Clinical & Experimental Cardiology
Open Access
ISSN: 2155-9880
ISSN: 2155-9880
Research - (2023)Volume 14, Issue 4
Background: The results of stenting the Unprotected Left Main Coronary Artery (UPLM) without IVUS needs to be studied.
Methods: This prospective and retrospective study was performed in the university hospitals. The local ethics committee approved the study. In the last five years, one hundred twenty patients with left main disease > 50% were subjected to stenting with drug-eluted stents. Risk assessment was calculated including Euro SCORE and Syntax score.
Patient selection: Consecutive patients arriving for primary Stenting or acute coronary episode were included.
Medications: All patients received clopidogrel and aspirin before the planned procedure. Anticoagulation with unfractionated heparin in a dose of 10000 IU was given at the beginning of the PCI. Calcification was assessed by angiographic imaging only. We estimated the vessel diameter as 2/3 diameter of the branches. One or two stent strategy was utilized according to the situation of the lesions.
Results: 92 patients (77.3%) presented with ACS, of which 65 patients (54.6%) had no Previous Intervention, and 27 patients (22.7%) had a previous PCI. Left ventricular ejection fraction significantly correlates with the complication at six months follow-up.
Syntax score: 11 patients (55%) with a high score of more than 32 had adverse events, P=0.004. Residual syntax shows a less significant correlation (P=0.016). Final kissing balloon inflation shows no statistically significant difference.
Conclusions: PCI in UPLM is a safe, feasible option with a high technical success rate and acceptable outcome at follow-up, even without the utilization of IVUS.
Left main coronary artery stenosis, Drug-eluted stents, SYNTAX score, IVUS, PCI
ACS: Acute Coronary Syndrome; BMS: Bare Metal Stent; CIN: Contrast-Induced Nephropathy; CABG: Coronary Artery Bypass Graft; CAD: Coronary Artery Disease; CCS: Chronic Coronary Syndrome; CTO: Chronic Total Occlusion; DES: Drug-Eluting Stent; ISR: In-stent restenosis; IVUS: Intravascular Ultrasound; LMCAD: Left Main Coronary Artery Disease; LMB: Left Main Bifurcation; LAD: Left Anterior Descending; LCX: Left Circumflex; MACE: Major Adverse Cardiac Event; PCI: Percutaneous Coronary Intervention; LVEF: Left Ventricular Ejection Fraction; STEMI: ST-Elevation Myocardial Infarction; NSTEMI: Non-ST Elevation Myocardial Infarction; TLR: Target Lesion Revascularization; TVR: Target vessel revascularization
All authors consent for publication
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study. Data and master charts are available with Dr. MS.
• Funding: This research received no specific grant from any public, commercial, or not-for-profit funding agency.
• Conflict of interest: The authors declare no conflict of interest in preparing this article.
Written consent from the local ethics committee: The Ethical Committee of the Faculty of Medicine Alexandria University, number 00012098
Written consent from patient: Written/verbal permission from the patient or the patient's parent/carer.
All the nursing staff, technicians, and residents
AZ, involved in the study concept, design, and stenting.
ML engaged in the study's conception, design, and stenting.
MS, involved in the study concept, design, and stenting.
SR was involved in writing the paper and submitting it. All authors contributed to the writing—original draft preparation and approved the final version.
None
The authors declare no conflict of interest in preparing this article
None.
The datasets used or analyzed during the current study are available from the corresponding author upon request.
Clinical trials demonstrated a higher re-intervention rate after Percutaneous Coronary Intervention (PCI) compared with Coronary Artery Bypass Grafting (CABG). PCI had a lower incidence of cerebrovascular events [1-9]. Current guidelines recommend CABG as class I for most patients with Left Main (LM) [3,4]. New features in stent technology, revascularization techniques, and antithrombotic medications make PCI safer. PCI with Drug-Eluting Stent (DES) implantation for Left Main Coronary Artery (LMCA) disease has dramatically increased in daily clinical practice. Detailed examination of the anatomic size of LM lesions is achieved using Intravascular Ultrasound (IVUS) [10-15]. IVUS helps determine the vessel size, lumen area, plaque extent, and calcification within the LMCA. IVUS is of value to ensure stent optimization of LMCA PCI. IVUS guidance is associated with improved clinical outcomes after the procedure.
Aim of the work
The study was designed to evaluate the short and mid-term clinical outcomes of elective, unprotected left main coronary artery stenting in multiple local centers. The feasibility of stenting UPLMD without IVUS needs to be studied to determine if this is possible in centers not equipped with IVUS.
Ethics approval and consent to participate
The local ethics committee: The Ethical Committee of the Faculty of Medicine Alexandria University, number 00012098, approved the study. We obtained informed consent: written/verbal permission from the patient or the patient's parent/career. All methods followed relevant guidelines and regulations (Declaration of Helsinki).
IVUS is the standard method now for optimization of stenting of the left main coronary artery. When it is not available, and in urgent cases, we cannot ignore the possibility of trying stenting without IVUS. So this study throws light on this possibility. The size of the main artery was calculated as 2/3 of the sum of the branches two or three. Finally, balloon reinflation was resorted to ensure sufficient strut deployment. Follow of six months and one year is not sufficient, but this does not validate the results. DK crush was not used in the beginning. Mini crush was used at first.
1. PCI in unprotected left coronary artery disease is a possible option with a high technical success rate and acceptable outcome at follow-up when IVUS is unavailable.
2. The following parameters were associated with increased MACE rate in our study: Hypertension as a risk factor was associated with an increased risk of complication at follow-up; elevated SYNTAX score; distal left main lesion location vs. ostial and mid-shaft; reduced left ventricular ejection fraction; residual SYNTAX score as a marker of incomplete revascularization
3. Risk stratification is crucial for strategy selection in managing LMCAD patients based on current validated anatomic and physiologic complexity scores.
4. Absence of assisting imaging techniques, namely IVUS, is not prohibitive to practicing UPLM PCI, as demonstrated in our study, despite its valuable role in stent optimization.
The present study evaluated the feasibility of stenting LMCA without IVUS. We successfully treated one hundred twenty such patients with drug-eluting stents. The percentage of complications was not inferior to the incidence when IVUS was utilized. Thus the strategy of stenting LMCAD without these techniques is safe and effective when performed by experienced interventional cardiologists [27-31]. We followed all patients in a cardiology outpatient clinic one month after PCI, followed by a visit or phone call after six months, and then after one year. No routine angiography was performed unless symptomatic or positive stress test; 24 patients had exercise testing during the follow-up period, four were positive, and fifteen had follow-up angiography following a positive stress test or ACS. In our study, the mean age of the patients was 60 years; this is six years younger than the mean age in the EXCEL trial, in which the mean age was 66.5 years; this may reflect the earlier or aggressive atherosclerotic cardiovascular burden. Lee HM et al., in their study, concluded that Simple crossover LM-to-LAD stenting without opening of a strut on the LCX ostium was associated with acceptable long-term clinical outcomes [24]. As regards other demographic criteria in our study predominant male sex (73.3%) was shared in different left main trials; in the Indian registry published in the Indian heart journal by Ray et al., 2016 [25], around 76% of the patients were male, of note the mean age was 60 years in this registry. In our study, neither the age nor the sex had influenced the outcome, including MACE at one-year follow-up significantly; still, at one-month follow-up, the reported complications were higher (9 patients out of 12) more than 65 years, and only three were below than 50 years [32-36].
A recent systematic review published in Cardiovascular Revascularization Medicine Journal in 2020 shows that women undergoing PCI for unprotected LMCD are at higher risk of MACE and MI than men. However, our study did not validate this finding primarily due to the small sample size [36]. As regards the risk factors and their relation to complications in our study, only hypertension had a statistically significant association with the adverse outcome, unlike DM, dyslipidemia, and smoking. These findings correlate with results published before [25]. The SYNTAX I score is one of our study's most important predictors of MACE. The mean syntax score in the complication group was 32.3 vs. 27.6 in the group with no complications (P-value 0.006). The same finding was reproducible at one month and six months outcome these findings consider revalidation of the value of SYNTAX score I as one of the most important prognostic factors in UPLM PCI. Capodanno et al. found that the SYNTAX score is essential to suggest cardiac mortality and MACE in patients undergoing percutaneous revascularization of the left main coronary artery even at short and mid-term follow-up at one year [27]. As regards the SYNTAX II score, it showed statistically significant results concerning MACE in our study. Syntax II Score was significantly higher in complication group 36.24 vs. 27.26 in the group without complications (P value<0.001). This finding comes in agreement with a study published by Madeira et al. from Portugal in 2016 titled Potential Utility of the SYNTAX Score II in Patients Undergoing Left Main Angioplasty over 132 patients undergoing UPLM PCI and concluded that The SYNTAX Score II might allow better and individualized risk stratification of patients who need revascularization of an unprotected left main coronary artery The authors suggested that a difference more significant than 5.7% between SYNTAX Score 2 estimates for PCI versus CABG may be clinically relevant in selecting the optimal revascularization strategy [28]. Another important prognostic factor in our study is the Residual Syntax Score (RSS) which was significantly higher in the complication group at one month, with a mean of 10.75 in complication vs. However, 4.77 in another group (P-value=0.018) was less significant at one-year follow-up; the value of RSS in many trials did not address UPLM PCI specifically. Another important angiographic criterion that shows significance is the location of the left main lesion. Ostial LM lesion PCI in our study, when compared to the distal site, offers a significantly lower incidence of MACE that was evident at one-year follow-up, where 10% of the distal LM PCI showed complication versus no reported difficulties in the ostial LM PCI group (P value=0.001). This finding agrees with Hyun et al.'s essential registry in 2020 [30]. Regarding the procedural characteristics, there was no significant difference in MACE in our study between the 2-stent strategy, including different techniques of 2-stent methods and one stent during the follow-up period. This is shown in The Milan and New-Tokyo Registry published by Takagi et al. in 2016, and they compared one versus two stents strategy in UPLMD in more than nine hundred and thirty patients in three different centers. The main issue observed was more TLR in single stent strategy, but no significant mortality difference; needless to say, ostial compromise of side branch ostium (whether LAD or LCX) is among the critical reasons for increased side branch revascularization, but as they concluded, it did not affect mortality [31-36].
This prospective study included 50 patients undergoing elective percutaneous coronary intervention for unprotected left coronary artery disease in Alexandria. In addition, a retrospective arm included 70 patients who had left main stenting in the last five years. The study included 120 patients, 88 males and 32 females, with a mean age of 61. Regarding risk factors, we found that diabetes was the most common risk factor present in 95 patients (79.2%), followed by hypertension in 83 patients (69.2%), 69 patients were current smokers (57.5%), and dyslipidemia in 60 patients (50%). Regarding clinical presentation, we found that 92 patients (77.3%) presented with ACS, of which 65 patients (54.6%) had no previous intervention, and 27 patients (22.7%) had a prior PCI. One patient with previous CABG, patients with a chronic coronary syndrome, were 27 (22.7%), and none of the chronic coronary syndrome patients had an earlier intervention. As shown in Table 1.
| No. | % | |
|---|---|---|
| Presentation | ||
| Acute | 92 | 77.3 |
| DiNovo ACS | 65 | 54.6 |
| ACS (Previous intervention) | 27 | 22.7 |
| CCS (No previous intervention) | 27 | 22.7 |
| ECG | ||
| Normal resting | 40 | 33.3 |
| Diffuse ST depression/raising aVR | 36 | 30 |
| ST elevation | 6 | 5 |
| Left BBB | 8 | 6.6 |
| Atrial fibrillation | 1 | 0.8 |
| Stigmata of previous infarction | ||
| Anterior Q waves | 20 | 16 |
| Inferior Q waves | 9 | 7.5 |
| ECHO | ||
| Severe MR | 5 | 4.1 |
| RWMA | 50 | 41.6 |
| ECHO (LVEF) (%) | ||
| Min.-Max. | 25.0-75.0 | |
| Mean ± SD. | 49 ± 12 | |
| EURO score (%) | ||
| 0-3 | 100 | 84 |
| 3-5 | 12 | 10.1 |
| >5 | 7 | 5.9 |
Table 1: Clinical, ECG, and ECHO characteristics of the studied cases (n=120).
Anatomical characteristics
According to coronary angiography, we determined the following anatomical characteristics:
• CAD extent, whether non-distal LM disease (ostial and shaft) or a distal bifurcation or trifurcation
• Left circumflex dominance.
• Bifurcation angle between LAD, LCX
• Ostial LCX significant disease as shown in Table 2.
| No. | % | |
|---|---|---|
| CAD extent | ||
| Non-distal | 19 | 15.8 |
| Distal | 101 | 84.2 |
| Bifurcation | 94 | 78.3 |
| Trifurcation | 7 | 5.8 |
| LCX dominance | ||
| No | 90 | 75 |
| Yes | 30 | 25 |
| Ostial LCX significant disease | ||
| No | 70 | 58.3 |
| Yes non-dominant LCX | 35 | 29.1 |
| Yes dominant LCX | 15 | 12.5 |
| Bifurcation angle | ||
| <70 | 92 | 76.7 |
| >70 | 28 | 23.3 |
| Number of diseased vessels | ||
| 1 | 19 | 15.8 |
| 2 | 65 | 54.1 |
| 3 | 36 | 30 |
| Presence of calcification | 55 | 45.8 |
| Presence of thrombi | 39 | 32.5 |
| RCA lesion | 29 | 24.1 |
| Medina classification (Distal LM) | ||
| 1,0,0 | 11 | 10.8 |
| 0,1,0 | 0 | 0 |
| 1,1,0 | 33 | 32.6 |
| 0,0,1 | 0 | 0 |
| 1,0,1 | 12 | 11.88 |
| 0,1,1 | 0 | 0 |
| 1,1,1 | 45 | 44.5 |
| Syntax I | ||
| <23 | 17 | 14.3 |
| 23-32 | 73 | 61.3 |
| >32 | 29 | 24.4 |
| Mean ± SD. | 28.37 ± 6.53 | |
Table 2: Angiographic characteristics (n=120).
| PCI characteristics | No. | % |
|---|---|---|
| LM stent type: Xience Xpedition/Alpine/V/Prime |
76 | 63.33 |
| Promus Element /Element plus/premiere | 12 | 10 |
| Biomatrix | 10 | 8.3 |
| Taxus Liberte | 8 | 6.66 |
| Onyx | 6 | 5 |
| Other stents (Osirio-Eucalimus-Isaar-Ultimaster) | 8 | |
| Technique (n=120) | ||
| Predilatation | 85 | 70.8 |
| One stent | 87 | 72.5 |
| Provisional | 71 | 59.2 |
| Direct (non-distal lesions) | 16 | 13.3 |
| Two stents | 33 | 27.9 |
| Culotte | 14 | 11.9 |
| SKS | 3 | 2.5 |
| TAP | 13 | 11 |
| Mini crush (DK crush) | 3 | 2.5 |
| Post-stenting balloon dilatation | ||
| POT | 53 | 44.1 |
| Re POT | 22 | 18.3 |
| Final kissing | ||
| No | 65 | 54.2 |
| Yes | 55 | 45.8 |
| IVUS guidance | 0 | 0 |
| Length Min. – Max. (Mean ± SD). | 8.0-48.0 (27.8 ± 10.4) | |
| Diameter Min. – Max. (Mean ± SD.) | 3.5-5 (4 ± 0.5) | |
| Median (IQR) | 3.5 (3.50-4.0) | |
| Other vessels treated | ||
| 1 vessel | 59 | 49.2 |
| 2 vessels | 35 | 29.1 |
| 3 vessels | 7 | 5.8 |
| Residual syntax Min.-Max. (Mean ± SD.) | 0.0-24 (5.3 ± 6.3) | |
| Median (IQR) | 4.0 (0.0-8.0) | |
Table 3: Procedural characteristics of the studied population (n=120).
PCI characteristics
• We classified the patients according to the following PCI Characteristics:
• Access either femoral (101 patients) or radial (19 patients).
• We used Guiding catheters to cannulate LMCA. 6F in 53 patients, 7F in 67.
• LM stent number.
• The technique used for stenting (Provisions-Cullotte-SKS-TAP- Minicrush, DK crush)
• POT and Final kissing done or not?
• Diameter and length of the LM stent.
• Other stents (s) are used to treat other lesions.
• Total stents number
• We calculated the residual syntax score (Table 3).
Complications: Procedural, In-hospital, one-month, and six months complications were documented, including access site hematoma, contrast nephropathy, dissection, heart failure, bleeding, TLR, non-TLR, Angina, ACS, stroke, and Death as shown in Tables 4-8.
| Complications | ||||||
|---|---|---|---|---|---|---|
| Procedural & In hospital | One month | Six months | ||||
| No. | % | No. | % | No. | % | |
| No | 100 | 83.3 | 108 | 90 | 104 | 86.7 |
| Yes | 20 | 16.7 | 12 | 10 | 16 | 13.3 |
Table 4: Distribution of the studied cases according to complications (n=120).
| Complication | No. | % |
|---|---|---|
| Procedural | ||
| Access site hematoma | 8 | 6.6 |
| PCI complications (dissection) | 2 | 1.66 |
| In hospital | ||
| CIN (Contrast Induced Nephropath) | 3 | 2.5 |
| Heart failure | 7 | 5.8 |
| One month | ||
| Heart failure | 3 | 2.5 |
| Bleeding | 4 | 0.83 |
| Angina | 3 | 2.5 |
| Non- TLR | 1 | 0.83 |
| Stroke | 1 | 0.83 |
| Six months- One year follow up | ||
| TLR | 2 | 1.66 |
| Non- TLR | 4 | 3.33 |
| Follow-up exercise test | 24 (20) | 20 (16.6) |
| Follow up angiography | 15 | 12.5 |
| ACS/CCS | 6 | 5 |
| Death | 2 | 1.66 |
| LVEF improvement | 12 | 10 |
Table 5: Distribution of the studied cases according to complications (n=120).
| No. | % | |
|---|---|---|
| Death | 2 | 1.7 |
| Nonfatal ACS | 6 | 5 |
| TLR | 2 | 1.7 |
| Combined (Death/ACS/TLR) | 10 | 8.3 |
| Non-TLR | 5 | 4.2 |
| Stroke | 1 | 0.8 |
| Heart failure | 7 | 5.8 |
| CABG referral | 0 | 0 |
Table 6: Distribution of the studied cases according to total MACE during follow-up (n=120).
| Complications (in hospital) | P | ||
|---|---|---|---|
|
No (n=100) | Yes (n=20) | |
| Positive DM (%) | 78 (78%) | 85.0 (0.7%) | 0.763 |
| Positive hypertension | 66 (66%) | 85.0 (0.09%) | 0.093 |
| Presentation | (n=99) | (n=20) | |
| Acute | 77 (77.8%) | 75 | 0.775 |
| CCS | 22 (22.2%) | 25 | |
| ECHO (LVEF) (%) | |||
| <40 | 17 | 60 | 0.033* |
| ≥ 40 | 83 | 40 | |
| Positive LCX dominance | 29 | 5 | 0.024* |
| Ostial LCX significant disease | 40 | 50 | 0.408 |
| Bifurcation angle | |||
| <70 | 77 | 75 | 0.781 |
| >70 | 23 | 25 | |
| Kissing | 47 | 40 | 0.566 |
| Access-Femoral | 83 | 90 | 0.737 |
| Access-Radial | 17 | 10 | |
| Other stents | 60 | 70 | 0.401 |
| Syntax I | 27.63 ± 6.54 | 32.03 ± 5.26 | 0.006* |
| Syntax II (PCI) Number (%) | 27.2 ± 7.5 (6.5 ± 4.9) | 36.2 ± 8.6 (13.8 ± 11.5) | <0.001* |
| Syntax II (CABG) Number (%) | 27.7 ± 10.4 (7.3 ± 6.7) | 36.2 ± 10.7 (16.2 ± 13) | 0.003* |
| Residual syntax | 4.98 ± 6.58 | 7.30 ± 4.73 | 0.016* |
Table 7: Relation between complications (in hospital) and different parameters.
| Complications (six months) | P | ||
|---|---|---|---|
| No (n=104) (%) | Yes (n=16) % | ||
| Positive DM | 83 (79.8%) | 75 | 0.741 |
| Positive HYPERTENSION | 75 (72.1%) | 50 | 0.087 |
| Presentation | (n=103) | (n=16) | |
| Acute | 80 (77.7%) | 75 | 0.757 |
| CCS | 23 (22.3%) | 25 | |
| ECHO (LVEF) (%) | |||
| <40 | 25 (24%) | 100 | 0.023* |
| ≥40 | 79 (76%) | 0 | |
| Positive LCX dominance | 24 (23.1%) | 37.5 | 0.226 |
| Ostial LCX significant disease | 42 (40.4%) | 50 | 0.468 |
| Bifurcation angle | |||
| <70 | 82 (78.8%) | 62.5 | 0.201 |
| >70 | 22 (21.2%) | 37.5 | |
| Kissing | 47 (45.2%) | 50 | 0.719 |
| Access | |||
| Femoral | 85 (81.7%) | 100 | 0.072 |
| Radial | 19 (18.3%) | 0 | |
| Other stents | 64 (61.5%) | 62.5 | 0.941 |
| Syntax I | 28.82 ± 5.93 | 25.44 ± 9.29 | 0.149 |
| Syntax II (PCI) | |||
| Number | 29.4 ± 8.3 | 24.5 ± 7.8 | 0.029* |
| % | 8.1 ± 7.3 | 5.4 ± 3.4 | 0.066 |
| Syntax II (CABG) | |||
| Number | 30.2 ± 10.7 | 22.6 ± 10.2 | 0.023* |
| % | 9.4 ± 9.1 | 5.0 ± 3.2 | 0.095 |
| Residual syntax | 5.3 ± 6.6 | 5.8 ± 3.9 | 0.241 |
Table 8: Relation between Complications (six months) and different parameters.
Statistical relation with different complications
Demographic data: The study included 120 patients. There was no statistically significant difference between the procedural and in-hospital complications regarding sex (p-value=0.46) and age group (p-value=0.52). Still, at one-month follow-up, 9 out of 12 complications were more than 60 years, and only three were below 50 years (P-value=0.024); at six months, there were no significant correlations between age, sex, and adverse events.
Risk Factors: As regards the risk factors, only the hypertension group showed statistically significant increased complications, where 17 out of 20 complications were in hypertensive subjects (85% with P-value=0.093); this finding was consistent at one-month follow- up where all 12 patients with complications were hypertensive (100%) (P-value=0.017) and to less extent at six months follow up eight patients out of 16 cases with complications were hypertensive (P-value=0.087). Diabetes and presentation (acute vs. CCS) were not significantly correlated with complication rate, P-value=0.76 for DM and 0.77, the same finding at one month and six months of follow-up.
LV function: Left ventricular ejection fraction significantly correlated with procedural and in-hospital complications, with 12 patients out of 20 who had reduced LVEF by Less than 40 % (P-value=0.033); at one month, LVEF was not significantly associated with complications, yet at six months follow up all 16 patients with reported complications (100%) had baseline LVEF of less than 40 % (P-value=0.023)
Angiographic and procedural characteristics
Syntax score: Statistically significant correlation between Syntax score and adverse outcome with a higher score, one patient out of 20 (5%) had a lower score than 23. In contrast, eight patients with intermediate scores had adverse events, and 11 patients (55%) with a high score of more than 32 had adverse events with a P-value of 0.004; the mean syntax score in the complication group was 32.3 vs. 27.6 in the group with no complications (P-value 0.006), Syntax II Score was significantly higher in the complication group 36.24 vs. 27.26 in the group without complications (P value<0.001), Residual syntax shows a less significant correlation with a mean value of 7.3 in the complication group versus 4.9 in the other group (P value=0.016) (Table 7), Figure 1 relation between complications and Syntax I. One month, the Syntax score still correlates with adverse events; the Mean syntax I score was 31.76 in the complication group vs. Twenty-eight in the other Group (P-value 0.07), and Syntax II PCI a mean of 38.47 in the complication Group vs. 27.69 in another group, the residual syntax score shows again statistically significant differences at one month with a mean of 10.75 in complication vs. 4.77 in another group (P-value=0.018) but not at six months follow-up between the complication group and the other group
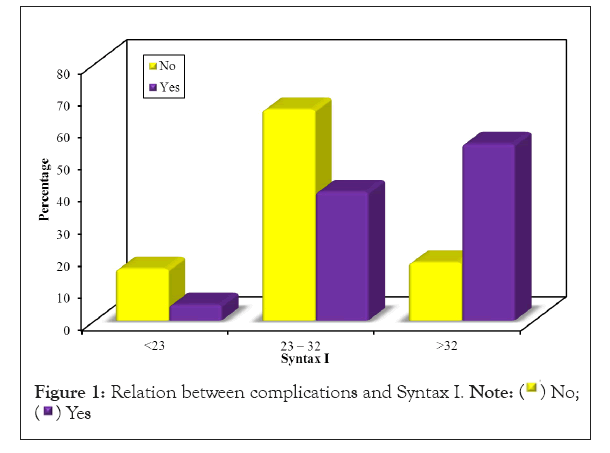
Figure 1: Relation between complications and Syntax I.

LCX: Neither LCX dominance nor significant ostial disease showed a statistically significant correlation with the adverse events during in-hospital and follow-up periods, as well as the angle between LAD and LCX in this study
Kissing balloon inflation: Final kissing balloon inflation shows no statistically significant difference compared to non-kissing regarding complications, procedural in-hospital, and follow-up period.
Other stents: Implantation of more than one stent shows no statistically significant differences compared to the single stent regarding complications, procedural in-hospital, and follow-up period.
Follow-up was done by the patient’s reexamination with history, ECG, and Echo. No new coronary angiography was done except in six patients with new chest pains. The left main stent was found to be patent or not stenosed. Multislice CT was done instead of coronary angio in five patients; the left main stents were not restenosed.
Procedural outcomes
1. Thrombolysis In Myocardial Infarction (TIMI) flow grade was graded Grade 0, absence of antegrade flow beyond the point of occlusion; Grade 1, partial penetration of contrast agent beyond the obstruction but incomplete distal filling; Grade 2, patency with opacification of the entire distal vessel but with delayed filling or washout of contrast agent; and Grade 3, normal flow.
2. We defined the procedural success rate as residual stenosis of less than 20% and establishment of Thrombolysis in Myocardial Infarction (TIMI)-3 flows. Without major periprocedural adverse events (Death, myocardial infarction, emergency revascularization).
In-hospital outcomes
A: Death; B: Myocardial infarction; C: Cerebrovascular stroke; D: Re-intervention: Target Vessel Revascularization (TVR), Target Lesion Revascularization (TLR), and Non-Target Vessel Revascularization (Non- TVR); E: Heart Failure.
Thirty days outcomes
A: Death; B: New angina or myocardial infarction; C: Cerebrovascular stroke; D: Re-intervention: TVR, TLR and (Non- TVR); E: Heart Failure. We recorded six-month outcomes as death, cerebrovascular stroke, re-intervention (TVR), (TLR), and (Non- TVR), new angina, and Heart Failure.
Study endpoints: Primary endpoints are major cardiovascular events at 30 days and six months, defined as death, myocardial infarction, cerebrovascular stroke, and re-intervention: TVR, TLR, and Non-TVR. All methods were performed following the relevant guidelines and regulations
Statistical analysis of the data
Data were fed to the computer and analyzed using IBM SPSS version 20.0. (Armonk, NY: IBM Corp) Qualitative data were described using numbers and percentages. The Kolmogorov-Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, and median. The significance of the obtained results was judged at the 5% level. The used tests were:
• Chi-square test: For categorical variables to compare different groups.
• Fisher's Exact or Monte Carlo correction: Correction for chi-square when more than 20% of the cells have an expected count of less than 5.
• Student t-test: For normally distributed quantitative variables, to compare two studied groups.
This study was performed in multiple local centers prospectively and retrospectively. The local ethics committee approved the study, and the patients signed informed consent. In the last five years, one hundred twenty patients with left main disease >50% were subjected to stenting with drug-eluted stents. All patients were subjected to detailed history taking with particular emphasis on acute coronary syndrome, angina duration, class, previous coronary interventions, and medications. In addition, 12 lead ECGs were revised with an evaluation of ST/T changes and any old infarction. An echocardiographic examination was done on all patients following the recommendations of the American Society of Cardiology [16-20]. We recorded ejection fraction, LV diameters, and wall motion. Laboratory testing included kidney function, lipid profile, and blood sugar. Risk assessment was calculated for every patient, including Euro SCORE and Syntax score.
Patient selection
Consecutive patients arriving for primary stenting or acute coronary episode were included.
Exclusion criteria: Patients with pulmonary edema, advanced renal insufficiency, advanced COPD (Chronic Obstructive Pulmonary Disease), and patients referred for surgery.
Medications: All patients received clopidogrel and aspirin before the planned procedure. Anticoagulation with unfractionated heparin in a dose of 10000 IU was given at the beginning of the PCI [21]. Post PCI, all patients received β blockers, ACE inhibitors, statins, and dual antiplatelets in the guidelines recommended doses.
PCI technique: A steerable guidewire was advanced in LAD, followed by PCI with pre-dilatation or direct stenting according to the operator's discretion (according to prediction of possible calcification, then predilation was opted to). One or two stent strategy was utilized according to the situation of the lesions [22-26]. Although we know that IVUS is the standard method to determine calcification, calcification: was assessed by angiographic imaging. We assessed vessel diameter as 2/3 diameter of the branches.
Citation: Rafla S, Zaki A, Loutfi MI, Sadaka MA, Shebl M (2023) The Feasibility of Stenting the Unprotected Left Main Coronary Artery without IVUS. J Clin Exp Cardiolog.14:786.
Received: 09-May-2023, Manuscript No. JCEC-23-24000; Editor assigned: 11-May-2023, Pre QC No. JCEC-23-24000; Reviewed: 25-May-2023, QC No. JCEC-23-24000; Revised: 01-Jun-2023, Manuscript No. JCEC-23-24000; Published: 09-May-2023 , DOI: 10.35248/2155-9880.23.14.786
Copyright: ©2023 Rafla S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.