Angiology: Open Access
Open Access
ISSN: 2329-9495
ISSN: 2329-9495
Research Article - (2024)Volume 12, Issue 8
Background: Hypertension is one of the most common chronic diseases, it often occurs together with dyslipidemia, increasing the risk of cardiovascular disease. Numerous studies have confirmed that exercise can be used as a nonpharmacological treatment option to improve hypertension, but there is a paucity of information on the effects of different exercise doses on lipid levels in hypertensive patients.
Objective: To systematically evaluate the effects of different exercise doses on the levels of blood lipids Total Cholesterol (TC), Triglyceride (TG), High Density Lipoprotein (HDL), Low Density Lipoprotein (LDL) in hypertensive patients.
Methods: Randomized controlled trials on the effects of exercise on patients with hypertension were searched in four databases: PubMed, Embase, Web of Science, and Cochrane. All searches were conducted from the time of database construction to May 2023. Literature data were extracted independently by 2 researchers and evaluated for literature quality. Meta-analysis was performed by applying Stata 16.0 software.
Results: A total of 19 papers comprising 26 studies with 1458 patients were included. 8 studies were categorized as having high adherence to ACSM and 18 as having low or uncertain adherence to ACSM. Four outcome indicators, the SMD ratios for exercise interventions with high ACSM adherence versus low or uncertain ACSM adherence were as follows: TC (-0.46: -0.50), TG (-0.61: -0.18), HDL (0.53: 0.30), and LDL (-0.68: -0.23).
Conclusion: The results showed that exercise interventions with high ACSM adherence had more significant effects on lipid levels in hypertensive patients than those with low or uncertain ACSM adherence. From the differences in outcome indicators, high ACSM adherence exercise improved TG, LDL and HDL more significantly, which can effectively reduce TG and LDL and enhance HDL levels, but the improvement effect on TC was not obvious.
Hypertension; Exercise dose; Lipids; American College of Sports Medicine (ACSM)
Hypertension, as one of the most common chronic diseases, is a major risk factor for coronary heart disease, stroke, heart failure, and chronic kidney disease [1-3]. According to the World Health Organization (WHO), hypertension has affected 1 billion people worldwide, and about 9 million people die from elevated blood pressure yearly [4]. The total number of adults with hypertension is projected to increase by 60% to 1.56 billion in 2025 [5]. Hypertension and dyslipidemia often occur together, and their co-existence accelerates the process of atherosclerosis and increases the risk of cardiovascular disease [6,7]. Study shows that even if a patient's blood pressure is well controlled, the risk of cardiovascular disease is still significantly increased when LDL levels are elevated. Therefore, simultaneous management of blood pressure and blood lipids in hypertensive patients is an important means of preventing and treating cardiovascular diseases [8].
Current treatment options for hypertension include both pharmacologic and non-pharmacologic interventions. However, studies have shown that about 70% of patients with hypertension who receive only medication cannot control their symptoms [9]. Long-term medication is not only expensive but also has side effects [10,11]. Therefore, non-pharmacological treatment programs are getting more and more attention and affirmation, especially physical exercise [12]. Numerous studies have confirmed the role of exercise as a non-pharmacological treatment option for blood pressure and lipid improvement in hypertensive patients [13-19].
The ACSM recommends exercise prescriptions for hypertensive patients, which were categorized as aerobic, resistance, and flexibility exercises, with detailed descriptions of frequency, intensity, duration and type of each type of exercise [20]. However, there are fewer studies analyzing the effects of different exercise doses on hypertensive patients, especially the effects of exercise doses on lipid levels in hypertensive patients. Therefore, this systematic review aimed to explore the effects of exercise interventions with high adherence to ACSM guidelines compared to those with low or uncertain ACSM adherence in hypertensive patients.
Data sources and searches
Four databases were searched: PubMed, Embase, Web of Science and Cochrane; the timeframe of searching was from the establishment of the database to May 15, 2023. The search strategy based on the theme of exercise's effects on hypertensive patients and followed the PICOS principle, which is mainly related to the subject population, the type of intervention, and the type of experiment. The search formula subject terms and free terms showed as follows: (“Hypertension” or “Blood Pressure, High” or “High Blood Pressure” or “Systolic blood pressure” or “Diastolic pressure” or “Hypertensive disease” or “Primary hypertension” or “Secondary hypertension” or “Essential hypertension” or “Endocrine hypertension”) AND (“Exercise” or “Exercises” or “Sports” or “Trainings” or “Fitness” or “Physical exercise” or “Physical activity” or “Physical fitness” or “Aerobic exercise” or “Resistance training” or “Strength training” or “Running” or “Tai Chi” or “Jogging” or “Bicycling” or “Motor activity” or “Physical workout”) AND (“Randomized controlled trial” or “controlled clinical trial” or “randomized” or “placebo” or “randomly”).
Inclusion and exclusion criteria of studies
Inclusion criteria: (a): Published randomized controlled trial; (b): Patients with hypertension or prehypertension; (c): The intervention could be any exercise; (d) The control intervention was no treatment or usual care and (e): The study's outcome indicators included TC, TG, HDL, and LDL.
Exclusion criteria: (a): The article was a review or conference report; (b): The intervention in the control group was exercise; (c): The subjects had cardiovascular diseases such as myocardial infarction, heart failure or metabolic diseases such as diabetes mellitus and (d): Subject is receiving medication to lower or control cholesterol levels.
Data screening and extraction: The first step, according to the search strategy, all the retrieved documents will be imported into the literature management software EndNote, sieve out the duplicates in the EndNote de-emphasis function, then the remaining items will be imported into the literature management software Zotero for the next round of screening. The second step, the first round of screening was done by two authors Chen and Cui by reading the titles of the literature according to the inclusion and exclusion criteria. The third step, the abstracts and full texts of the remaining literature were read for a second round of screening. If one of the authors considered a study to be eligible or uncertain, the two authors independently reviewed and assessed whether the study met the inclusion criteria. If there was disagreement between the two authors, a discussion was held with the third author Xie, and a consensus was reached. There were no restrictions on subject age, gender, literacy level, income, geographical location, body mass index, time of publication, or language of publication in this study.
Two authors Chen, Cui independently designed EXCEL forms and extracted the relevant data for inclusion in the study. The extracted data included: (1) Basic information of the paper (title, name of the first author, year of publication, country); (2) Information of the subjects (age, gender, sample size, disease level); (3) Experimental interventions (type of exercise, frequency of exercise, intensity of exercise, duration of exercise); (4) Characteristics of the risk assessment; (5) Data of the outcome indicators (TC, TG, HDL, LDL).
We used the Engauge Digitizer software to extract the outcome data if the post-intervention outcome data were presented graphically in the text and were not explicitly stated in the text. After data extraction was completed, the exercise intervention programs (exercise frequency, exercise intensity, and exercise duration) included in the study were assessed for dose and adherence according to the ACSM recommended exercise prescription for hypertensive patients (Table 1). Adherence to the exercise dose for each study was assessed by two authors Chen, Cui by independently scoring each study's exercise intervention according to different criteria defined for each aspect of the ACSM recommended dose.
| Exercise dose | Aerobic exercise | Resistance exercise | Flexibility exercise |
|---|---|---|---|
| Frequency | 5-7 days/week | 2-3 days/week | ≥ 2-3 days per week |
| Intensity | Moderate intensity (40%-59% reserve oxygen uptake VO2R or HRR); RPE of 12-13 on the 6-20 scale | Start with 60%-70% of 1RM and gradually increase to 80% of 1RM. Perform at least 8-10 different kinds of exercises. Muscular strength: 8~10 repetitions per set; Muscular endurance: 12-20 repetitions per set | Full range of flexion, extension, and rotation, or stretching to the point of feeling tension or slight discomfort |
| Time | Cumulative or continuous exercise of ≥ 30 min/day; if done in separate sessions, each session should not be less than 10 min | Muscular strength: 2-4 sets of repetitions Muscular endurance: ≤ 2 sets of repetitions |
Static stretching hold 10-30 s, repeat each movement 2-4 times |
Note: HRR: Heart Rate Reserve; VO2R: Reserve Oxygen Uptake; RPE: Rating of Perceived Exertion; 1RM: Maximum power of 1 Repetition.
Table 1: ACSM exercise recommendations for hypertensive patients.s
The movement indicators were scored on a scale of 0 to 2. 2 representing compliance, 1 representing unsure, and 0 representing non-compliance. In case of disagreement between two authors during the scoring process, a discussion was held with a third author to reach a final consensus. Based on this scale, we calculated the proportion of exercise doses that complied with the ACSM recommendations for exercise doses in hypertensive patients for each study. When the proportion was ≥ 70%, we categorized it as high adherence to ACSM recommendations; when it was <70%, we categorized it as low or uncertain adherence to ACSM recommendations.
Statistical analysis
In this study, meta-analysis was performed to compare the results of the included studies using STATA 16.0 software. The study was divided into two groups, one representing high ACSM adherence and one representing low or uncertain ACSM adherence. Heterogeneity between studies in each subgroup was assessed using the Higgins I2 statistic and interpreted according to the recommendations of the Cochrane Handbook [21]. In the heterogeneity test, a fixed-effects model was used if I2 ≤ 50%, and a random-effects model was used if I2>50%. The effect sizes were expressed as SMD combined with 95% confidence intervals (95% CI). The likelihood of publication bias was assessed by constructing a funnel plot of the standard error effect size for each study, and the funnel plots were evaluated using Beggar’s and Egger's rank correlation method, with p<0.05 set as statistically significant, the study results were tested for robustness by sensitivity analysis with one-by-one exclusion. The effects of subgroup treatments were compared using Higgins I2 statistic, p<0.05 was considered statistically significant.
Literature quality assessment
Two authors Chen, Cui independently evaluated the included literature using the Risk of Bias 2 (RoB 2) tool [22], in accordance with the quality assessment criteria for randomized controlled trials recommended by the Cochrane Systematic Reviews. RoB 2 consists of the following seven evaluation metrics: Random sequence generation, allocation concealment, blindness of the researcher and the researched, blinding of outcome output, incomplete data reporting, selective reporting, and other sources of bias. According to the Cochrane Handbook reviewers' scoring of studies, the risk of bias in each area was categorized into three levels: “Low risk,” “some risk,” and “high risk.” In case of disagreement during the scoring process, it was resolved in consultation with the third author Xie.
Literature search and selection
A total of 36763 articles were obtained through database search, and 19 articles were finally included according to the inclusion criteria through gradual screening [23-41] (Figure 1).
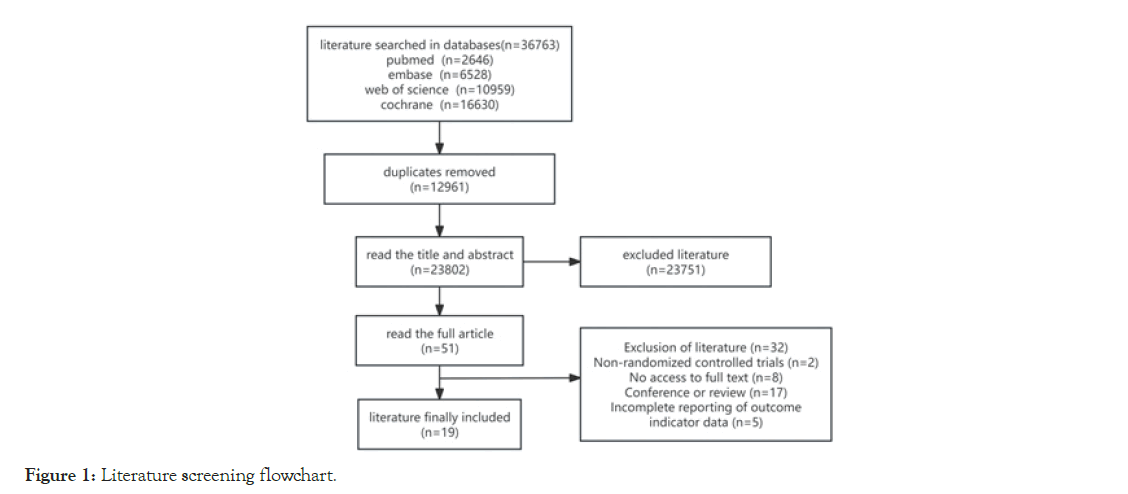
Figure 1: Literature screening flowchart.
Description of the characteristics of the studies
19 papers covering 26 studies with 1458 subjects (762 in the experimental group and 696 in the control group). The study was conducted in 11 countries, including India, Ethiopia, Nigeria, Japan, Switzerland, the Republic of Korea, the United States of America, Thailand, Italy, China and Brazil. The length of intervention was reported as ranging from a minimum of 8 weeks to a maximum of 16 months in 26 studies.
The frequency of exercise reported in the interventions ranged from three to seven times per week. Interventions included running, yoga, walking, tai chi, soccer, cycling, resistance training, taekwondo, and combined exercise. The control group did not undergo exercise intervention, maintained their original lifestyles or underwent usual care (Table 2).
| Author | Nation | sample size | Gender ratio | Age (years) | Disease level | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| T | C | T(M) | T(F) | C(M) | C(F) | T | C | |||
| Santos et al. [23] | Brazil | 20 | 20 | 0 | 20 | 0 | 20 | 64.20 ± 3.10 | 63.10 ± 2.30 | Hypertension stage 1-2 |
| Santos et al. [23] | Brazil | 20 | 20 | 0 | 20 | 0 | 20 | 62.60 ± 2.50 | 63.10 ± 2.30 | Hypertension stage 1-2 |
| Thiyagarajan et al. [24] | India | 51 | 49 | 31 | 20 | 31 | 18 | 44.08 ± 9.42 | 42.47 ± 9.00 | Prehypertension |
| Arca et al. [25] | Brazil | 19 | 14 | 0 | 19 | 0 | 14 | NR | NR | NR |
| Arca et al. [25] | Brazil | 19 | 14 | 0 | 19 | 0 | 14 | NR | NR | NR |
| Tsai et al. [26] | China, Taiwan | 12 | 11 | 7 | 5 | 5 | 6 | 49.60 ± 9.30 | 46.20 ± 5.60 | Mild hypertension |
| Seals et al. [27] | USA | 18 | 17 | 0 | 18 | 0 | 17 | 62 ± 9.00 | 65 ± 10.00 | Hypertension stage 1 |
| Daimo M et al [28] | Ethiopia | 23 | 23 | NR | NR | NR | NR | 38.80 ± 4.30 | 38.30 ± 4.20 | Hypertension stage 1 |
| Ruangthai et al. [29] | Thailand | 13 | 12 | 1 | 12 | 5 | 7 | 65.60 ± 4.50 | 66.70 ± 5.80 | NR |
| Ruangthai et al. [29] | Thailand | 13 | 12 | 0 | 13 | 5 | 7 | 68.00 ± 7.40 | 66.70 ± 5.80 | NR |
| Ruangthai et al. [29] | Thailand | 16 | 12 | 5 | 11 | 5 | 7 | 67.30 ± 5.90 | 66.70 ± 5.80 | NR |
| Dantas et al. [30] | Brazil | 13 | 12 | 0 | 13 | 0 | 12 | NR | NR | NR |
| Shou et al. [31] | China | 98 | 100 | 48 | 50 | 55 | 45 | NR | NR | Hypertension stage 1 |
| Church et al. [32] | USA | 103 | 102 | 0 | 103 | 0 | 102 | 56.60 ± 6.60 | 57.20 ± 5.80 | NR |
| Venturelli et al. [33] | Italy | 10 | 10 | 5 | 5 | 5 | 5 | 68.00 ± 3.00 | 66.00 ± 7.00 | Hypertension stage 1 |
| Venturelli et al. [33] | Italy | 10 | 10 | 5 | 5 | 5 | 5 | 67.00 ± 4.00 | 66.00 ± 7.00 | Hypertension stage 1 |
| Venturelli et al. [33] | Italy | 10 | 10 | 5 | 5 | 5 | 5 | 69.00 ± 6.00 | 66.00 ± 7.00 | Hypertension stage 1 |
| Knoepfli-Lenzin et al. [34] | Switzerland | 15 | 17 | 15 | 0 | 17 | 0 | NR | NR | Mild hypertension |
| Knoepfli-Lenzin et al. [34] | Switzerland | 15 | 17 | 15 | 0 | 17 | 0 | NR | NR | Mild hypertension |
| Lee et al. [35] | Korea | 17 | 19 | 8 | 9 | 6 | 13 | 52.60 ± 5.10 | 54.30 ± 5.50 | Mild to moderate hypertension |
| Kim et al. [36] | Korea | 10 | 10 | 0 | 10 | 0 | 10 | 72.90 ± 5.84 | 71.90 ± 3.11 | NR |
| Farinatti et al. [37] | Brazil | 29 | 14 | 7 | 22 | 5 | 9 | 53.00 ± 11.00 | 48.00 ± 5.00 | NR |
| Higashi et al. [38] | Japan | 10 | 7 | 7 | 3 | 6 | 1 | NR | NR | Mild Hypertension |
| Tsai et al. [39] | Taiwan, China | 37 | 39 | 19 | 18 | 19 | 20 | 51.6 ± 16.3 | 50.50 ± 9.80 | Hypertension stage 1 |
| Zheng et al. [40] | China | 21 | 20 | 6 | 15 | 7 | 13 | 65.19+6.47 | 60.70+8.03 | Hypertension stage 1-2 |
| Lamina et al. [41] | Nigeria | 140 | 105 | 140 | 0 | 105 | 0 | 58.90 ± 7.35 | 58.27 ± 6.24 | Mild to moderate hypertension |
Note: T:Test sample; C:Control; T/M: Ratio of Test to gender(Male); T/F: Ratio of Test to gender (Female); C/M: Ratio of Control to gender(Male); C/F: Ratio of Control to gender(Female)
Table 2: Overview of general characteristics of the study and participants.
After categorizing the interventions according to the ACSM recommendations, this study classified qigong, yoga, tai chi, taekwondo, and walking combined with stretching as aerobic and flexibility exercises; Soccer, running, cycling and walking were categorized as aerobic exercises; Two studies used endurance training and combined endurance strength training, which also involved flexibility stretching exercises; Four studies used strength resistance training; three studies used resistance combined with aerobic combined exercise.
Therefore, a total of 24 studies included an exercise dose for aerobic exercise, 6 studies involved an exercise dose for resistance exercise, and 9 studies involved an exercise dose for flexibility exercise (Table3).
| Author | Interventions | Length of intervention | TC | TG | HDL | LDL |
|---|---|---|---|---|---|---|
| Santos et al. [23] | Traditional resistance combined aerobic training | 16 weeks | √ | √ | √ | √ |
| Santos et al. [23] | Centrifugal resistance combined aerobic training | 16 weeks | √ | √ | √ | √ |
| Thiyagarajan et al. [24] | Yoga | 12 weeks | √ | √ | √ | √ |
| Arca et al. [25] | Water aerobics | 12 weeks | √ | √ | √ | √ |
| Arca et al. [25] | Dryland aerobics | 12 weeks | √ | √ | √ | √ |
| Tsai et al. [26] | Tai chi | 12 weeks | √ | √ | √ | √ |
| Seals et al. [27] | Walking | 12 weeks | √ | √ | √ | √ |
| Daimo M et al [28] | Aerobic combined resistance training | 16 weeks | √ | √ | √ | √ |
| Ruangthai et al. [29] | Endurance training | 12 weeks | √ | √ | √ | √ |
| Ruangthai et al. [29] | Strength training | 12 weeks | √ | √ | √ | √ |
| Ruangthai et al. [29] | Endurance and strength | 12 weeks | √ | √ | √ | √ |
| Dantas et al. [30] | Strength training | 10 weeks | √ | √ | √ | √ |
| Shou et al. [31] | 24-style simplified taijiquan | 3 months | √ | √ | √ | √ |
| Church et al. [32] | Running | 6 months | - | √ | √ | √ |
| Venturelli et al. [33] | Endurance training | 12 weeks | - | - | √ | √ |
| Venturelli et al. [33] | Circuit training | 12 weeks | - | - | √ | √ |
| Venturelli et al. [33] | Relaxation training | 12 weeks | - | - | √ | √ |
| Knoepfli-Lenzin et al. [34] | Soccer | 12 weeks | √ | - | √ | √ |
| Knoepfli-Lenzin et al. [34] | Running | 12 weeks | √ | - | √ | √ |
| Lee et al. [35] | Qigong | 8 weeks | √ | √ | √ | - |
| Kim et al. [36] | Taekwando | 12 weeks | √ | √ | √ | √ |
| Farinatti et al. [37] | Walking and stretching | 16 months | √ | √ | √ | √ |
| Higashi et al. [38] | Aerobics | 12 weeks | √ | √ | √ | √ |
| Tsai et al. [39] | Tai chi | 12 weeks | √ | √ | √ | √ |
| Zheng et al. [40] | Liuzijue | 12 weeks | √ | √ | √ | √ |
| Lamina et al. [41] | Interval training | 8 weeks | √ | - | √ | - |
Table 3: Characteristics of the study intervention.
Methodological quality assessment
19 studies were randomized controlled trials, therefore considered as low risk of bias. Regarding allocation concealment, 7 studies clearly reported allocation methods, therefore considered to have a low risk of bias for allocation concealment. In comparison, 12 studies did not clearly report allocation concealment, so this indicator's overall risk of bias was relatively high.
Regarding blinding of investigators and subjects, 13 studies were considered at some risk of bias because they did not explicitly report blinding of investigators and subjects.
In the blinded assessment of outcomes, 7 studies were assessed using randomized testing, professional staff, and blinded assessors, therefore considered as low risk; 12 studies did not mention that the method of assessing outcomes was of some risk.
Regarding the incomplete reports of outcomes, 8 studies had a post-experimental number of subjects that were consistent or virtually consistent with baseline, thus, we considered them to be at low risk; 3 studies had a small number of subjects withdrawing (5-10) and thus were considered to be at some risk; and 8 studies had a sizeable pre-post difference in the number of subjects (more than 10) and thus were considered to be at high risk.
Additionally, 10 studies were considered risky in selective reporting because they did not include an enrollment protocol or did not detail the reasons for subject attrition (Figure 2).
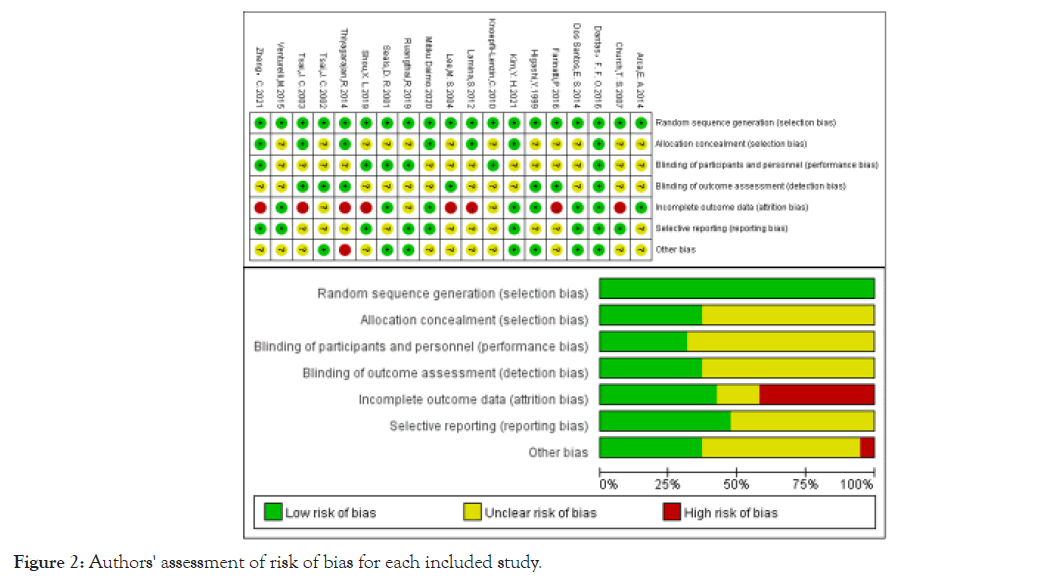
Figure 2: Authors' assessment of risk of bias for each included study.
Adherence to ACSM: 8 of the 26 studies had adherence to ACSM recommendations greater than 70%, and 18 studies had adherence to ACSM less than or equal to 70%. The reasons for the low adherence were, on the one hand, due to the dosage of exercise interventions that did not match the ACSM recommendations, such as insufficient number of exercises per week, excessive exercise intensity, and on the other hand, due to the fact that the text did not provide sufficiently clear and detailed information about the exercise program for proper assessment (Table 4).
| Author | Aerobics exercise | Resistance exercise | Flexibility exercise | ACSM compliance | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency (day/week) | Intensity/ work load | Duration (min) | Frequency (day/week) | Intensity/ work load | Repetition (times) | Sets (groups) | Frequency (day/week) | Intensity/ work load | Duration | Points | Percent | |
| Santos et al. [23] | 3 |  65-75 HRmax 65-75 HRmax |
 20 20 |
 3 3 |
 70-9010 RM 70-9010 RM |
 10 10 |
 |
3  |
- | - | 7/14 | 50 |
| Santos et al. [23] | 3 |  65-75 HRmax 65-75 HRmax |
 20 20 |
 3 3 |
 100-12010 RM 100-12010 RM |
 10 10 |
 |
3  |
- | - | 6/14 | 43 |
| Thiyagarajan et al. [24] | 3 |  NR NR |
 45 45 |
 |
- | - | - | 3  |
Full range of flexion |  NR NR |
 8/12 8/12 |
67 |
| Arca et al. [25] | 3 |  50-60 HRR 50-60 HRR |
 50 50 |
 |
- | - | - | - | - | - | 4/6 | 67 |
| Arca et al. [25] | 3 |  50-60 HRR 50-60 HRR |
 50 50 |
 |
- | - | - | - | - | - | 4/6 | 67 |
| Tsai et al. [26] | 3 |  64 HRmax 64 HRmax |
 50 50 |
 |
- | - | - | 3  |
Full range of flexion |  NR NR |
 7/12 7/12 |
58 |
| Seals et al. [27] | 3 |  40-80 HRmax 40-80 HRmax |
 30-45 30-45 |
 |
- | - | - | - | - | - | 3/6 | 50 |
| Daimo M et al [28] | 3 |  RPE9--13 RPE9--13 |
 23 23 |
 3 3 |
 1RM 30-60 1RM 30-60 |
 8 moves 8 moves |
 |
NR  |
- | - | 7/14 | 50 |
| Ruangthai et al. [29] | 3 |  50-70 HRmax 50-70 HRmax |
 60 60 |
 |
- | - | - | - | Total body stretch |  10min 10min |
 9/12 9/12 |
75 |
| Ruangthai et al. [29] | - | - | - | 3 |  1RM 50-80 1RM 50-80 |
 10 to 15 10 to 15 |
 |
3  |
- | - | 8/8 | 100 |
| Ruangthai et al. [29] | 3 |  50-70 HRmax 50-70 HRmax |
 20 20 |
 3 3 |
 1RM 50-80 1RM 50-80 |
 12 12 |
 |
2  |
Total body stretch |  10min 10min |
 15/20 15/20 |
75 |
| Dantas et al. [30] | - | - | - | 2-3 |  NR NR |
 9 moves 9 moves |
 |
NR  |
- | - | 5/8 | 63 |
| Shou et al. [31] | 7 | J50-60VO2max |  40-90 40-90 |
 |
- | - | - | 7  |
Full range of flexion |  2-4 times 2-4 times |
 12/12 12/12 |
100 |
| Church et al. [32] | 3-4 |  50VO2max 50VO2max |
 NR NR |
 |
- | - | - | - | - | - | 3/6 | 50 |
| Venturelli et al. [33] | 3 |  70Max exercise 70Max exercise |
 60 60 |
 |
- - |
- | - | - | - | - - |
2/6 | 33 |
| Venturelli et al. [33] | 3 |  70Max mechanical power 70Max mechanical power |
 60 60 |
 |
- | - | - | - | - | - | 2/6 | 33 |
| Venturelli et al. [33] | 3 |  NR NR |
 60 60 |
 |
- | - | - | - | - | - | 3/6 | 50 |
| Knoepfli-Lenzin et al. [34] | 3 |  65 HRmax 65 HRmax |
 60 60 |
 |
- | - | - | - | - | - | 2/6 | 33 |
| Knoepfli-Lenzin et al. [34] | 3 |  80 HRmax 80 HRmax |
 60 60 |
 |
- | - | - | - | - | - | 2/6 | 33 |
| Lee et al. [35] | 2 |  50-60Max exercise 50-60Max exercise |
 30 30 |
 |
- | - | - | 2 |
Full range of flexion |  NR NR |
 9/12 9/12 |
75 |
| Kim et al. [36] | 3 |  40-75HRR 40-75HRR |
 90 90 |
 |
- | - | - | 3  |
Total body stretch |  10min 10min |
 9/12 9/12 |
75 |
| Farinatti et al. [37] | 3 |  60-85HRmax 60-85HRmax |
 30 30 |
 |
- | - | - | 3 |
Total body stretch |  NR NR |
 8/12 8/12 |
67 |
| Higashi et al. [38] | 5 | J 43-61 VO2max |  30 30 |
 |
- | - | - | - | - | - | 5/12 | 83 |
| Tsai et al. [39] | 3 |  60-70HRmax 60-70HRmax |
 50 50 |
 |
- | - | - | - | - | - | 3/ 6 | 50 |
| Zheng et al. [40] | 3 |  NR NR |
 60 60 |
 |
- | - | - | 3  |
Total body stretch |  10min 10min |
 9/12 9/12 |
75 |
| Lamina et al. [41] | 3 |  60-79HRR 60-79HRR |
 45-60 45-60 |
 |
- | - | - | - | - | - | 3/6 | 50 |
Note: HRR: Reserve Heart Rate; HR: Heart Rate; VO2R: Reserve Oxygen uptake; RPE: Rating of Perceived Exertion; 1RM: Maximum power of 1 repetition; NR: Not Reported; ( ): Fulfils recommendation (2 points); (
): Fulfils recommendation (2 points); ( ): uncertain fulfilment (1 point), (
): uncertain fulfilment (1 point), ( ): does not fulfil recommendation (0 points).
): does not fulfil recommendation (0 points).
Table 4: Assessment of ACSM adherence.
Analyze the adherence percentage from the perspective of the study indicators: 22 studies included TC indicators, with 8 studies had high adherence to ACSM and 14 studies had low or uncertain adherence; 20 studies included TG indicators, of which 8 had high ACSM adherence and 12 had low or uncertain ACSM adherence; 26 studies included HDL indicators, of which 8 had high ACSM adherence and 18 had low or uncertain adherence; and 24 studies included LDL indicators, of which 7 had high ACSM adherence and 17 had low or uncertain adherence.
Meta-analysis
Analysis of TC: When the study outcome was TC, we analyzed 1193 subjects from 22 studies. Firstly, we found that I2 was less than 50% (I2=41.6%, p=0.022), so we used a fixed effect model for statistical analysis, Data analysis revealed the total combined SMD was (95%CI: -0.60, -0.37), suggests that exercise interventions are effective for TC in hypertensive patients. In the subgroup analysis, we grouped the subgroups based on the proportion of adherence to ACSM recommendations. The SMD for the subgroup with high adherence to ACSM recommendations was -0.46 (95%CI: -0.67, -0.37), for the subgroup with low or uncertain adherence to ACSM, the SMD was -0.50 (95%CI: -0.64, -0.35). The subgroup difference test showed that there was no significant difference between interventions with high ACSM adherence and those with low or indeterminate ACSM adherence in terms of improvement of TC in patients with hypertension (Figure 3).
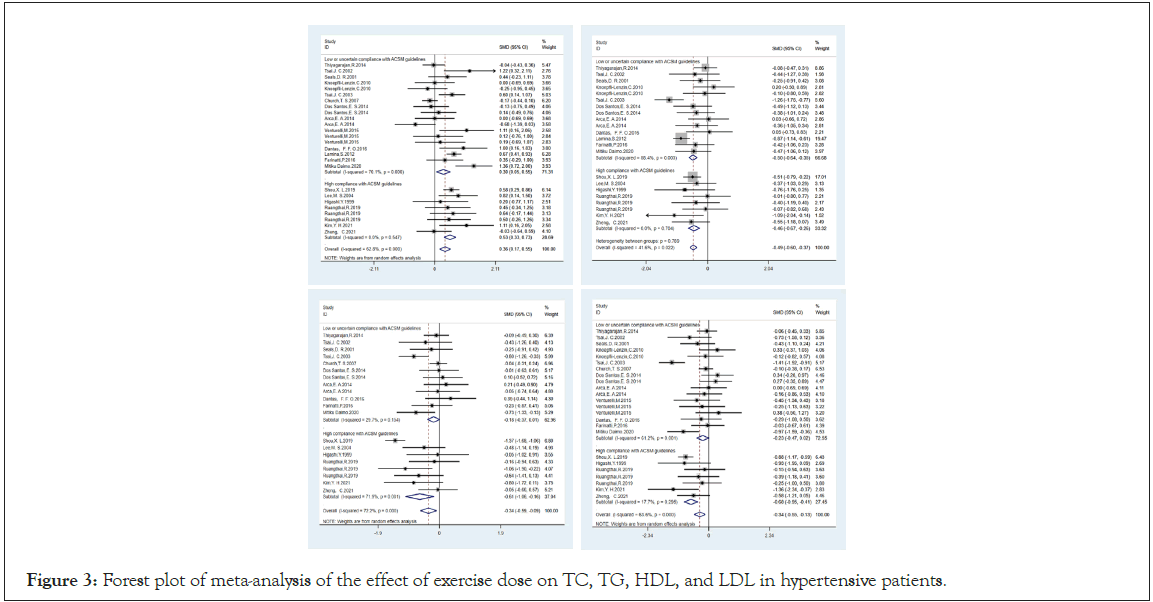
Figure 3: Forest plot of meta-analysis of the effect of exercise dose on TC, TG, HDL, and LDL in hypertensive patients.
By inspection of the funnel plot (Figure 4A), it was found that both sides of the funnel plot were roughly symmetrical. There was no significant publication bias, and we verified again that there was no significant publication bias by using Beggar’s (p=0.176) and Egger’s (p=0.061), Then, we found by sensitivity analysis (Figure 5A) that none of the articles had a large impact on the overall results, and the results were considered robust.
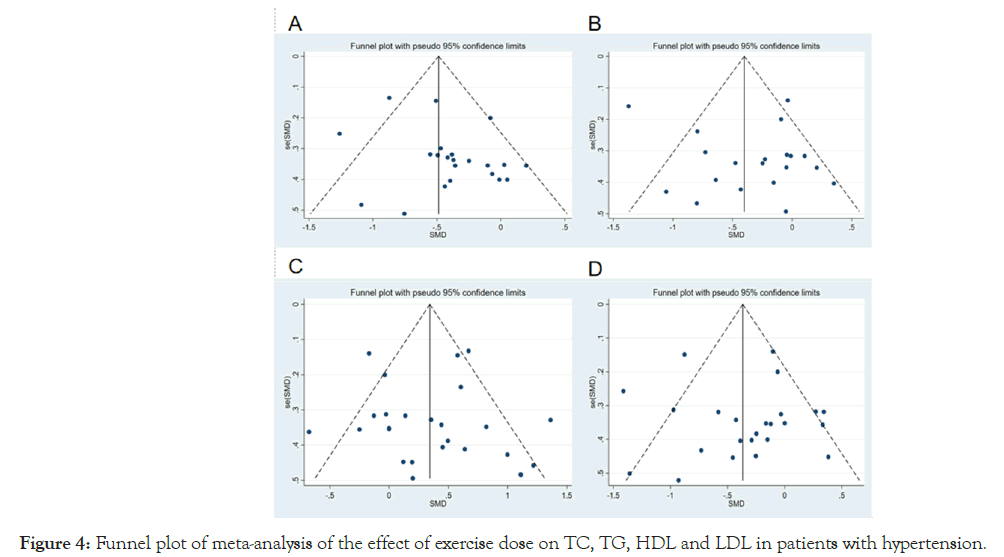
Figure 4: Funnel plot of meta-analysis of the effect of exercise dose on TC, TG, HDL and LDL in patients with hypertension.
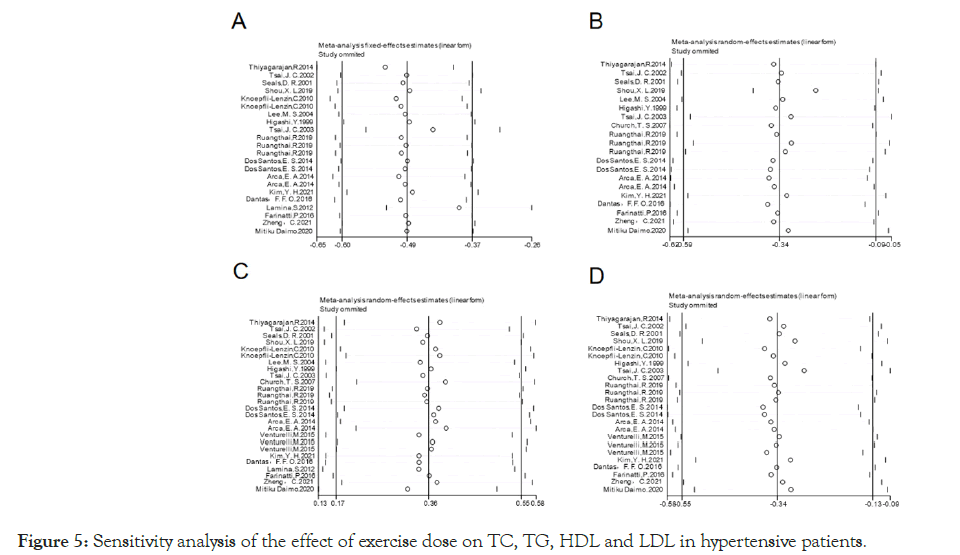
Figure 5: Sensitivity analysis of the effect of exercise dose on TC, TG, HDL and LDL in hypertensive patients.
Analysis of TG: When the study outcome was TG, we analyzed 1089 subjects from 20 studies. Firstly, we found that I2 was more than 50% (I2=72.2%, p=0.000) by heterogeneity test, so we used the random effect model for statistical analysis. Data analysis revealed the total combined SMD was -0.34 (95%CI: -0.59, -0.09), Suggests that exercise interventions are effective for TG in hypertensive patients. In the subgroup analysis, we grouped the subgroups based on the proportion of adherence to ACSM recommendations.
The SMD for the subgroup with high adherence to ACSM recommendations was -0.61 (95%CI: -1.06, -0.16), for the subgroup with low or uncertain adherence to ACSM, the SMD was -0.18 (95%CI: -0.37, -0.01). The subgroup difference test showed a significant difference between the study interventions with high ACSM adherence and those with low or uncertain ACSM adherence (Figure 3). Therefore, we concluded that exercise with high ACSM adherence was superior to exercise interventions with low or uncertain ACSM adherence for the treatment of TG in hypertensive patients.
By visual inspection of the funnel plot (Figure 4B), it was found that both sides of the funnel plot were roughly symmetrical. There was no significant publication bias, and we verified again that there was no significant publication bias by using Beggar’s (p=0.770) and Egger’s (p=0.89), Then, we found by sensitivity analysis (Figure 5B) that none of the articles had a large impact on the overall results, and the results were considered robust.
Analysis of HDL: When the study outcome was HDL, we analyzed 1458 subjects from 26 studies. We found that I2 was more than 50% (I2=62.8%, p=0.000) by heterogeneity test, so we used the random effect model for statistical analysis. Data analysis revealed the total combined SMD was 0.36 (95%CI: 0.17, 0.55), Suggests that exercise interventions are effective for HDL in hypertensive patients. In the subgroup analysis, we grouped the subgroups based on the proportion of adherence to ACSM recommendations. The SMD for the subgroup with high adherence to ACSM recommendations was 0.53(95%CI: 0.33, 0.73), for the subgroup with low or uncertain adherence to ACSM, the SMD was 0.30 (95%CI: 0.05, 0.55). The subgroup difference test showed a significant difference between the study interventions with high ACSM adherence and those with low or uncertain ACSM adherence (Figure 3). Therefore, we concluded that exercise with high ACSM adherence was superior to exercise interventions with low or uncertain ACSM adherence for the treatment of HDL in hypertensive patients.
By visual inspection of the funnel plot (Figure 4C), it was found that both sides of the funnel plot were roughly symmetrical. There was no significant publication bias, and we verified again that there was no significant publication bias by using Beggar’s (p=0.217) and Egger’s (p=0.667), Then, we found by sensitivity analysis (Figure 5C) that none of the articles had a large impact on the overall results, and the results were considered robust.
Analysis of LDL: When the study outcome was LDL, we analyzed 1177 subjects from 24 studies. We found that I2 was more than 50% (I2=63.6%, p=0.000) by heterogeneity test, so we used the random effect model for statistical analysis. Data analysis revealed the total combined SMD was -0.34 (95%CI: -0.55, -0.13), suggests that exercise interventions are effective for LDL in hypertensive patients. In the subgroup analysis, we grouped the subgroups based on the proportion of adherence to ACSM recommendations. The SMD for the subgroup with high adherence to ACSM recommendations was -0.68 (95%CI: -0.95, -0.41), for the subgroup with low or uncertain adherence to ACSM, the SMD was -0.23 (95%CI: -0.47, 0.02). The subgroup difference test showed a significant difference between the study interventions with high ACSM adherence and those with low or uncertain ACSM adherence (Figure 3). Therefore, we concluded that exercise with high ACSM adherence was superior to exercise interventions with low or uncertain ACSM adherence for the treatment of LDL in hypertensive patients.
By visual inspection of the funnel plot (Figure 4D), it was found that both sides of the funnel plot were roughly symmetrical. There was no significant publication bias, and we verified again that there was no significant publication bias by using Beggar’s (p=0.172) and Egger’s (P=0.664). Then, we found by sensitivity analysis (Figure 5D) that none of the articles had a large impact on the overall results, and the results were considered robust.
This systematic review and meta-analysis was based on the ACSM recommendations for exercise in hypertensive patients, and analyzed 26 randomized controlled trials covering 1,458 participants from different geographic regions and ethnic populations to explore the effects of high adherence to the ACSM and low or uncertain adherence to the ACSM on TC, TG, HDL, and LDL in hypertensive patients. The present study showed that exercise intervention with high adherence to ACSM was significantly more effective in lowering TG and LDL, and elevating HDL in hypertensive patients than exercise doses with low or uncertain adherence to ACSM, whereas the improvement in TC was not significant.
Different intervention modalities have different effects on hypertensive patients, and our study found that qigong, taekwondo, tai chi, and aerobic combined resistance exercise modalities had better improvement effects on hypertensive patients. This is consistent with the findings of previous studies [42-52]. Yin concluded that tai chi exercise cycles of more than 5 times per week for more than 12 weeks were more beneficial to lowering blood pressure and improving lipid metabolism by comparing the effects of different tai chi exercise cycles on hypertension [53], this fits with our findings [31]. We believe that the frequency of exercise has an important influence on the improvement of blood lipids in hypertensive patients. In most of the 26 studies we included, the frequency of exercise was 3 times per week, whereas the ACSM recommended frequency of exercise for hypertensive patients is 5-7 times per week, and the low frequency of exercise weeks resulted in a slightly poorer effect of the exercise interventions, which is one of the main reasons why most of the studies were categorized as having low or uncertain adherence to exercise by the ACSM.
There were some limitations in the research process, which may also lead to the bias of the final results. First, one studies did not have direct data among the final included literature. We used Engauge Digitizer software to extract the data from the graphs and tables in the text, and the final data of the two studies were expressed as Mean ± SE values, we converted them into Mean ± SD values, and the errors were unavoidable when extracting or converting the data, although the data were preserved as much as possible. Second, the included studies included different modalities of exercise training such as tai chi, qigong, soccer, and resistance exercise, and there may be relatively high heterogeneity among these studies. Third, this study was based on the ACSM's exercise recommendations for hypertensive patients, and the adherence to the exercise intervention programs included in the study was assessed. The ACSM's recommended exercise prescriptions for hypertensive patients include aerobic, resistance, and flexibility exercises [20],
Each of these described the recommended exercise dose in detail, including frequency, intensity, and duration of exercise. However, of the 26 randomized controlled trials included, 8 studies did not describe the exercise dose comprehensively, and unclear reporting may have biased the classification of adherence somewhat.
This article supports the idea that exercise is an effective measure to improve lipid levels in hypertensive patients, and our findings are again consistent with this conclusion. In analyzing the optimal dose of exercise in hypertensive patients, we found that exercise interventions with a high adherence to ACSM showed more significant improvements in TG, HDL, and LDL but less significant improvements in TC than those with low or uncertain adherence to ACSM. In addition, because of the lack of information on some of the included studies' exercise intervention programs, more randomized controlled trials with larger sample sizes are needed for future validation.
JC conceived and designed the study. JC and WLC did the screening of the title and abstract. Disputes were resolved by JX. Data inclusion was carried out by JC and WLC.JC and JX scored adherence to the ACSM recommended dose of each exercise intervention separately. All authors participated in the quality assessment of the included literature. JC and WLC completed the first draft of the manuscript. All authors advised on the article and approved the submitted version.
This study was funded by the "China Association for Science and Technology Project: Research on Content Guidelines for Health Science Promotion (No. kpbwh-2021-2-6).
The data supporting the conclusions in the study are included within the article and the additional file, further inquiries can be directed to the corresponding author.
All authors contributed to this study.
The authors declare that the study was conducted without any business or financial relationship that could be interpreted as a potential conflict of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Mierina K, Millere E (2024). The Effect of Exercise Dose on Blood Lipid in Hypertensive Patients Based on ACSM Recommendations: A Meta-Analysis. Angiol Open Access. 12:476.
Received: 05-Aug-2024, Manuscript No. AOA-24-33371; Editor assigned: 08-Aug-2024, Pre QC No. AOA-24-33371 (PQ); Reviewed: 22-Aug-2024, QC No. AOA-24-33371; Revised: 29-Aug-2024, Manuscript No. AOA-24-33371 (R); Published: 05-Sep-2024 , DOI: 10.35841/2329-9495.24.12.476.
Copyright: © 2024 Mierina K et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.