Journal of Clinical and Experimental Ophthalmology
Open Access
ISSN: 2155-9570
ISSN: 2155-9570
Research - (2020)Volume 11, Issue 6
Aim: This study assesses the impact of the UK COVID-19 lockdown on Ophthalmology Emergency Services at one of the largest dedicated Emergency Eye Departments in the UK.
Methods: We evaluated differences in attendances between 2019 and 2020 according to ethnicity, deprivation scores, age, clinician grade, diagnosis, discharge rate and follow up length.
Results: The mean number of attendances started to drop on the 17th March 2020. The mean number of attendances before versus after 17th March decreased by a factor of 2.2 with a 95% (CR) of (2.1,2.3); from 72 (95%CR 70,75) per day to 33 (95%CR 31,35). Attendance rates to the Emergency Eye Department during a 9-week period of lockdown dropped by 51% (95%CI 47-52%) compared with the same period in 2019 and 48% (95% CI50-54%) compared with 2018. There was no significant difference in patient age, ethnicity or index of deprivation quintile between 2019 and 2020.
There was a 61% drop (95% CI 48-70%) in the number of eye emergencies presenting in the second week of lockdown (30/04/2020–05/04/2020) compared to the corresponding period in 2019. Community eye emergencies dropped by 74% (95%CI 64-80%) and non-eye emergencies dropped by 64% (95%CI 47-75%).
Conclusion: Government measures to reduce the transmission of COVID-19 have had a significant impact on the attendance of patients to our Emergency Eye Department. Severe blinding conditions are not presenting as frequently. This raises the concern that once the restrictions of COVID-19 are fully lifted some patients might start to present with potentially incurable chronic ocular conditions with devastating secondary complications.
COVID-19; Ophthalmology; Lockdown
The first confirmed cases of COVID-19 pneumonia were identified in Wuhan, China in December 2019. This coronavirus has spread rapidly across the world, being formally classified as a pandemic by the WHO on 11th March 2020 [1]. Governments have placed unprecedented measures to limit the rate of transmission of COVID-19. The UK Government’s response was to gradually increase restrictions. This began on the 7th March 2020 asking anyone with symptoms of a dry cough or a raised temperature to self-isolate for 7 days. The most vulnerable groups were asked to shield and the whole population was instructed to cease non-essential travel on the 16th March 2020. Schools were closed on the 18th March followed by the closure of hospitality, entertainment and leisure centres on the 20th March. Then a formal lockdown was implemented on the 23rd March 2020 [2]. The lockdown instructions covered three areas; requiring people to stay at home, except for limited purposes, closing certain businesses and venues and stopping gatherings of more than two people in public [3].
As a consequence of the lockdown many workplaces closed, there was a restriction on free movement of millions of people and social contact was limited to the household. These changes have been deemed necessary to reduce transmission rates. The NHS has redistributed manpower to the front-line services to manage COVID-19 patients. The Royal College of Ophthalmologists advise all face-to-face outpatient activity should be postponed unless patients are at high risk of rapid, significant harm if their appointment is delayed. However, The Royal College of Ophthalmologists states that ophthalmology A&E services should stay open with consultant level support for both triage and directly assessing patients [4]. These changes could increase demand at A&E services as without routine provision of care their condition may worsen and therefore need to attend A&E.
The aim of this study is to review the impact of this state of emergency on the Ophthalmology Emergency Service. This will help identify several areas for future planning to manage the progression of this COVID-19 pandemic or even future pandemics.
A single centre retrospective observational study was performed at Manchester Royal Eye Hospital, United Kingdom.
This is one of the largest tertiary referral centres with a dedicated Emergency Eye Department (EED). The EED is open 12 hours a day from 8 AM to 8 PM. Patients are seen either after being referred by another health care provider or the patients selfpresent with an eye condition. The EED is staffed with Nurse Practitioners, trainee Ophthalmologists, Ophthalmic subspecialty Fellows, Staff Grade clinicians, Optometrists and Consultant Ophthalmologists.
Data was obtained from electronic records departmental software (Symphony, Emis Health, EMIS Group, Leeds, UK) alongside their paper based patient records.
Daily attendance figures to the EED from 10/02/2020 to 17/05/2020 were recorded to see how attendances changed from prior to during lockdown. Attendance figures for the same period in 2018 and 2019 were obtained for comparison.
Patient demographics were collected for each patient attending the EED over a 9-week period of lockdown in 2020 (23/03/2020 – 24/05/2020) and a corresponding 9-week period in 2019 (25/03/2019 – 26/05/2019). For each patient their age, ethnicity and postcode were recorded. From their postcode each patient’s Index of Multiple Deprivation Quintile was obtained from the Ministry of Housing, Communities & Local Government Postcode Lookup tool [5]. This score gives an indication of each patient’s level of deprivation from 1 (most deprived) to 10 (least deprived) based upon their residential post code.
The clinical record of each patient that attended the EED for the second week of lockdown (30/03/2020 – 05/04/2020) and a corresponding week in 2019 (01/04/2019) was reviewed. The formal diagnosis, grade of clinician assessing the patient, requirement for follow up from the EED visit and length of follow up, if required, was recorded. Each ophthalmic diagnosis was then triaged into one of three categories – Eye Emergencies, Community Emergencies, Non-Eye Emergencies. Eye Emergencies were classified as a diagnosis which should be managed under the care of an Ophthalmologist in an Emergency Eye Department. Community Emergencies are ophthalmic diagnoses that can be managed in the community by General Practitioners, Optometrists or Community Pharmacists. Non Eye Emergencies are diagnoses which are not considered to need urgent assessment and management. For the grading of each individual diagnosis please see the supplementary online material.
We first modelled the number of attendances from 10/02/2020 to 17/05/2020 using a Bayesian Poisson model with non-informative priors for the parameters: flat priors for the mean attendances and a uniform distribution on (10th February 19th April) for the change point. 10,000 MCMC iterations were used and model diagnostics checked for convergence. The estimated changepoint from this model was the date at which the number of attendances began to change.
We then evaluated the proportion of attendances in 2019 and 2020 according to age, ethnicity, Index of Multiple Deprivation Quintile, grade of clinician, and case mix (eye emergencies, community emergencies, non-eye emergencies) using chi-squared tests for differences in proportions.
In 2020 the number of attendances to the EED was reduced. The estimated date the attendances started to decrease was the 17th March. The mean number of attendances before versus after 17th March decreased by a factor of 2.2 with a 95% credible range of (2.1, 2.3); from 72 (95% 70, 75) per day to 33 (95% CR 31, 35) (Figure 1).
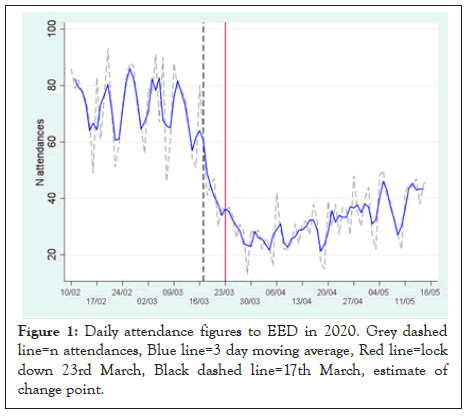
Figure 1: Daily attendance figures to EED in 2020. Grey dashed line=n attendances, Blue line=3 day moving average, Red line=lock down 23rd March, Black dashed line=17th March, estimate of change point.
Attendance rates during the first 9 weeks of lockdown in 2020 (23/03/2020 – 24/05/2020) were compared to the corresponding 9 weeks of 2018 and 2019. The mean number of attendances fell by 51% (95% CI 47-52%) in 2020 compared with the same period in 2019 and 48% (95% CI 50-54%) compared with 2018 (Figure 2).
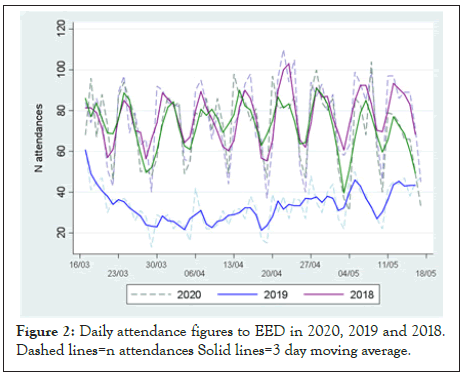
Figure 2: Daily attendance figures to EED in 2020, 2019 and 2018. Dashed lines=n attendances Solid lines=3 day moving average.
Over the first 9 weeks of lockdown (23/03/2020 – 24/05/2020) 2094 patients attended the EED. In the corresponding period in 2019 (25/03/2019 – 26/05/2019) 4792 patients attended. Full data sets of age, ethnicity and Index of Multiple Deprivation Quintile were obtained for all patients. The age distribution of patients has shifted between 2019 and 2020, with a trend to younger (<20 years) and older patients (>70 years) less likely to attend. However, the difference between years did not reach statistical significance (p=0.0621). There was no difference in ethnic group (p=0.408) or Index of Multiple Deprivation Quintile (p=0.129) between the years.
In the second week of lockdown (30/03/2020 – 05/04/2020) 172 patients attended the EED. In the corresponding week in 2019 (01/04/2019 – 07/04/2019) 517 patients attended. Comparing the years there is a difference in the grade of clinician who is seeing each patient (p<0.001). More patients are being seen by Consultants (7.4% in 2019 and 15.7% in 2020) and Fellows (7% in 2019 and 13% in 2020). Trainee ophthalmologists are seeing a similar proportion, 55% in 2019 and 51% in 2020. Less patients are being seen by Nurse Practitioners 29% in 2019 and 17% in 2020. In 2019, 68% (95% CI 64-72%) of patients were discharged compared with 73% (95% CI 66-79%) in 2020. The difference was not significant (p=0.207). The average (median) follow up time in 2019 was 7 days, compared with 14 days in 2020, although this difference was not significant (p=0.275).
The case mix of patients attending in the second week of lockdown in 2020 (30/03/2020-05/04/2020) was similar to the corresponding period in 2019 (01/04/2019-07/04/2019). There were similar proportions of Eye Emergencies, Community Emergencies and Non-Eye Emergencies. However, the total number of attendances reduced significantly between years in all categories. Eye Emergencies reduced from 190 cases in 2019 to 75 cases in 2020. This is a reduction of 61% (95% confidence interval [CI] 48-70%). Community Emergencies dropped from 209 cases in 2019 to 55 cases in 2020, a reduction of 74% (95% CI 64-80%). Non eye emergencies dropped from 107 cases in 2019 to 39 cases in 2020, a reduction of 64% (95% CI 47-75%) (Figure 3).
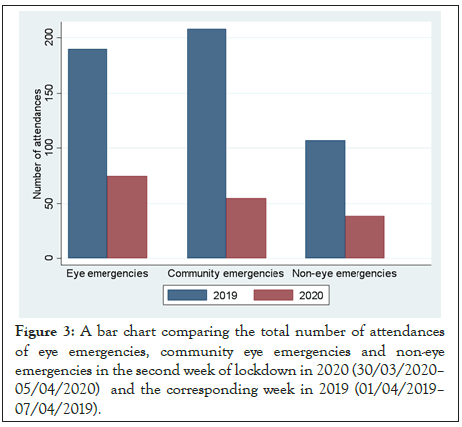
Figure 3: A bar chart comparing the total number of attendances of eye emergencies, community eye emergencies and non-eye emergencies in the second week of lockdown in 2020 (30/03/2020– 05/04/2020) and the corresponding week in 2019 (01/04/2019– 07/04/2019).
There was no change in the proportion of ocular trauma cases from 2019 to 2020 however the total number of cases had reduced. There were 72 cases of ocular trauma in 2019 and 23 in 2020. The top ten most common diagnoses for each year are shown in Table 1. Examples of the number of presentations of different eye emergencies for 2019 and 2020 are shown in Table 2.
| Top diagnosis | 2019-n (%) | 2020-n (%) |
|---|---|---|
| 1 | Dry Eye Syndrome-68 (13%) | Dry Eye Syndrome-19 (11%) |
| 2 | Chalazion-49 (9%) | Posterior Vitreous Detachment-14 (8%) |
| 3 | Conjunctivitis: bacterial/viral-36 (7%) | Anterior Uveitis-13 (8%) |
| 4 | Posterior Vitreous Detachment - 34 (7%) | No abnormality detected-13 (8%) |
| 5 | Corneal abrasion-29 (6%) | Corneal Abrasion-11 (6%) |
| 6 | Anterior Uveitis-29 (6%) | Chalazion-10 (6%) |
| 7 | Subconjunctival Haemorrhage-24 (5%) | Corneal foreign body-7 (4%) |
| 8 | No Abnormality Detected-21 (4%) | Conjunctivitis: Bacterial/viral-6 (3%) |
| 9 | Corneal foreign body-16 (3%) | Keratitis: Bacterial-6 (3%) |
| 10 | Keratitis: Bacterial-14 (3%) | Keratitis: Herpes simplex-6 (3%) |
Table 1: The 10 most common diagnosis’s during the second week of lockdown in 2020 and the corresponding week in 2019.
| Diagnosis | 2019 n (%) | 2020 n (%) |
|---|---|---|
| Anterior Uveitis | 29 (6%) | 12 (7%) |
| Keratitis: Bacterial | 14 (3%) | 6 (3%) |
| Papilloedema | 4 (1%) | 3 (2%) |
| Retinal tear | 6 (1%) | 2 (1%) |
| Retinal detachment | 7 (1%) | 2 (1%) |
| Chemical eye injury | 8 (2%) | 1 (1%) |
| Acute angle closure glaucoma | 1 (<1%) | 1 (1%) |
| Giant Cell Arteritis | 2 (<1%) | 0 |
| Scleritis | 5 (1%) | 1 (1%) |
| Periorbital cellulitis | 4 (1%) | 5 (3%) |
| Central retinal artery occlusion | 1 (<1%) | 0 |
Table 2: Examples of attendances of Eye Emergencies presenting during the second week of lockdown in 2020 and a corresponding week in 2019.
This study provides the first results as to how the COVID-19 lockdown has affected an Ophthalmology Emergency Department. We have shown that there has been a dramatic reduction in patient attendances over 9 weeks of lockdown, with numbers dropping by half compared to a similar period in 2018 and 2019. This is in keeping with the drop in attendance figures seen at the general A&E Departments. In April 2020, 916,581 attended A&E in the UK, a reduction of 57% from the same period in April 2019 [6]. In the UK, Ophthalmology Emergencies usually present to a general A&E and then are referred onto an ophthalmologist. This makes it challenging to analyse Ophthalmology Emergency attendances from the gross A&E figures. In Manchester we have a well-established walk in Emergency Eye Department giving us a unique insight into how Ophthalmology presentations have varied through the COVID-19 pandemic.
Formal lockdown came into effect on the 23rd March 2020 however our results show that the attendances started to drop 6 days earlier on the 17th March. Throughout lockdown travel to hospital was never limited for health reasons. Despite this we have seen a significant drop in attendances. Changes to the working of our EED could help explain part of this downturn. During lockdown we introduced a consultant ophthalmologist to be present in the EED during its opening times as per national guidelines [4]. They would help to manage the flow of patients in the department, supervise juniors directly and take telephone referrals from other healthcare providers. Alongside this a Nurse Practitioner was allocated to answer patient queries and give self-care advice over the phone. This level of senior clinician involvement and a dedicated patient phoneline would help to explain a reduction in attendances through improved triage and self-care advice. However, this change is unlikely to cause a 50% drop in attendances. One of the clear messages from the government was to ‘stay at home’ & ‘protect the NHS’ [3]. It is likely people were, and still are, staying away from hospitals. They are following government guidelines of safeguarding the NHS and to protect themselves from the threat of contracting COVID-19.
From our analysis there is no statistical difference in the patient’s ethnicity or social deprivation score for those attending during lockdown versus the same period in 2019. There is a trend to the under 20’s and over 70’s staying away more during lockdown, but this was not statistically significant. It is reassuring that the government’s message to ‘stay at home’ seems to have reached all areas of the population equally. In addition, the social changes during lockdown do not appear to have affected access to Emergency Eye Services for those more deprived.
The attendances to the EED are significantly reduced during lockdown however the case mix remains unchanged. There is no significant difference between the proportion of Eye Emergencies, Community Eye Emergencies and Non-Eye Emergencies presenting during a week of lockdown compared to the same week in 2019. We expected the urgent conditions causing sight loss or pain to still present during lockdown and the less urgent cases to stay away. However, this has not been the case. Most notably eye emergencies have dropped by 61% which is a concerning finding. The top 10 diagnoses between the years are remarkably similar with the most common diagnosis (dry eyes) in both years, accounting for over 10% of all cases seen. This condition can be managed in the community or by self-care and is not an eye emergency. More severe painful conditions such as anterior uveitis had 29 cases in 2019 versus 12 cases in 2020. There are anecdotal reports on the flare up of uveitis being related to higher levels of stress, as many people are working at home this could have reduced stress levels and subsequently the frequency of uveitis presentations. However, you could also argue that COVID-19 could lead to higher stress levels due to worry about your health and the potential effect of lockdown on your employment. This reduction is mirrored in bacterial keratitis, 14 cases in 2019 versus 6 cases in 2020, this could be due to the less frequent use of Contact lenses during lockdown in comparison to normal times [7,8].
There was a reduction in posterior vitreous detachments from 34 cases in 2019 to 14 cases in 2020. A similar reduction in retinal detachments with 7 cases in 2019 and 2 cases in 2020 and retinal tears with 6 cases in 2019 and 2 cases in 2020. During lockdown, the general population will have had a significant reduction in their mobility and should be leading a more sedate lifestyle by staying at home. This might have a protective effect on developing a posterior vitreous detachment and its potential sequalae. If this is not the case, we should see a rise in chronic retinal detachments in the future as the pressure of COVID-19 lifts.
Cases of ocular trauma were less frequent in during lockdown with 23 cases in 2020 and 72 in 2019, a 69% drop. A significant proportion of this case was corneal foreign bodies with 7 cases in 2020 and 16 cases in 2019. This reduction in ocular trauma is contrary to other units in the UK and abroad who have seen a rise in the cases of ocular trauma during lockdown, often due to increased levels of DIY [9-13].
During the lockdown period all diagnoses are down in proportion to each other rather than just a reduction in the more minor conditions. There are possible explanations for the reduction of some eye emergencies, but It is unlikely that all ophthalmic emergencies have all had a global reduced incidence due to lockdown. Possible explanations are that patients are avoiding hospitals to try and reduce the burden on the NHS or they are concerned about contracting COVID-19 in hospital so are staying at home. This trend has been seen across other specialities. Most notably the 60 % reduction in urgent cancer referral from GP’s [11] and the 30%-50% drop in heart attacks presenting to hospital.
The general significant reduction in attendances to the Emergency Eye Department and a reduction in the presentation of severe eye emergencies is a concern and further analysis and time is needed to obtain a full picture of the further consequences of the pandemic and lockdown. Once the pressure from COVID-19 abates will these hidden ophthalmology cases start to appear? As a community we should also be concerned about the sequelae that may be unleashed. The authors are concerned about the number of patients potentially developing complications as a consequence of ‘staying at home’, which could invariably lead to sight loss. It is important to stress to the general population to still seek help if they feel they have an ophthalmology emergency.
Katie Harronz- Research at UCL Great Ormond Street institute of Child Health is supported by the NIHR Great Ormond Street Hospital Biomedical Research Centre
Citation: Young JF, Harron KL, Bilal L, Richardson JAL, Dhawahir-Scala FE (2020) The Effect of Lockdown due to COVID-19 on a Large Emergency Eye Department: The Manchester Experience. J Clin Exp Ophthalmol. 11:859. DOI: 10.35248/2155-9570.20.11.859
Received: 28-Sep-2020 Accepted: 12-Oct-2020 Published: 19-Oct-2020 , DOI: 10.35248/2155-9570.20.11.859
Copyright: © 2020 Young JF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.