) was found to be 41% of the amount of mandibular setback (8.2 mm) at 6 months. The mean reduction in PAS area at 3 and 6 months were 1.6 cm2 (range 0.71-2.22 cm2) and 2.1 cm2 (range 0.77-2.29 cm2) demonstrating no recovery in the PAS area. The hyoid bone displaced posteriorly in an anteroposterior plane (Hy-CVT). The mean posterior displacement of hyoid (Hy-CVT) was 2.6 mm (range 2-4 mm) at 3 months and 2 mm (range 0-4 mm) at 6 months which was statistically significant (p value 0.013). The hyoid bone displaced inferiorly in a supero-inferior plane (Hy-FH). The mean inferior displacement of hyoid (Hy-FH) was 3 mm (range 0-10 mm) at 3 months and 4 mm (range 0-9 mm) at 6 months. The results demonstrate that bioadaptive changes of the hyoid are greater postsurgery and tend to settle in the direction of its pre-surgical position in the anteroposterior plane and drift inferiorly in the superoinferior plane at 6 months follow-up. The hyoid displacement may occur in a direction as dictated by the musculature and peri-airway structures in an attempt to restore the airway space.
In this study the cephalograms were taken with the FH parallel to the floor as in previous studies [6,10]. The cranio-cervical hyperflexion or hyperextension that characterizes these patients before and after surgery could not be assessed as the cephalograms were not taken in natural head position [8,11-16].
Muto et al suggested that when measuring the PAS, head posture or cranio-cervical angulation should be considered, as the changes in head posture can affect size of PAS. The above authors were of the opinion that cranio-cervical angulation (OPT/NSL) changed considerably after BSSO setback and it was difficult to obtain a constant value for OPT/NSL even when the orbito-auricular plane was maintained parallel to the floor [10]. It was also reported that head posture is significantly related to the PAS; a change in craniocervical inclination of 100 was found to alter the PAS by 4 mm [16].
Achilieos et al. reported that cervical hyperflexion occurs after mandibular setback osteotomy to compensate for the decrease in PAS [12]. The craniofacial morphology is related to the PAS and radiographs are taken at a smaller cranio-cervical angulation in patients with mandibular prognathism as they retrude it, thereby causing cervical hyperextension and reduced PAS values, whereas patients with mandibular retrognathism protrude it causing cervical hyperflexion, increased cranio-cervical angulation and increased PAS values. Therefore, Muto et al recommended correction of data by calculating at an OPT/NSL value of 1030, as it demonstrated larger changes in the PAS than measured values [10].
No correction of PAS data for the errors in head posture had been attempted in this study. However, precautions were taken while taking radiographs to minimize the errors. The cephalograms were taken with the FH parallel to the floor. Subjects were asked to remain still and not to chew or swallow and to occlude their teeth in centric occlusion to avoid inaccurate and contradictory results. The authors recommend that patient positioning with FH as a reference is more appropriate than natural head position for evaluating airway changes because it eliminates the effect of head posture changes that are known to occur when the jaws are moved forward or backward.
The imaging technique for morphologic airway evaluation after mandibular setback surgery includes cephalometric radiography [1,9,17-22], computed tomography (CT) [23], cone beam computed tomography (CBCT) [24-26] and magnetic resonance imaging (MRI) [27]. Cephalometric radiography is an indispensable and routinely used imaging technique for surgical orthodontic treatment; with no additional financial or radiation burden and ethical issues; so, it was chosen from among the imaging modalities. The advantages with lateral cephalograms are wide availability, simplicity, low expense, ease of comparison with other studies, patient compliance and minimal radiation whereas the disadvantages include the lateral viewing angle, two dimensional representation of a three dimensional structure and lack of volumetric data of the airway. However lateral cephalograms may provide useful information in the estimation of retrolingual and nasopharynx volume [28].
Computed tomography (CT) and magnetic resonance imaging (MRI) appear to be superior to cephalometry about estimating the size of oropharynx and hypopharynx. CT allows better delineation of the soft tissue and air. In three-dimensional computed tomography (3DCT), the lateral and frontal pharyngeal width can be compared [29]. A study comparing airway dimensions on lateral cephalogram and 3DCT reported significant correlation between the PAS measured with lateral cephalograms and the volume of the pharyngeal airway on CT, but the former could not provide information about the lateral structures and cross sectional area of the upper airway [9].
Pracharktam et al. studied the effect of postural changes on the airway using cephalograms in upright and awake supine positions. They observed that the posterior superior pharyngeal airway space was reduced when changing from upright to supine posture [30]. Pae et al. proposed that the oropharyngeal cross-sectional area decreases in the supine position advocated in CT, when compared to the upright position used in cephalograms [31]. Thus, CT studies for airway volume estimation are also subject to limitations.
Partinen et al. in a study on OSA patients concluded that the cephalometric variables were statistically significant predictors of elevated respiratory index and standardized cephalometric radiographs could be useful in determining the appropriate treatment for OSA patients. They noted that a PAS width less than 5 mm (measured from base of tongue to posterior pharyngeal wall along a line drawn through B point to gonion) and a mandibular plane (MP) to hyoid distance greater than 24 mm had the highest respiratory distress index [32]. Riley showed that a PAS less than 11 mm and MP to hyoid distance greater than 15.4 mm were indicative of OSA [33]. Another possible factor related to SRBD is the underlying skeletal craniofacial type. The two patients described by Riley et al. seem to have a dolichocephalic facial appearance with a large nasion sella-mandibular plane angle [7]. Inferior positioning of hyoid bone has been suggested as a bioadaptive mechanism to restore the airway space; on the contrary, a downward drift of hyoid has also been considered as a diagnostic indicator of OSA. This may be because; bioadaptive mechanisms ought to have minimal influence in OSA patients or in large mandibular setbacks. Further, OSA patients are contemplated to have additional risk factors which drives the hyoid inferiorly beyond the limits of adaptive threshold.
BMI was incorporated in this study to eliminate a known confounding factor as obesity plays a role in determining the shape of the pharyngeal lumen in awake subjects [34]. Some subjects with a large BMI, and sleep disordered breathing showed diminished respiratory function during sleep post operatively [6]. Swelling of the pharyngeal space caused by mandibular setback surgery increases the work of breathing in the immediate post-operative period, with a gradual recovery, with reduction of swelling within one month [35]. In the present study immediate post-operative cephalograms were not assessed because the follow up examination had been designed to observe osseous healing also. This allowed for soft tissue edema to settle downand adaptation to a more stable cranio-cervical angulation.
A standard instrument (Epworth sleepiness scale) is a simple tool in clinical practice to assess the degree of self-related sleepiness and is used for screening OSA. A value above 10 is considered abnormal. The ESS score is generally high in patients with OSA [36,37]. The ESS scores in the present study suggested that none of the patients had a predisposition for SRBD. The pre- and post-operative ESS scores were normal and ranged between 1 and 4.
The Fujita classification of airway obstruction divides the velohypopharynx into three descriptive levels; Type I is retropalatal, posterior to the soft palate or velopharyngeal, Type II is both retropalatal and retro-lingual or velohypopharyngeal and Type III is retro-lingual, posterior to the tongue base or hypopharyngeal Mandibular setback surgery is more commonly associated with a narrowing of the retrolingual or hypopharyngeal airway in the reported studies [1,18,24]. In the present study, there was a reduction in the retrolingual airway,6 months post-surgery in most patients (Figures 2a, 2b, 2c). It is reasonable to assume that as the mandible is surgically retruded, the size of the oral cavity reduces and the relative tongue proportion increases. The tongue may then be displaced, superiorly and posteriorly, thereby reducing the retrolingual airway dimension [38-41]. If a post-operative narrowing commensurate with OSA is anticipated, other surgical options such as bimaxillary osteotomy should be explored [33,42,43]. The results in the current study agree with the earlier studies reported in the literature [1,8,18,24,44-46].
The position of the hyoid bone is one of the important factors for maintaining the airway space. It is determined by the conjoint action of the supra and infra hyoid muscles and the resistance provided by the elastic membrane of the larynx and trachea. It has been shown that the hyoid bone adapts to anteroposterior changes in head position and to alteration in the inclination of the mandible [46].
In the current study, the vertical position of hyoid from FH was measured. The authors are of the view that FH, in comparison to MP would be a more stable reference plane, unaltered by surgical intervention and uninfluenced by the rotation of the mandible. The Hy to FH measurements suggested an inferior displacement of the hyoid bone, at 3- and 6-monthspost-surgery. In the anteroposterior plane, Hy to CVT measurements suggested a posterior repositioning of hyoid bone at 3 months and a tendency to move towards its pre-surgery position at 6 months post-surgery. Wickwire et al suggested that after surgical mandibular setback the hyoid descends drawing the root of the tongue down and out of the overcrowded pharynx [39]. The displaced hyoid bone showed a tendency to return to its original position in the long term [46]. Eggensperger reported that inferior displacement of hyoid bone remained 12 months after surgery, although there was no significant posterior displacement [3]. The posterior and inferior displacements of the hyoid bone were biological adaptations to maintain the airway space [6]. The current study also agrees with other research indicating an inferior positioning of hyoid bone [1,3,12,47,48].
Patients undergoing mandibular setback surgery should be followed up till their old age to monitor for the development of any airway obstruction [49]. Other predisposing factors of OSA like obesity [50], short necks [51], macroglossia [38], large uvula [21], dolichocephalic facial appearance [45] and excessive soft tissue around nasopharyngeal area [27,49] should be evaluated prior to mandibular setback surgery. Guven et al. found that the normal value of PAS based on lateral cephalometric study is 11 ± 2 mm [47]. Hochban reported that the average preoperative PAS in a prognathic patient is 16 mm measured between Tb and Phw [45]. In the present study the mean preoperative PAS width measured was 16 ± 3.5 [11-17].
The bioadaptive changes that occur in the oropharynx, hypopharynx and its associated structures of tongue, hyoid bone, supra hyoid and infra hyoid muscles play an important role in restoring the airway space in the post-operative period. Following mandibular setback surgery, the suprahyoid muscles in the floor of the mouth and tongue, viz. anterior belly of digastric, mylohyoid, geniohyoid and genioglossus could exert pressure on the hyoid bone, causing its posterior and inferior displacement. This can be correlated radiographically by the reduced Hy-CVT and increased Hy-FH measurements at 3 months follow up. The hyoid bone assumes a more anterior position in later follow-ups, which is considered as an adaptive change to regain the PAS and to maintain a forward tongue posture. This can be correlated on lateral cephalograms with an increase in Hy-CVT measurements. The inferior positional adaptation of the hyoid bone is likely to restore the PAS and reestablish the length and tonicity of the suprahyoid muscle fibers altered following mandibular setback surgery. The long term adaptational change in the hyoid and its musculature is a question to answer.
The limitations in the present study include a small sample size, use of conventional methods, and a follow up period limited to 6 months. Moreover, no assessments were made about the counterclockwise rotation of mandible, PAS at the level of soft palate and occlusal stability.
The present consensus is that large mandibular setbacks may affect the normal biological and physiological adaptations that restore the airway space postoperatively, particularly in patients presenting with predisposing factors vulnerable for OSA. Bimaxillary osteotomies could be a more viable treatment alternative in such patients.
Mandibular setback surgery has the potential for narrowing the PAS with a significant reduction in width and area, that could predispose to OSA. This study demonstrated a significant reduction in PAS width and area corresponding to the decrease in length of mandible after BSSO setback. The decrease in PAS width was found to be 41% of the amount of mandibular setback at 6 months. The mean mandibular setback recorded at 6 months was 8.2 mm. The mean reduction in PAS width registered at 3 and 6 months were 3.8 mm and 3.4 mm (p value 0.001), marginally reclaiming the PAS width at 6 months. The mean reduction in PAS area at 3 and 6 months were 1.6 cm2 and 2.1 cm2 (p value 0.009) demonstrating no recovery in the PAS area. The hyoid was displaced posteriorly and inferiorly; the mean displacements in the posterior direction at 3 and 6 months were 2.6 mm and 2 mm (p value 0.013) and inferior direction were 3 mm and 4 mm. The results demonstrate that bioadaptive changes of the hyoid are greater post-surgery and tend to settle in the direction of its presurgical position in the anteroposterior plane and drift inferiorly in the supero-inferior plane in an attempt to restore the airway space.
We thank all the staff members in the Department of Oral and Maxillofacial Surgery, Government Dental College, Kozhikode, Kerala, India, for their support in conducting this study. We also thank Mr. Shylendra Nath S, First Stroke, Thiruvananthapuram for the graphic illustrations.
This study conformed to the tenets of the Declaration of Helsinki.
The authors report no conflict of interests. The study received no significant financial support that could have influenced its outcome.
Citation: Dain CP, Thomas JP (2020) The Bioadaptive Changes in the Pharyngeal Airway and Hyoid Position Following Mandibular Setback Surgery: A Cephalometric Study. J Sleep Disord Ther 9:321.
Received: 30-Aug-2020 Accepted: 09-Oct-2020 Published: 16-Oct-2020 , DOI: 10.35248/2167-0277.20.9.321
Copyright: © 2020 Dain CP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.