
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2021)Volume 12, Issue 7
Objectives: High risk surgical patients are prone to experience complicated outcomes that directly lead to longer days on ventilators and consequently longer ICU and hospital stay. PCO2 gap has elicited an increasing interest in directing resuscitation towards optimizing CO2 gap. Thus, we aimed to compare the impact of PCO2 gap targeting protocol to a classical Goal Directed Therapy Protocol (GDT) on ICU stay Ventilator day and length of hospital stay, in high-risk surgical patients admitted to ICU.
Design: Blinded prospective randomized clinical trial.
Settings: Qena University Hospital.
Patients: 80 patients who have high risk surgical criteria adopted from Shoemacker et al score and were admitted to ICU postoperatively, were divided into two groups: in group (A) PCO2 gap algorithm was applied 12 h postoperative with end point PCO2 gap 2-6 mm Hg ,and in group (B) goal directed therapy protocolwas applied 12 postoperative targeting endpoints: MAP >65mmHg, CVP between 8-12 cmH2O, Haematocrite value more than 30, SvO2 >75% and urine output more than >0.5 ml/kg/hr.
Measurements and results: Regarding duration of ventilator dependency, ICU stay and hospital stay, all values were lower in group a compared to group B although it was statistically insignificant.
Conclusion: In high risk surgical patients in ICU, targeting PCO2 values has no significant difference to early goal directed therapy regarding the decrease in ventilation days, ICU stay or hospital stay.
Haematocrite; Cardiac index; Anesthesia; Intensive care unit
Impaired tissue oxygenation in critically ill patients may be due to multiple factors could progressively lead to adverse outcomes such as organ dysfunction, organ failure, prolonged stay in Intensive Care Unit (ICU) and in hospital and increased mortality [1]. Early detection of tissue hypoxia and maintenance of adequate tissue oxygenation are considered the key elements in the care of critically ill patients. Optimization of hemodynamics and improvement of both metabolic status and tissue oxygenation are primarily addressed via “goal-directed” therapies [2,3]. Unfortunately, the adequacy of tissue perfusion remains difficult to assess. A broad use of monitoring tools and parameters has been reported to help clinicians in resuscitation of critically ill patients, but their non-specificity to tissue hypoxia exploited the need for additional markers to be investigated [4]. The difference between venous carbon dioxide and arterial carbon dioxide pressure (pCO2 gap) has been described as a parameter reflecting tissue hypo perfusion in critically ill patients who are insufficiently resuscitated. The pCO2 gap/CavO2 ratio has also been introduced as an indicator of the respiratory quotient, thus the relationship between DO2 and VO2 [5,6].
Most of the knowledge about the pCO2 gap and the pCO2 gap/ CavO2 ratio has come from studies in the literature on animal models or Intensive Care Unit (ICU) patients. To date, publications pertaining to the operative setting are sparse, specifically the ability of hemodynamic protocols based on the pCO2 gap measurement to decrease postoperative adverse outcomes including ICU days and length of hospital stay LOS [7]. With that thought in mind, this study was designed to compare the impact of goal directed therapy and PCO2 gap algorithm application on outcomes of high risk patients undergoing major abdominal surgery regarding ICU stay and LOS.
This was single blinded prospective randomized clinical trial that was conducted between Jan. 2020 and Mar. 2021. After approval from ethical committee of Qena University Hospitals, Qena, Egypt 85163. Eighty high-risk surgical patients who underwent major abdominal surgeries and admitted postoperatively to ICU were included in the research after obtaining written informed consent from the patients or from the patient’s legal representative. The criteria for inclusion are that of Shoemacker criteria summarized (Table 1) [8].
| Criteria | Items |
|---|---|
| Demographic criteria |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Surgical criteria |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Intensive care criteria |
|
|
|
|
|
|
Table 1: Demographic, surgical and intensive care inclusion criteria.
The participants were randomly assigned into two groups. Group (A) (n=40) ScvO2-CVa CO2 gap-guided protocol (PCO2 gap protocol) applied with 12 h postoperative (Figure 1). End point PCO2 gap aiming to keep pCO2 below 6 mmHg. When needed, readings of ScvO2, PCO2 gap, Hct, SpO2, Cardiac Index (CI) were taken every 4 hours postoperative.
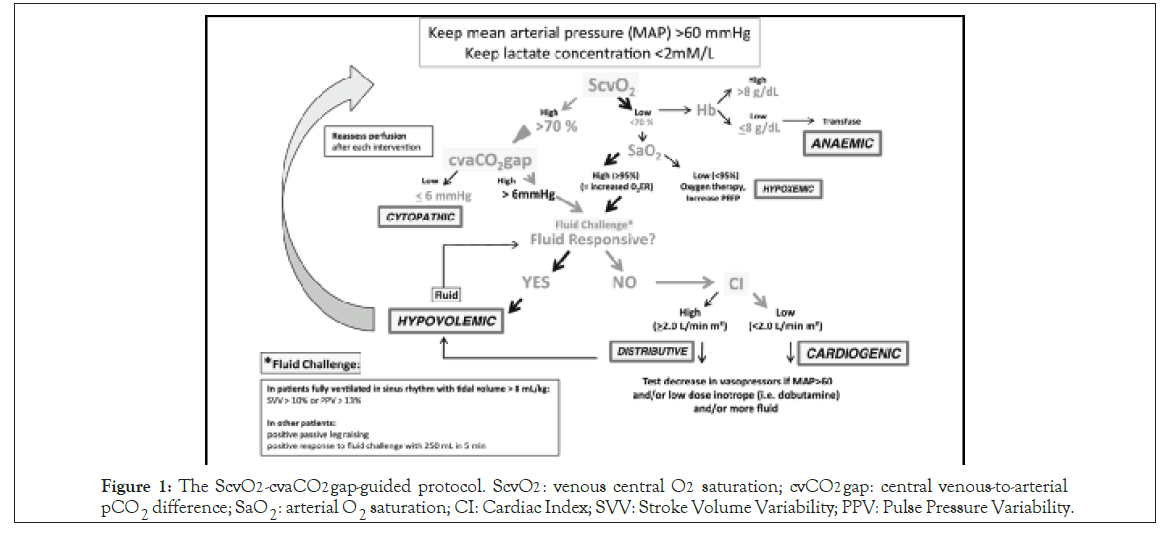
Figure 1: The ScvO2-cvaCO2 gap-guided protocol. ScvO2 : venous central O2 saturation; cvCO2 gap: central venous-to-arterial pCO2 difference; SaO2: arterial O2 saturation; CI: Cardiac Index; SVV: Stroke Volume Variability; PPV: Pulse Pressure Variability.
Group (B) (n=40): Early goal-directed therapy treatment flowchart, Kaiser Permanente Northern California, was applied 12 h postoperatively targeting MAP>65 mmHg, CVP between 8-12 cmH2O, Haematocrite value more than 30, Svo2 >75% and urine output more than >0.5 ml/kg/hr (Figure 2). Readings of ScvO2 , Hct, UOP, CVP and MAP were taken every 4 hours postoperative. All patients were admitted to ICU immediately postoperative. Monitoring included electrocardiography, noninvasive blood pressure end tidal CO2 pulse oximetry and urine output determined by insertion of urinary catheter (Foley’scatheter). for central venous pressure and mixed venous oxygen saturation monitoring during major surgery, all patients from both groups catheterized by standard three-lumen catheter central line (Certofix trio, B Braun, Germany) in the right internal jugular vein, catheter tip positioned within the superior vena cava, and correct positioning were verified by chest radiograph. For arterial sampling arterial catheters (Arteriofix, B Braun, and Germany) were placed. All patients were managed according to their allocated group. Data concerning ventilator dependency days, duration of stay in ICU and LOS were recorded.
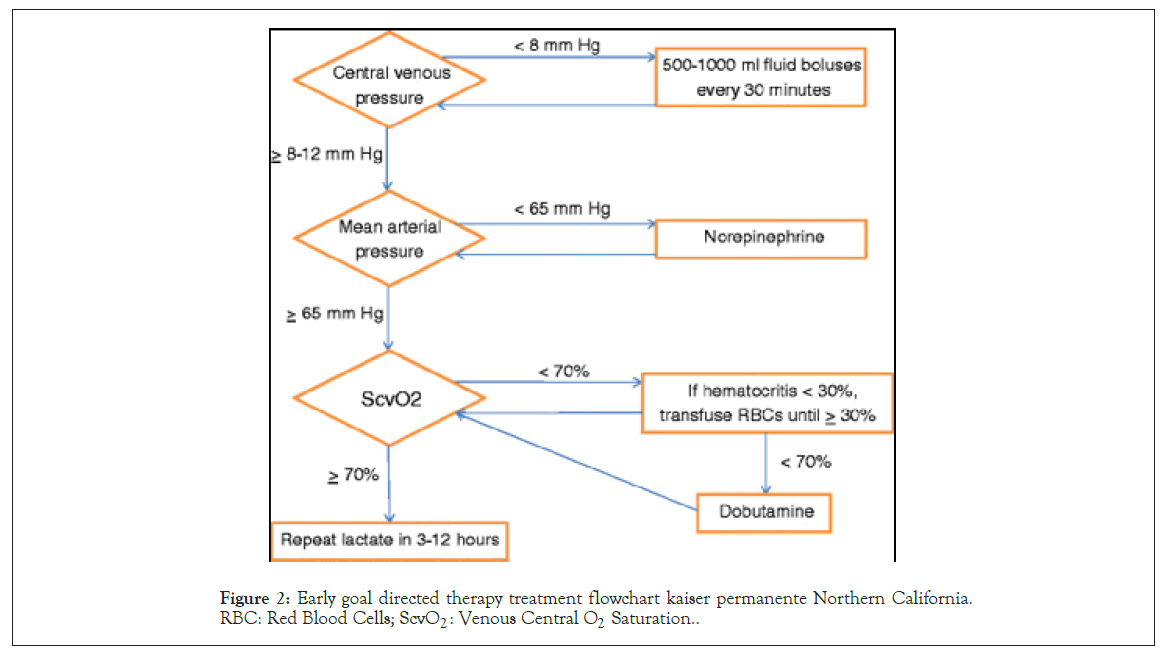
Figure 2: Early goal directed therapy treatment flowchart kaiser permanente Northern California. RBC: Red Blood Cells; ScvO2 : Venous Central O2 Saturation..
Statistical analysis
Mean and standard deviations were calculated for all quantitative variables using IBM SPSS 23.0 statistical software, P <0.05 were considered significant. All data are presented as absolute value (%), as mean ± standard. Student’s t-test was used to assess the differences between both groups in the case of a normal distribution. The chi- square test or Fisher’s exact test was used for categorical data.
The sample size was composed of 80 patients divided into 2 groups of 40. They constituted the total of consecutive high risk surgical patients in a period of 14 months. Calculations indicated a minimum sample size of 80 patients [confidence level (1-a) 95%, power level (1-b) 80%].
Regarding demographic data among study groups: Table 2 shows that the mean age of patients with GDT was 56.67 ± 12.35 years and means body mass index was 27.51 ± 7.56 kg/m2 while mean age of PCO2 group was 51.56 ± 13.67 years with mean body mass index was 27.93 ± 4.11 kg/m2. Majority (80% of GDT group and of PCO2 of enrolled patients were males. Regarding type of surgical intervention of enrolled patients, they are summarized (Table 3). The most frequent surgical interventions were exploration and resection and anastomosis. Regarding duration of ventilator dependency, it was lower in group A (0.07 ± .2) than group B (1.3 ± 2.4). ICU stay was lower in group A (2.9 ± 2.3) than group B (4.1 ± 3.8). As for Length of hospital stay it was also lower in group A (8.3 ± 3.7) compare to group B (9.9 ± 3.8). Although all these variables were lower in group A than group B, the differences were Figure 2: Early goal directed therapy treatment flowchart kaiser permanente Northern California. statistically insignificant as shown (Table 4).
| Baseline data | Group B GDT (n=40) |
Group A PCO2 gap (n=40) |
P value |
|---|---|---|---|
| Age (years) | 56.67 ± 12.35 | 51.56 ± 13.67 | 0.09 |
| Sex Male Female |
32 (80%) 8 (20%) |
30 (75%) 10 (25%) |
0.29 |
| BMI (kg/m2) | 27.51 ± 7.56 | 27.93 ± 4.11 | 0.14 |
Data expressed as frequency (percentage), mean (SD). P value was significant if <0.05. GDT: Goal Directed Therapy; PCO2 gap: Venous-Arteria Carbon Dioxide Partial Pressure Gap; BMI: Body Mass Index
Table 2: Baseline data of enrolled patients.
| Surgery | Group B GDT (n=40) | Group A PCO2 gap (n=40) | P value |
| 0.16 | |||
| Exploration | 25 (62.5%) | 24 (60%) | |
| Resection and anastomosis | 9 (22.5%) | 4 (10%) | |
| Cholecystectomy | 0 | 5 (12.5%) | |
| Intestinal repair | 2 (10%) | 2 (5%) | |
| CBD exploration | 0 | 2 (5%) | |
| Choledochojejunostomy | 0 | 3 (7.5%) | |
| Debridement | 2 (5%) | 0 | |
| Gastrojejunostomy | 1 (2.5%) | 0 | |
| Ileocecal resection | 1 (2.5%) | 0 |
Data expressed as frequency (percentage). P value was significant if <0.05. GDT: Goal Directed Therapy; PCO2: Carbon Dioxide; CBD: Common Bile Duct.
Table 3: Type of surgery of enrolled patients.
| Outcomes | Group B GDT (n=40) | Group A PCO2 gap (n=40) | P value |
|---|---|---|---|
| Ventilation days | 1.3 ± 2.4 | 0.07 ± .2 | 0.07 |
| ICU stay (days) | 4.1 ± 3.8 | 2.9 ± 2.3 | 0.3 |
| Hospital Stay (days) | 9.9 ± 3.8 | 8.3 ± 3.7 | 0.3 |
Data expressed as mean (SD). P value was significant if <0.05. GDT: Goal Directed Therapy; PCO2 gap: Venous-Arterial Carbon Dioxide Partial Pressure Gap
Table 4: Ventilation days, ICU stay, and hospital stay among study groups
The widely practiced and critically acclaimed protocols of GDT have been well received in the critical care settings. Yet, questions have been raised if their adequacy could be improved by introducing additional markers [9,10]. PCO2 gap has been proposed to better describe the correlation between systemic blood flow and global metabolic demand as it provides information that is not provided by other parameters [11,12]. The recent studies including this study have adopted this hypothesis and put it under research. The main finding of our study is that PCO2 directed resuscitation approach can decrease ICU stay, ventilator dependency days and LOS in high-risk patients who undergone major abdominal settings as effectively as conventional GDT protocol with no statistical difference between both protocols.
Robin et al. supported these results through prospective single- center observational study in a 1-year period, which included 150 high risk surgical patients total [7]. They observed that a high PCO2 gap (≥ 6 mmHg) was associated with more organ failure, longer duration of mechanical ventilation and LOS. In April 2021, Ehab Saeed Abdalazeem, conducted a study on 100 adult patients diagnosed with severe sepsis or septic shock and were divided in two groups according to ΔPCO2 [13]. The high ΔPCO2 group was associated with higher incidence of complication and organ failure than normal ΔPCO2 group. As regard the length of ICU stay and days of mechanical ventilation, they were also longer in high ΔPCO2 group although the difference was statistically insignificant.
Although these studies have demonstrated that targeting PCO2 in management of critically ill patients has an impact on lowering morbidity with hemodynamic stability, the results of a study conducted by (Pierre-Grégoire Guinot) in 2017 came in disagreement with the above findings [14]. They ran the study on 393 patients who undergone cardiac surgery with Cardio Pulmonary Bypass (CPB) and their results did not support an association between PCO2 gap and postoperative outcomes (morbidity, mortality, SOFA scores, ICU length of stay) [15]. This contradiction could be explained by the change in physiopathology of the cardiac surgical population included in Guinot study. Most relevant publications have highlighted the significant impact of CO on PCO2 gap that the PCO2 gaps represent an indicator for CO meeting the global metabolic demand, i.e. Elimination of CO2 produced by peripheral tissues [7,11,16-19]. The impact of CPB on CO2 production and acid-base balance could change the balance between partial CO2 tension and CO2 content by changing metabolic conditions, blood flow, body temperature, and alveolar ventilation.
The conflict between results could well suggest that it may be not sufficient to direct resuscitation towards PCO2 gap only. The use of PCO2 gap in conjunction with ScvO2 has also been investigated and has been shown to predict the patient's outcome better than using ScvO2 alone [20]. In a Study by Vallee 2008 it was suggested that ICU resuscitated patients, targeting only ScvO2 may not be sufficient to guide therapy [15]. They proposed that even if the target value of 70% ScvO2 is met, a P (cv-a) CO2 more than 6 mmHg could be a useful marker for inadequately resuscitated patients.
In 2020, Philippe Portran designed an original pilot study for patients who had undergone standard cardiac surgery to investigate the value of ΔPCO2 as aprognostic tool and comparing that with an existing algorithm that involves targeting values of ΔPCO2, ERO2 and lactate [21]. High ΔPCO2 (≥6 mmHg) was observed on ICU admission and on POD1 tat also failed to predict prolonged duration of stay in ICU. However, a significant increase in both ICU and hospital LOS was noted in the group of patients who were managed by the algorithm. The association between POD1 values of ΔPCO2, and POD1 variations for ΔPCO2 and ERO2 or lactate were inconclusive or absent at best, suggesting that an approach combining the ICU admission values of ΔPCO2, ERO2 and lactate could predict outcomes regarding ICU and hospital stays more effectively than ΔPCO2 alone. Recent studies published in 2019 proposed that ratio of PCO2 gap to the arterial- venous oxygen content difference also may be useful as a target for resuscitation they concluded that Pcv-aCO2/Ca-vO2 is an important predictor of postoperative major organ morbidity and mortality in patients undergoing cardiac surgery [22]. In our study, we opted for drawing samples from central venous catheter rather than PAC. Results may be different if PAC was used, but choice was in favor of feasibility and partly because PAC is not routinely used in management of high-risk patients in our ICU. Finally, PCo2 gap and the conventional markers in GDT (serum lactate, mixed venous oxygen saturation) all have different physiological kinetics and taking all these physiological differences into account may alter results but also it would be very difficult. Part of our choice of methodology was to provide practitioners with feasible simple bedside tool that according to our findings may lead to avoid longer ICU and hospital stays.
We conclude that, for high-risk surgical patients admitted to ICU, it is possible that rapid resuscitation targeting PCO2 value is as effective as early GDT resuscitation protocol, regarding the impact on duration of ICU days, ventilator days and LOS. We recommend further studies to be directed towards evaluation of the role Pco2 gap plays as a part of the different resuscitation protocols currently applied in the critical care settings, and not as a sole target for resuscitation.
Citation: Sayed G (2021) The Impact of Early Goal Directed Therapy and PCO2 Gap Protocol on Outcomes of High-Risk Surgical Patients Admitted to ICU: A Prospective Study. J Anesth Clin Res. 12:1012.
Received: 07-Jul-2021 Accepted: 22-Jul-2021 Published: 29-Jul-2021 , DOI: 10.35248/2155-6148.21.12.1015
Copyright: © 2021 Sayed G. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.