Journal of Nutrition & Food Sciences
Open Access
ISSN: 2155-9600
ISSN: 2155-9600
Research Article - (2013) Volume 3, Issue 3
Background: The Glycemic Index (GI) of traditional bread has not been measured previously. Objective: To determine the GIs of 3 traditional breads and 3 commercial breads widely consumed in the United Arab Emirates (UAE). Design: The study was conducted at the Rashid Center for Diabetes and Research in the UAE. Subjects (n=14) were served 50 g glucose (reference) on 3 occasions, followed by a selection of 50 g of available carbohydrates in the breads. Each bread was tested by 7 subjects, and these breads were 3 traditional breads (rigag, chbab, and khameer) and 3 commercial breads widely consumed in the UAE (white pita bread, khobuz; white bread roll, summon; whole-meal bread). After an 8- to 10-hour overnight fast, the subjects’ capillary blood glucose was measured via finger-prick samples over 120 min. The GI (%) of a specific bread for each subject was measured geometrically (trapezoids rule) by calculating the incremental area under the blood glucose response curve (IAUC) divided by the average IAUC for the reference (in triplicate) multiplied by 100. Then, the GI of the bread was calculated as the mean value across all subjects who consumed that bread. Results: Compared to the control (50 g glucose), the GIs of the traditional UAE bread ranged between low and medium; the GIs for rigag, chbab, and khameer were 48.21(15.6), 63.95 (7.06), and 63.91 (11.49), respectively. AllGIs exhibited a significant difference (P<0.05). However, the GIs of the 3 commercial breads ranged between medium and high. The GIs of khobuz, summon, and whole-meal bread were 70.11 (15.42) (P<0.05), 73.12 (4.63) (P>0.05), and 66.71 (14.68) (P<0.05), respectively. The correlation between the GI value in the studied portion and fat (r=0.04) and protein (r=0.18) was weak, but that with insoluble fiber was moderate (r=0.48). Conclusion: The GI values of these traditional UAE breads provide valuable information to healthcare providers, researchers, and the public. The difference between our GI values and that of previously tested food proves the importance of testing the food consumed in a particular country.
Keywords: Glycemic index; Carbohydrate; UAE traditional diet
The glycemic index, a tool for carbohydrate classification
Many scientific studies have emphasized that the key strategy for the management of weight and metabolic diseases such as diabetes is Medical Nutrition Therapy (MNT). MNT is based on achieving glycemic control by monitoring carbohydrate intake [1,2].
In 1980, the glycemic index (GI) was introduced as an alternative system for classifying (quantifying) carbohydrate-rich food according to its effects on the postprandial glucose response in 2 h, i.e., the “area under the 2-h postprandial glucose curve” [3].
Changes in glycemia after the ingestion of equivalent carbohydrate exchanges can vary widely. However, the diet that produces a low glycemic response is associated with significantly less insulin resistance and lower prevalence of the metabolic syndrome [4], risk of type 2 diabetes [5-8] risk of ischemic heart disease [9], and reduction of the lipid profile [10].
Many studies consider the GI a very important factor [4-10], but others do not consider it a useful dietary planning tool for weight management or disease prevention [11-13].
The use of the GI for the classification (low, ≤ 55; medium, 56–69; high, ≥ 70) [14] of carbohydrate-rich food has been endorsed by the US Food and Agriculture Organization/World Health Organization (FAO/ WHO) and the American Diabetes Association. It was recommended that, for individuals who wanted to make extra effort in monitoring their food choices, the GI be combined with the carbohydrate composition (“carb counting”) of food to achieve blood glucose goals [11,15,16].
Study justification
According to the International Diabetes Federation Atlas statistics, the prevalence of diabetes in the United Arab Emirates (UAE) is very high [17]. The major factor that could further increase the prevalence of diabetes is an unhealthy lifestyle [18].
Based on our clinical observations, the daily consumption of bread is a deeply rooted tradition in many societies, including those in the UAE, as it is a main component of most meals. Some traditional bread is prepared at home daily. In addition, commercial breads are bought from local bakeries.
In 2004, Allison’s study found that the only way to reduce dietary GI while maintaining a high carbohydrate intake [11] was to substitute white bread with low-GI bread, and this could reduce the risk of type 2 diabetes [19].
As far as we know, there is no published data on the GIs of traditional breads (rigag, chbab, and khameer) commonly consumed in the UAE.
It is impossible to predict the GI of a particular food from the published value for a food of similar description [20], as many factors could influence the GI of a particular food [21]. This is why it is important to measure the GI of a particular food rather than estimating it.
Thus, this study aimed to measure and evaluate the composition and GIs of 3 commonly eaten traditional breads and to compare them with 3 commercial breads widely consumed in the UAE. In addition, we discuss the factors that contribute to the differences among the GIs of these breads in comparison with previously published data.
The results may help the diabetic, the obese, and their healthcare providers, e.g., dietitians and diabetologists, develop diets that are appropriate both medically and culturally. In addition, our results hold significance for researchers seeking to quantify the GI of the UAE traditional diet.
Subjects and methods
We recruited 16 healthy subjects, but 14 subjects completed the study (2 dropped out; 7 women and 7 men) (Table 1) [22]. Potential subjects were excluded if they reported a history of gastrointestinal disorders (e.g., celiac disease), suffered from diabetes, were taking medication for any chronic disease conditions, pregnant, breastfeeding, or intolerant or allergic to any type of food [15].
| Mean | SD | |
|---|---|---|
| Age (years) | 29.5 | ± 6.6 |
| Height (m) | 62.6 | ± 19.1 |
| Weight (kg) | 161.3 | ± 7.8 |
| BMI (Kg/m2) | 23.91 | ± 2.4 |
(Mean values and standard deviations for 14 subjects)*
Table 1: Characteristics of study population.
The study was conducted at the Rashid Center for Diabetes and Research in the UAE. The method used to measure and calculate the GIs of the breads was in accordance with WHO/FAO recommendations [15]. The study spanned 3 weeks, comprising 5 testing sessions every week. The subjects (n=14) attended each testing session after an 8- to 10-hour overnight fast, having been instructed not to consume unusually large meals, drink alcohol, or exercise vigorously on the previous day, and to avoid cycling or walking to the center.
On the first 3 testing days, the subjects were served with the standard reference food (EasyDex 50 g glucose concentration; Aeromed, Glastonbury, CT, USA). On the remaining testing days they were served the bread (one type per testing day) that had been randomly assigned to them and asked to consume it within 15 minutes. As 300 mL reference glucose syrup was provided, the subjects were given 300 mL of water to drink with the tested bread. Each bread was tested by 7 different subjects [15]. Each subject tasted 1–4 breads.
A qualified technician performed the blood glucose measurement. A fasting blood sample was obtained at 0 min (fasting), and the reference/ test food was consumed immediately after this. Then, we measured the glucose level in capillary blood [15,23,24] obtained by finger prick using a OneTouch UltraEasy glucometer (Johnson & Johnson [Middle East] Inc., USA). Blood samples were collected at 15, 30, 45, 60, 90, and 120 min after initiating reference/bread consumption, and stopwatches were used to ensure accuracy.
Experimental bread and portion size
We tested 6 breads widely consumed in the UAE, which consisted of 3 traditional breads: rigag, chbab, and khameer. The other 3 breads were commercial breads: white pita bread (khobuz), white bread roll (summon), and whole-meal bread.
Rigag is thin, unleavened bread, the batter of which comprises flour (70% whole-meal flour with 30% white flour), salt, and water, and is cooked on a hot metallic surface.
Chbab is made by combining flour (50% white flour and 50% whole-meal flour), water, egg, sugar, vegetables oil, and yeast. The batter is very thin due to the large amount of water used. It is baked by pouring the batter on a hot flat pan, and vegetable oil is added at the last stage of cooking to the top of the bread to brown the surface. This bread is well known because of its surface, which is full of air bubbles similar to the ones in pancakes.
Khameer is prepared by mixing flour (100% white flour) with eggs, yeast, sugar, vegetable oil, and ghee, and proving the dough in a warm place until the volume increases (yeast effect). Flat portions are formed; the surface covered with egg yolk and sesame, and it is baked on a flat pan.
The other 3 breads (khobuz, summon, and whole-meal bread) are prepared commercially in local bakeries.
Fresh bread samples were placed in sterile plastic bags and sent to the Dubai Central Laboratory (Food and Environment Laboratory Section), UAE, for nutrient analysis. All results are presented as the percentage in 100 g of the total bread weight. Based on these results, portion sizes were calculated to provide 50 g available carbohydrate [15] (Table 2).
| Bread name | Portion Size (g) |
| Rigag bread | 98 |
| Chbab bread | 105 |
| Khameer bread | 92 |
| White bread | 98 |
| White Samoon | 88 |
| Whole meal bread | 120 |
Table 2: The portion size which contains 50 g of available carbohydrates.
Ethics
A UAE Ministry of Health Research Ethics Committee approved the protocol used in this study. Each subject signed an approved consent form after a short interview. The procedures involved and the role of the subject (those who met the inclusion criteria) in the study were explained during the interview.
Each subject was assigned a code number unique to this study. The list of subjects and all the material related to this study were kept in a locked file in the hospital information system. After the data were collected and analyzed, the list of the participants’ names and their code numbers was destroyed. The study findings are presented only in summary form and names will not be used in any report.
Statistical method and data analysis
In our study, the GIs of the specific breads were calculated in 4 steps.
First, we calculated the incremental area under the curve (IAUC) in a subject (reference/tested bread) (as the sum of the surface of triangles and trapezoids between the blood glucose curve and horizontal baseline parallel to the X-axis from the beginning of blood glucose at time 0 to 120 min and ignoring the area under fasting reading. Microsoft Excel was used) (Figure 1). Second, the mean of the IAUCR1, IAUCR2, and IAUCR3 for the reference food (50 g glucose, which was repeated 3 times for each subject) was calculated. Third, the GI (%) for each subject was calculated by dividing the IAUC for the tested bread by the mean IAUCR for the reference food and multiplying the result by 100. The following formula was used:
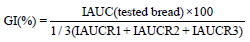
Fourth, the GI of each bread was calculated as the mean value of GI (%) across all subjects consuming that bread. The statistical significance of the differences between values was assessed using a paired t-test. P<0.05 was considered significant. Then, the bread was classified based on its GI value into 3 groups: low ( ≤ 55), medium (56–69), and high ( ≥ 70) [14].
Nutrient compositions of tested bread
The Dubai Central Laboratory (Food & Environment Laboratory Section) analyzed the nutrient compositions of all the breads. The results are presented as a percentage of each composition in 100 g of the total bread weight (Table 3).
| Bread name | Calories (Kcal/100g) | Carbohydrate (%) | Fat (%) | Total protein (%) | Moisture (%) | Crude fiber (%) | Total Ash(%) |
|---|---|---|---|---|---|---|---|
| Rigag bread | 281 | 50.9 | 2.78 | 13.1 | 29.8 | 0.67 | 2.8 |
| Chbab bread | 273 | 47.6 | 8.43 | 1.8 | 39.2 | 0.45 | 2.49 |
| Khameer bread | 352 | 54.2 | 10.6 | 9.93 | 22.7 | 0.34 | 2.19 |
| * white pita bread (khobuz) | 279 | 51.5 | 3.54 | 10.7 | 33.3 | 0.29 | 0.97 |
| *White breadroll (summon) | 292 | 56.9 | 3 | 9.33 | 28.9 | 0.21 | 1.66 |
| *Whole mealbread | 290 | 41.7 | 4.35 | 14 | 37.2 | 0.78 | 2.01 |
* The highest consumed bread in UAE (type and brands) were taken from a report of one of the biggest market in the country.
Table 3: Central food lab analysis results of 100 g of total weight of tested types of bread (%).
Table 3 shows that khameer contained the highest percentage of fat, while rigag and summon contained the lowest fat percentage (2.78% and 3%, respectively). The protein percentage was the lowest in chbab (1.8%), while it was highest in whole-meal bread (14%).
Based on these laboratory results, the available nutrient compositions (carbohydrate, fat, protein, crude fiber, and so on) in the studied portion sizes were calculated and demonstrated in table 4.
| Bread name | Calorie | Caro (g) | Fat (g) | Protein (g) | Moisture (g) | Crude Fiber (g) | Ash (g) | Studied portion size(g) |
|---|---|---|---|---|---|---|---|---|
| Rigag bread | 276 | 50 | 2.73 | 12.87 | 29.27 | 0.66 | 2.75 | 98 |
| Chbab bread | 287 | 50 | 8.86 | 1.90 | 41.18 | 0.47 | 2.62 | 105 |
| Khameer bread | 325 | 50 | 9.78 | 9.16 | 20.94 | 0.31 | 2.02 | 92 |
| white pita bread (khobuz) | 271 | 50 | 3.44 | 10.39 | 32.33 | 0.28 | 0.94 | 98 |
| White bread roll (summon) | 257 | 50 | 2.64 | 8.20 | 25.40 | 0.18 | 1.46 | 88 |
| Whole meal bread | 348 | 50 | 5.22 | 16.79 | 44.60 | 0.94 | 2.4 | 120 |
Table 4: Caloric, fat, protein, moisture, fiber and ash amount in the studied portion size, which contains 50 g of available carbohydrate.
The whole-meal bread had the highest caloric content, as well as very little crude (insoluble) fiber, while summon had the lowest caloric content. The crude fiber in all tested breads was low (<1%), and was highest in rigag and whole-meal bread.
Measuring the GI
Fourteen subjects completed the study (of the original 16, one dropped out due to personal issues and the other because of impaired glucose tolerance). Seven subjects tested each bread. The average postprandial glycemic responses of 7 subjects (reference food and each bread) over 2 h is presented in curves and demonstrated in figure 1.
The GI of the traditional breads ranged between low and medium: rigag, 48.21(15.66); chbab, 63.95(7.06); and khameer, 63.91(11.49). All GIs exhibited a significant difference (P<0.05).
However, the GIs of the other 3 breads ranged between medium and high: khobuz, 70.11(15.42) (P<0.05); summon, 73.12( 4.63) (P>0.05); and whole-meal bread , 66.71(14.68) (P<0.05).
The GIs for all tested breads are illustrated in figure 2. Rigag was the only low-GI bread (48.2), while the other 3 tested breads (chbab, khameer, and whole-meal bread) had a medium GI, and the remaining 2 tested breads (summon and khobuz) had high GIs.
The relationship between GI and fat, protein, and crude fiber
We measured the relationship between the GI and the macronutrients fat, protein, and crude fiber. The correlation between the GI and fat (r=0.04) and protein (r=0.18) was weak, while the relationship between the GI and crude fiber (r=0.48) was moderately negative (Figure 3).
Our dataset identifies the GIs of 6 breads (3 traditional, 3 commercial) commonly consumed in the UAE. As far as we know, the GIs of the traditional breads have not been determined previously, while the GIs of the commercial breads have been published.
Our clinical observation determined that very high amounts of bread are consumed in the UAE, which means that measurement of the GI of bread would contribute significantly to quantifying the GI of the UAE diet.
The study shows that the GIs of traditional bread ranged between low and medium, as the GIs of rigag, chbab, and khameer were 48.21 (low), 63.95 (medium), and 63.91 (medium), respectively. The GIs for the 3 commercial breads ranged between medium and high: the GIs of summon, khobuz, and whole-meal bread were 73.12 (high), 70.11 (high), and 66.71 (medium), respectively.
Considering the GI for recommendation of bread choice rather than caloric and fat composition, moderate consumption of a low- GI bread such as rigag might arguably be a better option than other higher-GI breads. The same applies for any other traditional bread that is low GI, and could be a better choice than khobuz or summon, which have high GIs.
The GI of khobuz has not been published in the International table of glycemic index and glycemic load values [21], but in 2005, Henry demonstrated that the GI of white pita bread was 69, which is a small difference of 1.1% from our measured value [25], which could be due to variability in the measurement of GI [26].
The GI of summon was the highest among all the breads (GI=73). No previous study has measured the GI of summon in healthy subjects. However, the GI of summon with cheese was measured in 2007, and it was 50 ± 6 [25].
The GI of the whole-meal bread in our study was 66.71, which is in the range of the measured value of whole-meal bread in healthy subjects (72 ± 6) in the International table [21], and the GI for wholemeal bread in the Aston Study in 2008 was 66 [27], which is very close to our results.
Many factors could influence GI values in food, including * methodological factors [22] and ** factors related to the tested food itself, such as its physical form, the availability of other macronutrients (e.g. fat, protein, fiber), the type of sugars and starch in the food, and the processing, preparation, and cooking methods [21,28,29].
Arguably, perhaps the most important measurable factor that could affect the GI value is the addition of other macronutrients such as fat and protein, and the availability of insoluble fiber. It would be difficult to discuss each factor separately here, as the breads contained unequal mixtures of fat, fiber, and insoluble fiber.
In the studied portion size, the relationship between the GI with fat (r=0.04) and protein (r=0.18) was very weak, while its relationship with fiber was negatively moderate (r=0.48). We found that the bread with highest GI (summon) contained the least crude fiber.
Many studies have discussed the effect of the available amounts of protein, fat, and insoluble fiber. Some studies have shown that protein may significantly reduce the glycemic response by stimulation of insulin secretion [30]. Other studies have found that fat may significantly reduce the glycemic response by slowing gastric emptying [20,31]. However, other studies have revealed that the macronutrient content per 100 g of test foods does not significantly affect glycemic response [25]. Moreover, other studies have found that the relationship between the GI and insoluble fiber is significant [32], whereas others have found that it is not [3].
All the previous discussions have highlighted the importance of testing foods in the country of consumption because the processing conditions and raw ingredients used may have a significant impact on the GI.
Our dataset describes the GI values of 3 previously untested traditional breads and 3 commercial breads commonly consumed in the UAE, demonstrating that the traditional breads have a lower GI value range in comparison to the other breads. In addition, the correlation between the GI values and insoluble fiber was negatively moderate, while that with fat and protein was weak. The difference between the GI values in our study and the previously tested items prove the importance of testing food in the country of consumption rather than assuming that it is the same as a previously published value for a similar food in another country. This data test is useful to both researchers and healthcare professionals in advising patients about their diets.
The roles of the authors are as follows: the main investigator was Areej, a clinical dietitian who prepared and reviewed the protocol and the scientific proposal, proposed the budget, and conducted the research. Merciamma, Hisham, and Shibby were responsible for blood sampling, performing the oral glucose tolerance test, documentation, and record keeping. Dr. Salah was the supervisor. None of the authors reports any conflict of interest in this study.
We would also like to acknowledge the assistance extended by engineer Arwa Ahmad from Germed Medical Marketing during data collection, and Sarah Qassim, RCDR dietician, during the final stages of writing this paper.
We thank LifeScan Middle East and Africa, a division of Johnson & Johnson (Middle East) Inc., and appreciate their contribution in providing funds for the study (glucometers, Lancets, test strips, and test meals).