Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Review Article - (2016) Volume 5, Issue 1
The current study aimed to evaluate the effects of varicocelectomy on semen quality and Assisted Reproductive Technology (ART) clinical outcomes. This meta-analysis was performed using Ovid (Medline, Adis, LWW, Embase; 1974 to 2014 November 10) and the PubMed (until 2014 November 10) databases. Male infertility, varicocelectomy and assisted reproductive technology were required as keywords. Data were analysed with STATA 11.0. Odds Ratio (OR) and 95% Confidence Interval (CI) were used to assess the effects of varicocelectomy on the ART clinical outcomes and funnel plots help to detect publication bias. 538 of 1068 participants issue from 7 original sources from diverse area in the world underwent varicocelectomy followed by ART between 2001 and 2011. Globally, defected semen parameters were improved after varicocelectomy among treated groups in all these studies. Significant improvement in clinical pregnancy (OR=1.76; 95% CI: 1.35-2.29, P<0.0001) and decrease of miscarriage rate (OR=0.65; 95% CI: 0.42-0.99, P=0.042) after ART use-among treated group; and finally, undergo ART specifically Intracytoplasmic Sperm Injection (ICSI) after varicocelectomy may increase live birth among treated group; Although 4 of these studies showed statistical differences, overall, there is no difference to achieve pregnancy among couples who underwent varicocelectomy and followed ART (OR=1.58; 95% CI: 0.82-3.03; P=0.172). Overall, the findings of the study suggested that varicocelectomy improves semen quality and therefore may reduce miscarriages, increase clinical pregnancy and live birth rates of couples who undergo ART specifically ICSI.
<Keywords: Varicocelectomy; Male infertility; ART; Pregnancy outcomes
Infertility affects 10-15% of couples who are trying to conceive and male factors account for 40-50% [1,2]. Varicocele is responsible of onethird of cases and stand as the most frequent cause of male infertility [3]; 21-41 % of men with primary and up to 81% with secondary infertility are due to varicoceles [4,5]. Even though, varicocele pathophysiology remains unclear, Sofikitis et al. [4] recently demonstrated the whole defect mechanism on testicular spermatogenetic activity and epididymal spermatozoa maturation process. The development of varicocele affecting leydig cell secretory function results in bilateral intratescular testosterone content although, impact the sertoli cell secretory function.
The most important outcomes of varicocele repair in male infertility should be the pregnancy and live birth for the couple. Unfortunately, the management of male infertility associated with varicocele has always remained one of the most difficult and constant critical issue for human reproduction. Hence, despite the great spectacular progress of assisted reproductive technologies (In Vitro Fertilization/ Intracytoplasmic Sperm Injection IVF/ICSI, Intrauterine Insemiation/ IUI); very few Randomized, Controlled Trials (RCT) set real evident benefit of varicocelectomy on men fertility. Thus, patients with varicocele are generally recommended to undergo varicocelectomy to reverse its impairments and mostly in some cases, surgical varicocele repair are followed by Assisted Reproductive Technology (ART) [5-11].
Since decades, varicocelectomy benefits remain very controversial. Some studies suggested that varicocelectomy may improve clinical pregnancy and live birth rates by ICSI of infertile couples in which the male partner has clinical varicocele [6,12-15] In contrast, several others have shown that varicocelectomy does not impact pregnancy outcomes [7,16-18], even following ICSI procedures and surgical repair itself is a trauma to testis and spermatogenesis. However, according to the 2004 and 2006 Recommendation of the male infertility by the American Urological Association (AUA) and American Society for Reproductive Medicine (ASRM), [2,19,20] and the European Association of Urology (EAU) 2012 guidelines [3,21], varicocele repair should be considered in cases of a clinical varicocele, semen abnormal parameters with more or 2 years of infertility and otherwise unexplained infertility.
To date, varicocele repair of infertile couple following by assisted reproductive technology remains controversial. Several relevant studies did not draw a definitive conclusion whether varicocelectomy is effective and beneficial to treat men infertility. However, constant and further questions are still without answers on it real necessity compared with ART. In addition, there is a huge dispute about the effects of varicocelectomy on ART. Does varicocelectomy increase assisted reproductive technology clinical outcomes? Therefore, we performed this meta-analysis to assess the effects of varicocelectomy on semen quality and ART clinical outcomes.
Selection of studies
We identified comprehensive literature from Ovid (Medline, Adis, LWW, Embase; 1974 to 2014, November 10) and the PubMed (until 2014, November 10) databases. We used: male infertility, varicocelectomy and assisted reproductive technology as searching keywords. All articles performed were in english and limited to human. Reference lists of the selected studies. In addition, relevant update reports were checked.
Assessment of studies and inclusion criteria
Two investigators independently performed and assessed the quality of each article using the Newcastle-Ottawa Scale [22]. Study inclusion criteria based on discrepancies and recommendations from previous relevant articles and scientific societies (American Society of Andrology, American Urological Association, American Society for Reproductive Medicine, European Association of Urology, European Academy of Andrology and WHO [23]) for the management of male infertility due to varicoceles. The eligible studies met: 1) Study design included comparison of outcomes of varicocelectomy; 2) Participants with varicocele underwent ART; 3) No difference in the demographic characteristics of subjects; and 4) Outcomes included clinical pregnancy, miscarriages and live births.
Statistical analysis
The raw data extracted from eligible studies were assessed for completeness observations to guarantee the accuracy and integrity during the transfer process. Data were entered into STATA11.0 and the OR and its 95% CI to analyze the effects of varicocelectomy on the ART clinical outcomes. Heterogeneity was evaluated using the Chisquared and P <0.05 was considered statistically significant, the random effects model was used; otherwise, the fixed effects model was adopted. We used funnel plots to assess publication bias.
Characteristics of studies and participants
Of 116 potentially relevant articles, six pertinent studies and one review included original data were finally used for this meta-analysis (Figure 1). Seven retrospectives studies were analyzed from America (USA, Brazil) and Asia (Turkey, Japan); data of six studies were collected during the period of 2001-2013. Total of 1068 participants included in this research; 538 men from couples having history of successful varicocelectomy before ARTs and 530 participants as control (Table 1). Four of five studies mentioned the mean age showing that treated group are about 34 years; however, mean age was globally similar among treated and untreated groups. The effect of varicocelectomy on semen quality and ART clinical outcomes (Pregnancy, miscarriages and live birth).
| Study, year | Study design | Nation | Duration of data collection | Sample size (n) | Mean of age (Yr) | |||
|---|---|---|---|---|---|---|---|---|
| Treated (VC) | Control | Treated(VC) | Control | |||||
| Daitch et al.,[11] | Retrospective | USA | -- | 34 | 24 | -- | -- | |
| Inci et al.,[10] | Retrospective | Turkey | 2001.1-2008.5 | 35 | 9 | 34.8 | 32.3 | |
| Haydardedeoglu et al.,[8] | Retrospective | Turkey | 2003.11-2008.4 | 31 | 65 | 28.74±5.19 | 29.43±3.90 | |
| Esteves et al.,[9] | Retrospective | Brazil | 2002.1-2008.7 | 80 | 162 | 35.80±5.4 | 35.40±6.30 | |
| Pasqualotto et al.,[7] | Retrospective | Japan | 2007-2011 | 169 | 79 | -- | -- | |
| Shiraishi et al.,[5] | Retrospective | Brazil | 2000-2008 | 21 | 53 | 37.80±0.47 | 36.1±0.55 | |
| Gokce et al.,[6] | Retrospective | Turkey | 2006.1-2010.7 | 169 | 138 | 34.80±4.30 | 34.40±4.10 | |
VC: Varicocele
Table 1: Characteristics of studies and varicocele status.
All participants presented fertility problems with abnormal semen quality. The severe abnormality of sperm found in four studies was azoospermia, two other studies noted each oligoasthenozoospermia, asthenospermia and another excluded azoopermia and leukocytospermia for semen abnormalities. All treated patients underwent surgical repair for varicocele followed ART. According to varicocele correction, inguinal or subinguinal microsurgical techniques were frequently used in 5/7 of studies.
Globally, most defected semen parameters were improved after varicocelectomy among treated groups in all these studies (P <0.05). However, no statistical difference showed mainly on progressive motility and percentage strict morphology. Application of ART especially ICSI was widely provided to 1010 participants in 6 of these studies (Table 2).
| Study, year | Status of semen | Techniques for varicocele repair | The effect of varicocelectomy on semen quality in treated and untreated participants | ARTs |
|---|---|---|---|---|
| Daitchet al.[11] | Asthenospermia | Inguinal Ivanissevich or subinguinal microsurgical | Varicocelectomy did not improve semen parameters in treated vs untreated. | IUI |
| Inciet al.[10] | Azoospermia | Inguinal or subinguinal microsurgical | Varicocelectomy increased the sperm retrieval rate via microTESE in treated group (30% vs 53% , OR=2.63, 95% CI: 1.05–6.60, P=.036). | ICSI |
| Haydardedeogluet al.[8] | Azoospermia | Inguinal or subinguinal microsurgical | Varicocele repair can significantly improve the sperm retrieval rate of treated group via TESE (60.81% and 38.46% respectively, P =.01) | ICSI |
| Esteveset al. [9] | Azoospermia | Macrosurgical | Varicocele repair improved sperm count (P=.02), number of motile sperm (P<.001) and total sperm count (P<.001); no difference in progressive motility, percentage strict morphology and decreased the sperm defect score (P=.01) among treated and untreated groups. | ICSI |
| Pasqualottoet al.[7] | Oligoasthenozo- ospermia | Not stated | Not stated | ICSI |
| Shiraishiet al. [5] | Azoospermia excluded | Subinguinal microsurgical | Varicocele repair improved just semen volume (P=.0043), however no difference in sperm concentration, sperm motility and morphology among treated and untreated groups. | ICSI |
| Gokceet al. [6] | Azoospermia | Subinguinal microsurgical | Semen parameters were improved after varicocelectomy but no statistical difference on progressive motility and percentage strict morphology of pre and postoperative compared to control groups. | ICSI |
ARTs: Assisted Reproductive Technologies;
TESE: Testicular Sperm Extraction; vs: versus;
IUI: Intrauterine Insemination;
ICSI: Intracytoplasmic Sperm Injection
Table 2: The effect of varicocelectomy on semen quality.
Pregnancy outcomes reported show significant statistical clinical pregnancy rate on varicocele followed ART among treated group compared to untreated in four studies favouring varicocelectomy. Overall, the result showed significant difference of studies (OR=1.76; 95% CI: 1.35-2.29, P=0.000) (Table 3) and funnel plot (Figure 2) suggested publication bias found among these studies. In two of studies, no differences were reported about the miscarriages in treated and control groups. Although, in general significant statistical difference was reported (OR=0.65; 95% CI: 0.42-0.99, P=0.042) (Table 4); thus, varicocelectomy may help to reduce miscarriages among couples who undergo ART.
| Study, year | Treated(n) | Control(n) | OR | 95% CI | Weight | Odds Ratio | ||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | M-H, Fixed, 95% CI | ||||
| Daitchet al.[11] | 11 | 23 | 4 | 20 | 2.391 | [0.657, 8.703] | 3.78% | 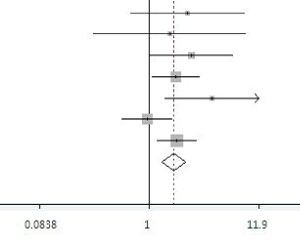 |
| Inci et al.[10] | 11 | 24 | 2 | 7 | 1.604 | [0.286, 9.12] | 2.60% | |
| Haydardedeogluet al.[8] | 23 | 8 | 34 | 31 | 2.621 | [1.024, 6.712] | 6.75% | |
| Esteveset al.[9] | 48 | 32 | 73 | 89 | 1.829 | [1.062, 3.151] | 23.00% | |
| Pasqualottoet al.[7] | 13 | 8 | 15 | 38 | 4.117 | [1.420, 11.934] | 3.86% | |
| Shiraishiet al. [5] | 52 | 117 | 25 | 54 | 0.96 | [0.540, 1.707] | 28.11% | |
| Gokceet al. [6] | 105 | 65 | 73 | 1.872 | [1.185, 2.958] | 31.89% | ||
| Total (95%CI) | 1.756 | [1.347, 2.288] | 100.00% | |||||
| Total (n) | 263 | 275 | 218 | 312 | ||||
| Heterogeneity Chi Square =7.71 (d.f.=6), Pa=0.260 ; I2 (Variation in OR attributable to heterogeneity)=22.2% Test of over effect OR=1; Z=4.17 P=0.000 |
||||||||
A: number of clinical pregnancies in treated group; B: number failed to conceive in treated group; C: number of clinical pregnancy in control group; D: number failed to conceive in control group; OR: odds ratio; d.f.:degree of freedom; CI: confidence interval; Pa : value of Q-test for heterogeneity test
Table 3: Clinical pregnancy outcome in treated (varicocelectomy) vs control group after ART.
| Study, year | Treated(n) | Control(n) | OR | 95% CI | Weight | Odds Ratio | ||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | M-H, Fixed, 95% CI | ||||
| Daitchet al.[11] | 0 | 11 | 3 | 1 | 0.019 | [0.001, 0.568 ] | 8.75% | 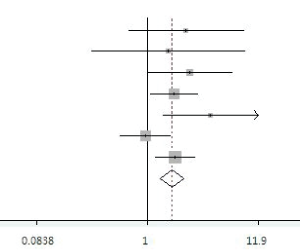 |
| Inci et al.[10] | 2 | 9 | 0 | 2 | 1.316 | [0.047, 37.157] | 1.17% | |
| Haydardedeogluet al.[8] | 3 | 20 | 7 | 27 | 0.579 | [0.133, 2.519] | 9.07% | |
| Esteveset al.[9] | 11 | 37 | 22 | 51 | 0.689 | [0.298, 1.594] | 24.85% | |
| Pasqualottoet al.[7] | 2 | 11 | 2 | 13 | 1.182 | [0.142, 9.827] | 2.90% | |
| Shiraishiet al. [5] | 40 | 12 | 17 | 8 | 1.569 | [0.544, 4.525] | 9.79% | |
| Gokceet al. [6] | 25 | 80 | 25 | 40 | 0.500 | [0.255, 0.979] | 43.47% | |
| Total (95%CI) | 0.646 | [0.424, 0.985] | 100.00% | |||||
| Total (n) | 82 | 180 | 76 | 142 | ||||
| Heterogeneity Chi squrare = 7.92 (d.f.= 6), Pa=0.244; I2 (Variation in OR attributable to heterogeneity)=24.2% Test of over effect OR=1; Z=2.03P=0.042 |
||||||||
A: number of miscarriages in treated group; B: number of clinical pregnancies until delivery in treated group; C: number of miscarriages in control group; D: number of clinical pregnancy until delivery in control group; OR: odds ratio; d.f.: degree of freedom; CI: confidence interval; P:value of Q-test for heterogeneity test; Pa: value of Q-test for heterogeneity test
Table 4: Miscarriage outcome in treated (varicocelectomy) vs control group after ART.
Publication bias of studies showed in Figure 3. We detected that heterogeneity was statistical significant (Chi-squared test, P =0.000) that led to the use of random effects model to analyse live birth outcomes. The achievement of pregnancy illustrated by the live birth examined in these studies was controversial.
Three studies reported no difference of live birth increasing among treated compared to untreated group. Even if 4 of these studies showed statistical differences, overall, there is no difference to achieve pregnancy among couples who underwent varicocelectomy and followed ART (OR=1.58; 95% CI: 0.82-3.034; P=0.172) (Table 5). Regarding the funnel plot, the publication bias existed in these studies (Figure 4).
| Study, year | Treated(n) | Control(n) | OR | 95% CI | Weight | Odds Ratio | ||
|---|---|---|---|---|---|---|---|---|
| A | B | C | D | M-H, Fixed, 95% CI | ||||
| Daitch et al.[11] | 11 | 23 | 1 | 23 | 11.00 | [1.311, 92.299] | 6.66% | 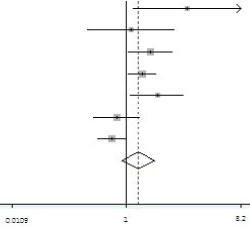 |
| Inci et al.[10] | 9 | 26 | 2 | 7 | 1.212 | [0.212, 6.935] | %8.67 | |
| Haydardedeoglu et al.[8] | 20 | 11 | 27 | 38 | 2.559 | [1.055, 6.205] | 18.05% | |
| Esteves et al.[9] | 37 | 43 | 51 | 111 | 1.873 | [1.080, 3.248] | 19.61% | |
| Pasqualotto et al.[7] | 11 | 10 | 13 | 40 | 3.385 | [1.172, 9.775] | 14.23% | |
| Shiraishi et al. [5] | 12 | 157 | 8 | 71 | 0.678 | [0.266, 1.732] | 15.50% | |
| Gokce et al. [6] | 80 | 88 | 40 | 25 | 0.568 | [0.317, 1.019] | 19.27% | |
| Total (95%CI) | 1.576 | [0.820, 3.026] | 100.00% | |||||
| Total (n) | 191 | 356 | 142 | 215 | ||||
| Heterogeneity Chisquare=20.51 (d.f.=6), Pa=0.002 ; I2 (Variation in OR attributable to heterogeneity)=70.7% Estimate of between-study variance Tau2=0.4865; Test of over effect OR=1; Z=1.37 P=0.172 |
||||||||
A: number of live births in treated group; B: number of miscarriages and failed to clinical pregnancy in treated group; C: number of life births in control group; D: number of miscarriages and failed to clinical pregnancy in control group; OR: odds ratio; d.f.: degree of freedom; CI: confidence interval; Pa: value of Q-test for heterogeneity test;
Table 5: Live birth outcome in treated (varicocelectomy) vs control group after ART.
Data analyzed in the current study revealed that 538 participants from diverse area in the world, issue from 7 original sources underwent varicocelectomy following by ARTs during the period of 2001-2011; this may be sufficient to assess male infertility due to varicoceles regarding the existing controversies [4,7,14,16,24,25] and based on updated recommendations and guidelines for good practices [3,4,19-21,23].
The mean age of 4 studies showed mid advanced age (34 years old) for men to conceive; most studies suggested the average interval of about 6 months from varicocelectomy to ART [1,24,26,27]. Regarding the present observation, discrepancies and limited outcomes of varicoclectomy following ART among couples with middle advanced age, female age and couple’s time desire to conceive in practice must be accounted. Although, longer interval between varicocelectomy and ART seems to be more productive [6,11,28,29]. The effect of varicocele repair using microsurgical techniques among men with azoospermia was predominant in this study largely promoted semen quality and clinical outcomes of couples who underwent ARTs. This result was previously demonstrated in some studies [23,25,30-32].
Moreover, several studies reported the effectiveness of IUI or ICSI to increase clinical outcomes [30,33], however Baker et al. [12] found that high DNA fragmentation index (>30) help to achieve spontaneous pregnancy. Thoroughly, spontaneous pregnancy should remain the ultimate standard for evaluating the succeed management of male infertility due to varicocele treatment. Despite the conclusion issued from Evers et al. [17] in 2003 and the recent study from Pasqualotto et al. [7] demonstrated that surgical procedure did not have any impact on pregnancy or miscarriage rates following ICSI of couples with exiting varicocele repaired, however several other studies argue that varicocelectomy has beneficial effects on ART outcomes [27,29,34].
In this study, even though, clinical pregnancy, miscarriages and live birth rates were independently inconsistent; however, global findings showed that varicocelectomy improves semen quality and therefore reduced miscarriages (OR=0.65; 95% CI: 0.42-0.99, P=0.042), increased pregnancy (OR=1.76; 95% CI: 1.35-2.29, P=0.000) and live birth rates (OR=1.58; 95% CI: 0.82-3.034; P=0.172) of couples who underwent ART especially ICSI. Overall, the use of ART specifically ICSI after varicocelectomy found in 6 studies of the current investigation revealed the increase of clinical outcomes. Performing ART after varicocele repaired among men with infertility is a long time procedure and requires couples’ adherence as well as costs and unknown long-term effects of ART. All studies included were retrospective design and even whether random effect model was used to analyze live birth outcomes, the non- randomization of participants in each study for varicocelectomy followed by ART may affect original data. Giving the existing controversies and different updated recommendations for male infertility due to varicoceles, further studies with randomized, control trials are valuable.
Varicocelectomy improved semen quality; furthermore, it may reduce miscarriages, increased clinical pregnancy and live birth rates of couples who underwent ART specifically ICSI. In spite of the longterm procedure, high associated costs and medical risks of ART, the current meta-analysis suggested that varicoceletomy is beneficial for infertile men prior to ART.
All authors declare no competing financial interests.