Advanced Techniques in Biology & Medicine
Open Access
ISSN: 2379-1764
ISSN: 2379-1764
Research Article - (2023)Volume 11, Issue 3
Background: Limitation of the lower limb mobility leads, as a result of the conscious or unconscious compensation to avoid pain, to a disturbance of the gait pattern. A noticeable deviation of gait cycle parameters is manifested by significant asymmetry between the injured and non-injured limbs. Inadequate or insufficient rehabilitation can lead to the persistence of asymmetry causing other musculoskeletal problems. It is assumed that the body-weight supported treadmill rehabilitation program is capable of effective gait symmetry restoration in patients recovering after lower limb surgery.
Methods: Thirty patients recovering after lower limb arthroplasty underwent a treatment program consisting of 6 sessions of body-weight supported treadmill exercise. Gait cycle parameters including stance time, step time, step length, swing time, and weight-bearing proportion of each limb were recorded during each exercise session. The evolution of gait asymmetry was evaluated in terms of the symmetry index.
Results: The present study demonstrated that body-weight supported treadmill therapy significantly reduces gait asymmetry. The symmetry index of stance time, step length, step time, swing time, swing time/stance time ratio, and weight bearing was improved by 42%, 33%, 48%, 37%, 49%, and 33%, respectively. The Wilcoxon test proved a significant difference across all parameters except the step length.
Conclusion: Body-weight supported treadmill has a positive effect on gait asymmetry in patients recovering from lower limbs arthroplasty. Despite their limitations, patients are able to incorporate walking in the early rehabilitation phase and eliminate the emergence of associated health problems arising as a result of mechanical compensation.
Body weight supported treadmill therapy; Antigravity treadmill; Gait asymmetry; Symmetry index; Gait parameters; Stance time; Swing time; Step length; Step time; Arthroplasty; Lower limb arthroplasty; Gait deviation
Globally, around 1.7 billion people of all ages are diagnosed with disorders of the musculoskeletal system. Approximately 440 million suffer from fractures and 528 million from osteoarthritis, the leading cause of arthroplasty [1]. These and other conditions of the lower extremities can significantly limit the ability to walk and the overall patient’s independence. The dependence between the ability to walk at normal speed and self-assessed overall health was proven by subjective assessment of older adults [2]. Regular walking has also shown beneficial effects on blood pressure, heart rate, body mass index, body fat, quality of life, and depression [3]. Any short-term or long-term limitation of walking can lead not only to the weakening of the lower limb muscles but also to the deterioration of the patient's overall health.
Limitation of the lower limb mobility leads, as a result of the conscious or unconscious compensation to avoid pain, to a disturbance of the gait pattern. There is a noticeable deviation of gait cycle parameters, manifested by significant asymmetry between the injured and non-injured limbs. The process of recovery and gait restoration is accompanied by a reduction of between-limb asymmetry and an increase in the injured limb weight bearing [4]. Inadequate or insufficient rehabilitation can lead to mechanical compensations, limitation of range of motion, disruption of proprioception, and preservation of pain, resulting in pathologic gait and the persistence of asymmetry [5,6]. Uneven load distribution can contribute to loss of bone mineral density in the underloaded limb, development of low back pain, osteoarthritis, or other conditions resulting in the necessity of joint replacement on the contralateral limb. To avoid the emergence of associated musculoskeletal problems, it is necessary to time the rehabilitation appropriately and, ideally, include technological advances enabling functional gait retraining programs as early as possible.
It is, due to all aforementioned reasons, desirable to include walking in the treatment plan of patients recovering from an injury or surgery of the locomotor system, already in the early rehabilitation stage. In order to avoid re-injury due to increased load, it is necessary to choose an approach allowing gradual loading of the extremity. Body-Weight Supported Treadmill Therapy (BWSTT), also known as Antigravity Treadmill (ATG), enables complete or partial support of the patient's weight during exercise. Unweighting the patient's body reduces his need to further unload the injured limb and thus prevents from developing a gait deviation. It is assumed that the BWSTT approach yields the asymmetry between injured and non-injured extremity reduction and normal gait pattern restoration.
The efficacy of BWSTT has been proven in the treatment of multiple neurological and musculoskeletal conditions including post-stroke paresis, Parkinson’s disease, cerebral palsy, spinal cord injury, lower limb fractures and postoperative recovery after total knee and hip arthroplasty and anterior cruciate ligament reconstruction. Despite the proven effectiveness in clinical practice, the influence of BWSTT on gait asymmetry has not yet been clearly demonstrated. While a few studies monitoring such effects in post-stroke patients did not show a significant impact, others indicated a possible beneficial effect. Current clinical evidence completely lacks studies describing the impact of BWSTT on gait symmetry in patients with other indications, for example, post-operative musculoskeletal conditions [7-20].
The aim of the present trial is to evaluate the evolution of the symmetry index (SI) of multiple gait parameters during the BWSTT program in patients recovering after lower extremity arthroplasty. As the secondary outcome measures gait parameters including stance time, step length, step time, swing time, swing/stance time ratio, and weight bearing of affected and unaffected limb development have been monitored.
Design
Data were collected at the Military rehabilitation center in Slapy, Czech Republic, between January and April 2023. Measurements were provided automatically during each session by embedded sensors and saved inside the BWSTT unit. At the end of the trial, data were assigned to respective patients and evaluated by an independent research team. Due to the lack of clinical evidence on gait symmetry in patients with musculoskeletal conditions, the sample size was estimated from published data in post-stroke patients [21]. To detect a significant (p<0.05) difference between data collected during the first and the last treatment session with 80% power, at least 16 patients are required. The study followed the 1975 Declaration of Helsinki ethical guidelines adopted by the General Assembly of the World Medical Association (1997-2000) and by the Convention on Human Rights and Biomedicine of the Council of Europe (1997) [22].
Participants
Adult patients recovering from total lower limb arthroplasty hospitalized in the Military rehabilitation center in Slapy who were willing to participate were included in the study. Those suffering from severe cardiovascular disease, bronchial asthma, angina pectoris, disc herniation, epilepsy, or any conditions with contraindicated increased abdominal pressure as well as uncooperative and pregnant patients were excluded.
Intervention
During the course of the study, each participant completed 6 exercise sessions on the BWSTT device (BTL Industries Ltd.) followed by conventional physiotherapy. BWSTT device represents a special treadmill adapted for walking or running with reduced body weight for early gait recovery of the locomotion system after disorders of neurological or musculoskeletal origin. Unweighting works on the principle of positive pressure created within the inflatable bag surrounding the lower half of the patient's body and the treadmill itself. The patient wears special shorts with an integrated half zipper, which, by zipping into the bag opening, ensures a sealed connection. As soon as the zipper is closed, the bag is inflated and the device is calibrated to the patient's weight. Next, the therapist sets the therapy parameters - speed, inclination, and the percentage proportion of supported body weight. The parameters should be adapted to the patient's condition and ability, and their progression is expected throughout the treatment program. Sessions were scheduled twice a week with a total of 6 sessions lasting 20 minutes each.
Data analysis
Gait parameters including stance time, step length, step time, swing time, and weight-bearing proportion of affected and unaffected limbs were recorded during each BWSTT session via embedded pressure sensor (H8C load cell). In addition to the measured gait parameters, the stance time/swing time ratio parameter was evaluated. The symmetry index was calculated as an indicator of gait symmetry based on the following equation [21]:
Where, P represents the respective gait parameter.
Symmetry index equal to zero indicates full symmetry, whereas value above 100 indicates full asymmetry. A negative value indicates that PAffected<PUnaffected, because of this, the absolute values were used rather than the SI itself [23].
All calculations and statistical analyses were performed using custom-written script (MatLab R2010b, Mathworks, Inc., Narick, MA, USA). Prior to the statistical analysis, data normality was tested by the Shapiro-Wilk test. As the normal distribution was rejected, non-parametric Wilcoxon sign rank test was used to evaluate the statistical significance of the difference in data taken during the first and the last therapy session. A level of p<0.05 was considered statistically significant.
A total of 30 patients in the early rehabilitation stage after arthroplasty surgery were assigned. Twenty-one patients required gait recovery due to total knee arthroplasty and nine due to total hip arthroplasty. See Table 1 for group demographics.
All participants were able to finish the full study course. The treatment was generally well tolerated with no adverse events reported. The average walking speed was 2.35 ± 0.62 km/h and the weight unloading proportion was 53.9 ± 12.3% across all treatment sessions. Inclination was not changed and remained at 0% for all participants during the entire treatment program (Table 1).
| Knee arthroplasty | Hip arthroplasty | Total | |
|---|---|---|---|
| Age, mean (SD) | 69(5.46) | 66.56(6.42) | 62.57(11.48) |
| Sex, male/female | 13-Aug | 06-Mar | 19-Nov |
| Affected limb, right/left | 13-Aug | 03-Jun | 16/14 |
Table 1: Participants demographics.
Symmetry index
The symmetry index showed improvement throughout the trial in all measured gait parameters as shown in Table 2. Stance time, step length, step time, swing time, swing time/stance time ratio, and weight bearing reported improved in symmetry index by 42%, 33%, 48%, 37%, 49%, and 33%, respectively. Only the step length symmetry ratio did not reach the level of statistical significance when comparing the data using the Wilcoxon test. The difference in the symmetry ratio of all remaining indicators was evaluated as statistically significant (Table 2).
| Stance Time (ms) | Step Length (cm) | Step Time (ms) | Swing Time (ms) | Weight Bearing (%) | Swing Time/Stance Time | ||
|---|---|---|---|---|---|---|---|
| Before | Unaffected | 1201.50 (204.50) | 52.00 (6.75) | 802.00 (190.50) | 576.50 (105.25) | 51.50 (3.00) | 0.50(0.07) |
| Affected | 1100.00 (232.00) | 50.50 (9.25) | 845.50 (139.75) | 599.00 (184.25) | 48.50 (3.00) | 0.55(0.16) | |
| Symmetry Index | 6.83 (8.10) | 3.58 (4.40) | 6.62 (7.14) | 11.36 (16.90) | 6.00 (11.00) | 9.87(31.58) | |
| After | Unaffected | 1030.50 (131.50) | 58.00 (8.75) | 768.00 (128.25) | 546.00 (115.50) | 51.00 (2.00) | 0.50(0.06) |
| Affected | 1015.00 (165.50) | 58.00 (10.50) | 764.50 (151.50) | 529.00 (123.00) | 49.00 (2.00) | 0.51(0.01) | |
| Symmetry Index | 3.97 (5.38) | 2.39 (3.84) | 3.47 (4.63) | 7.15 (6.57) | 4.00 (8.00) | 5.52(6.60) | |
| Wilcoxon (p=0.05) | Between- limb Before | <0.001 | <0.001 | 0.01 | 0.23 | <0.001 | 0.02 |
| Between- limb After | 0 | 0.03 | 0.31 | 0.97 | 0 | 0.3 | |
| Symmetry Index | <0.001 | 0.22 | <0.001 | 0.04 | 0.001 | 0.004 | |
Note: Data are displayed as median (interquartile range). P values calculated by wilcoxon sign rank test meeting statistical significance (p<0.05) are highlighted in green.
Table 2: Gait parameters and respective symmetry indexes measured during the first (before) and the last exercise session (after).
Gait parameters
The difference between affected and unaffected limbs during the first session was considered significant for all gait parameters except for swing time shown in Table 2. While stance time, step length, and weight-bearing proportion were lower for the affected limb, step time, swing time, and swing/stance time ratio were lower for the unaffected limb. The treatment program led to a reduction in between-limb differences in all parameters. Step time and swing/ stance time ratio reported almost complete elimination of asymmetry as during the last treatment no significant between-limb difference was found. Data distribution of respective gait indicators is visualized in Figure 1.
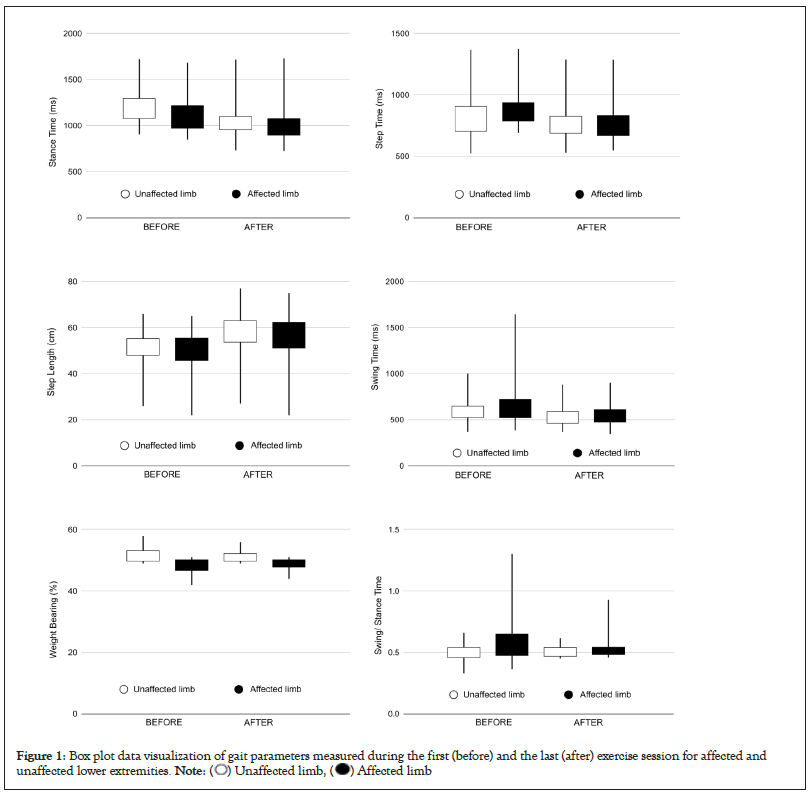
Figure 1: Box plot data visualization of gait parameters measured during the first (before) and the last (after) exercise session for affected and
unaffected lower extremities. 
Patients after arthroplasty show significant asymmetry in almost all gait parameters. The observed asymmetry direction between the affected and unaffected limb is consistent with other studies investigating gait cycles in patients after total hip arthroplasty, tibial fractures and post-stroke patients [24,25]. The absolute values of the gait parameters differ quite significantly within the individual studies, mainly because of their dependence on walking speed [26]. Since, the patients in the present study were able to walk at a relatively low speed (2.35 ± 0.62 km/h), the comparison with neurological patients may be appropriate, although not entirely accurate. The values are consistent with the data published by Wang et al. evaluating gait parameters at different speed levels in stroke patients [27].
During the 3-week BWSTT study course, a significant improvement in the symmetry of the gait parameters was reported in terms of both symmetry index and between-limb comparison. Similar findings were presented in stroke patients, but the clinical evidence of BWST on gait asymmetry in patients with musculoskeletal conditions is missing. Despite the lack of existing studies, due to the nature and principle of the therapy, the positive effect on the between-limb difference is completely explainable for multiple reasons. First of all, as the BWSTT system enables controlled weight bearing during walking or running, it provides postural support with promoted coordination of the lower limbs. The patient is able to incorporate walking without the necessary support of a therapist, crutches, or cane already in the early rehabilitation stage leading to a reduction in his need for conscious or unconscious compensation of the impaired limb. Secondly, the demands on the muscles are controlled by the proportion of the weight load and therefore can be gradually increased during the rehabilitation program. It is assumed that such an approach could lead to the development of more effective and efficient movement strategies and can prevent the occurrence of gait deviations with associated musculoskeletal conditions. Another benefit of BWSTT is that it eliminates the risk of falling while walking or running, thus allowing the patient to fully concentrate on the ongoing activity. At the same time, it also allows the therapist to fully devote himself to controlling the patient's gait pattern instead of manually supporting him during the exercise. From all the above-mentioned theoretical evidence and the results of the present study, it can be concluded that the BWSTT program can contribute to the reduction of between-limb asymmetries in patients with lower extremity impairment.
It is necessary to mention the possible limitations of this research. The absence of a control group complicates the determination of the progress achieved by BWSTT and by conventional therapy. Between-group comparison of BWSTT patients and patients who underwent a stand-alone conventional rehabilitation would provide a better insight into BWSTT outcomes. The merging of patient’s post total knee and hip arthroplasty into one group can represent another source of inaccuracy. In the future, separate studies should be considered for different affected body areas and indications, not only of musculoskeletal but also of neurological origin. The present study assumes that the reduction of asymmetry will last or will improve in the course of further rehabilitation. However, it is appropriate to support this assumption by collecting data not only during, but also after the end of the BWSTT program in a reasonable follow-up period.
Despite a few limitations, this study has an indisputable benefit, primarily because it is the very first study investigating the effect of BWSTT on between-limb asymmetry in patients recovering from musculoskeletal conditions.
Future studies could focus on a comparison between patients recovering after hip and knee arthroplasty as it could bring interesting insight into the restoration of gait symmetry. In patients recovering from arthroplasty, a significant improvement in between-limb symmetry was observed after the BWSTT program consisting of 6 sessions. These findings represent a promising approach in the rehabilitation of the musculoskeletal system, primarily due to the possibility of its early incorporation into the treatment plan with minimization of the re-injury risk or the creation of gait deviation due to impaired limb compensation.
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
[Crossref] [Google scholar] [PubMed]
Citation: Kubícek M, Brozek T (2023) The Effect of Body-Weight Supported Treadmill Therapy Program on the Gait Asymmetry in Patients After Lower Limb Arthroplasty. Adv Tech Biol Med. 11:415.
Received: 30-Jun-2023, Manuscript No. ATBM-23-25428; Editor assigned: 03-Jul-2023, Pre QC No. ATBM-23-25428 (PQ); Reviewed: 17-Jul-2023, QC No. ATBM-23-25428; Revised: 24-Jul-2023, Manuscript No. ATBM-23-25428 (R); Published: 31-Jul-2023 , DOI: 10.35248/2379-1764.23.11.415
Copyright: © 2023 Kubícek M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.