Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Research Article - (2019)Volume 10, Issue 1
Introduction: Eczema is a common condition affecting children characterized by itching and inflammation of the skin which can affect the quality of life of the patient and family involved. This study is aimed at assessing the quality of life of family members with children suffering from this condition.
Methods and analysis: Two different questionnaires were used for assessment and these are Dermatitis family impact (DFI) and family dermatology life quality index (FDLQI). Twenty-seven parents were involved in the study and data was analyzed using IBM SPSS Statistics software (SPSS Inc, Chicago, IL, USA). The 2 questionnaires were then compared using student’s T-test. Different family units were compared using one-way ANOVA.
Conclusion: The mean FDLQI was 19.8 ± 5.4 S’s with a range of 10-30 which is classified as having an extremely large effect on the parent’s life. The mean DFI score was 20.6 ± 5.70 which is also classified as having an extremely large effect on the parent’s life.
FDLQI; DFI; Eczema; Psychosocial impact
Eczema is a chronic inflammatory skin disease characterized by pruritus and dry skin, commonly affecting the flexural regions but can also affect the face, neck, truck and extensor surfaces in children and infants [1]. The most common subtype is atopic eczema which commonly develops during the first few months of life and is the most common inflammatory skin disease in children [2,3]. International studies calculating the prevalence of eczema have shown it to be particularly high in developed countries such as the United Kingdom [4,5]. This region has a prevalence of over 20% in the age groups looked at in the studies (6-7 years and 13-14 years) [4,5]. Other areas with a prevalence of above 20% include North America, Australia, New Zealand, France and Latin America [4,5]. It has been shown to have a profound effect on quality of life not only in children with the condition but in parents and family members related to the children. This is a single-center questionnaire-based study taking place in a dermatology outpatient department. It is looking at the parents of children with eczema and assessing how much impact it has on the quality of life of the family by caring for their child. The study asks parents to fill in two questionnaires: the dermatitis family impact (DFI) questionnaire and the family dermatology life quality index (FDLQI). It also asks for basic information such as age and gender.
The development of numerous questionnaires/tools to help assess the impact on quality of life of dermatological conditions has helped realize the large impact eczema can have on children, with over 25 % of children having moderate to severe health-related quality of life impairment [1,6]. Children rate sleep loss and itching (which is the predominant cause of sleep loss) as the most important factors of their eczema [7,8]. The impact of childhood eczema is thought to be so severe that some studies have found that the impact on quality of life may be higher than other chronic childhood diseases such as diabetes, cystic fibrosis, asthma and enuresis although skin diseases such as psoriasis and scabies appear to have higher quality of life impairment than eczema [7]. The sleep loss the child suffers also disturbs the parents with them estimating to lose on average 2.5 hours sleep per night, particularly during a flare-up of the disease [9]. Furthermore, 2-3 hours per day overall were found to be spent looking after a child with eczema [10,11]. This can impact on their working hours and as a result it may impact on them financially, which can further affect their quality of life [10-12]. Parents have to take more care with laundry, cleaning the house, food preparation and shopping for certain soaps and perfume products, adding more stress to their lives [2]. This impact on quality of life is made clearer when parents frequently report feelings of frustration, anger, depression, guilt and an inability to cope [9,13].
The study uses two questionnaires: the dermatitis family impact questionnaire (DFI) and the family dermatology life quality index (FDLQI) [13,14]. The former is a disease specific questionnaire specifically for the family of children with dermatitis. The latter questionnaire is designed for any dermatological condition but the questions have been altered slightly to be more specific to eczema. Both questionnaires consist of ten questions and produce quantitative results with a minimum score of 0 and a maximum score of 30, with the higher number indicating a higher impact on quality of life [13,14]. Each item/ question can be scored from 0 to 3. The DFI asks parents about how they have felt over the past week whereas the FDLQI asks about the past month. Questionnaires allow for the collection of a significant amount of data from a large group of participants using up a short amount of their time. There is minimal impact on the participant and no personal data is collected due to the ability to collect data anonymously. Furthermore, both the DFI and the FDLQI have been validated in papers published in peer reviewed journals [2,15]. This not only justifies their usage but allows for easy comparisons with previous papers that use the same questionnaires.
Objective
• Understand the impact of childhood eczema on the parents/family of the child as measured by the FDLQI and DFI
• Determine any correlations between age, gender, occupational status and family unit type with FDLQI score.
This was a single-centre questionnaire-based study involving parents of children presenting to a pediatric outpatient dermatology clinic in New Cross hospital, Wolverhampton, United Kingdom. Parents of children with diagnosed eczema were identified and approached by their child’s consultant dermatologist and asked whether they would like to take part in the study. Willing participants were then asked to fill out both the FDLQI and DFI questionnaires anonymously. Participants were also asked general questions about their age, gender, whether they were working or unemployed, and their family unit type. Family units consisted of: one parent/caregiver employed, both parents/carers working, both parents/carers not working and a single parent family. The purpose of this was to identify potential subgroups whereby parents may need extra or less support. For example, a study found that it was the mother, who tended to be the primary care-giver, felt more stress/impact on their quality of life than the father or other members of the family [16]. Furthermore, a single parent family or younger parent might have a higher impact. If this were the case then they would need more intensive support than another group that might have had a lower impact on their quality of life.
The questionnaire results were inputted onto a spreadsheet and their overall scores were then calculated. As both the questionnaires were anonymous (the patient was asked not to put any identifying information on the answer sheet), none of the parents were followed up. The primary outcomes measured were the DFI and FDLQI scores produced by the parents. Secondary outcomes included age, gender, family unit type and whether they were employed or unemployed. Parents who lacked capacity or who were under 18 were excluded from the study. Data was analyzed using IBM SPSS Statistics software (SPSS Inc, Chicago, IL, USA). Average index scores are expressed as a mean plus/minus the standard deviation (SD).
Mean average score for the two questionnaires was compared using independent Student’s t-test. This was also used to compare subgroups in each questionnaire. Average scores of different family units were compared using one- way ANOVA. Correlation between the two indices was calculated using Spearman’s rank test. P value of <0.05 was considered statistically significant.
Overall 27 parents took part in the study. Of these parents, 15 completed the FDLQI, 7 completed the DFI and 5 completed both sets of questionnaires.
Family dermatology life quality index (FDLQI)
The mean FDLQI was 19.8 ± 5.4 (standard deviation) with a range of 10-30. This average score is classified as having an extremely large effect on the parent’s life. The highest scoring question in the questionnaire was, “I have spent time putting on creams and/or giving medicines to my child,” with a mean score of 2.8 ± 0.41. With “My physical well-being has been affected by my child’s eczema (e.g. feeling tired) scoring 2.45 ± 0.75 and “I have increased housework such as cleaning due my child’s eczema” scoring 2.375 ± 0.58. There was no statistical difference in FDLQI score between those working and those not working. (Independent Students T-test, mean difference 1.75, 95% Confidence Intervals -3.89283 to 7.39). Furthermore, there was no significant difference (one-way ANOVA, p=0.121) in FDLQI score between the different family unit types (Table 1).
| N | Mean | Standard Deviation | Standard Error | |
|---|---|---|---|---|
| One parent working | 6 | 19.3333 | 7.44759 | 3.04047 |
| Both parents working | 12 | 19.7917 | 3.22954 | 0.93229 |
| Both parents not working | 1 | 12 | ||
| Single parent family | 1 | 30 | ||
| Total | 20 | 19.775 | 5.42042 | 1.21204 |
Table 1: This table compares the family dermatology life quality index score in different family unit groups in terms of means, standard deviations and standard errors.
Dermatitis family impact (DFI) questionnaire
The average DFI score was 20.6 ± 5.70. This score is classified as having an extremely large effect on the parent’s life. The range was 13-30. The highest scoring question in the questionnaire was, “how much effect has your child having eczema had on causing emotional distress such as depression, frustration or guilt,” scoring 2.58 ± 0.51 on average. The next highest was, “how much effect has your child having eczema has on housework, e.g. washing and cleaning” and, “how much effect has helping with your child’s treatment had on the main carers life” both scoring 2.5 ± 0.67 on average.
DFI and FDLQI
Independent Student’s t-test showed no significant difference between the two average scores of the DFI and FDLQI. Five parents completed both questionnaires. Paired Student’s t-test of these 5 parents showed no significant difference between questionnaire scores. Furthermore, both questionnaires had significant positive correlation (Spearman’s rank test, p=0.01) (Figure 1).
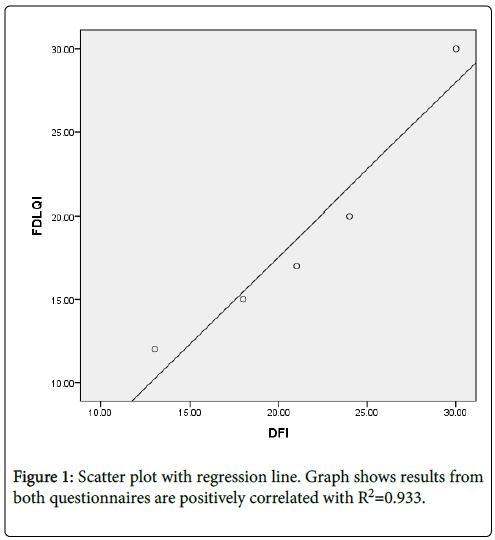
Figure 1: Scatter plot with regression line. Graph shows results from both questionnaires are positively correlated with R2=0.933.
The results clearly showed that having a child with eczema has a large impact on a parent’s quality of life. On average the DFI showed an extremely large impact on quality life whilst the DFLQI showed a very large impact on the parent’s quality of life. Notable areas which scored highly in the questionnaires were related to the physical and emotional impact on the parent, causing fatigue, anxiety, guilt, depression. This is concordant with other studies [9,13]. To tackle this, it is important that health care professionals take into account the psychosocial health of the parents and treat it accordingly. Parents may benefit from counseling or more reassurance and support from the healthcare team. Parents may benefit from advice and tips on dealing with their increased workload from caring for their child. Furthermore, a child who is unable to sleep due to severe eczema may prompt more intensive treatment. This would tie into educating parents how to treat a flare-up and the different dosages of different medication to use when the disease is more severe.
Administering treatments to the child also appeared to have a large impact on the patient’s life from the study results. Other studies have found that often parents receive conflicting advice from health workers as well as friends and family, which contributes to their anxiety [9,13,17,18]. Furthermore, lack of knowledge about treatments and the possible side effects is thought to contribute significantly to noncompliance of the child and failure of the treatment [13]. Better patient education of treatments forms a vital part of reducing the impact of treatments on parent’s quality of life [19]. Not only will it help the parents but also help control the child’s eczema. Techniques of educating parents include leaflets, videos showing them how to administer topical therapies, nurse specialists and doctors going through with the parents exactly how to put the creams on and when to use each one. Education on the side effects of steroid therapies is also important and many parents feel anxious with administering it to their children [15,20]. Although no significant difference between FDLQI score and family type was found, Table 1 did suggest some possible associations.
The single parent family has the highest possible score of 30 and the child whose parents were both not working has the lowest average of 12. It would be a logical hypothesis that a single parent family, where the responsibility of child care falls on a single parent, the impact of a child having eczema would be higher than a two-parent family. Contrastingly, the family with two parents not working had a below average score of 12. Whilst below the average, this number is classified as having a very large effect on the parent’s life (with 11 being the cut off between very large and moderate). Hence, the impact is still high. However, it might be less than other parents’ as with both parents not working they may have more time to administer treatments to their child and so not be as stressed and fatigued. There is only one participant who fell into this category so it is hard to draw conclusions from it. The lack of any difference between genders could also be attributed to the small sample size. However, a study assessing gender differences in quality of life impact also found no difference in impact between the mother and father. In conclusion child eczema has a significant impact on families involved and many aspects of it have to be addressed as part of the management [21].
Citation:
Al Abadie MS, Sheikh Z, Al-Rubaye MS, Al Abadie D (2019) The Impact of Child Eczema on Family Members Assessed by 2 Different Quality of Life Assessment Tools. J Clin Exp Dermatol Res 10: 480.
Received: 18-Oct-2018 Accepted: 20-Dec-2018 Published: 10-Jan-2019
Copyright:
© 2019 Al Abadie. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.