
Journal of Clinical Toxicology
Open Access
ISSN: 2161-0495

ISSN: 2161-0495
Research Article - (2012) Volume 0, Issue 0
Introduction: In the highly active anti-retroviral therapy (HAART) era, acquired immunodeficiency syndrome (AIDS)-related causes of death have declined, while non-AIDS-related causes, especially drug overdose and liver disease, have become a leading cause of death in persons with human immunodeficiency virus (HIV). Excess mortality among HIV-infected patients has been identified in those with substance use dependence. Our aim was to review the recent literature regarding the impact of HIV/AIDS on the current drug overdose epidemic with respect to the HAART era (1997 onwards).
Methods: This systematic review screened Pubmed database using search terms (HIV, AIDS, HAART, overdose, hepatitis, nephropathy, opioid, acetaminophen, methadone) and included cohort studies with derived mortality rates while excluding individual case reports, commentaries, letters, and publications over 20 years old. The crude overdose mortality rate (COMR) for each study was used to calculate a pooled COMR for each region during the post-HAART era. Calculation of 95% confidence intervals (CI) for COMR used 5% alpha.
Results: The COMR in HIV-infected persons was calculated for 17 cohort studies that analyzed cause of death in 22,414 total cases of HIV infected individuals who died from overdose in the United States, Canada, Puerto Rico, Europe, and Asia. The COMR worldwide during the pre-HAART era was 4.0% (CI 0.9-7.16) but this figure significantly increased to 17.5% (CI 12.4-22.7) during the post-HAART era. Factors that contributed to the rising COMR included: demographic factors, chronic pain, acetaminophen use, intravenous drug use, prescription drug addiction, HAART use, and end-organ disease (nephropathy, liver disease, neuro-cognitive disorder).
Conclusion: In the HAART era, AIDS-related causes of death declined, while deaths due to overdose significantly increased in HIV patients. The rise in COMR was primarily attributable to pharmaceutical drugs for pain management. AIDS-related end-organ diseases may possibly impair metabolism and physiologic responses to drug overdose. Future research should focus on expanded COMR reporting, drug misuse, and prognostic markers.
Keywords: HIV; Overdose; Mortality; Acetaminophen; Opioid; Intravenous; Prescription
An estimated one million people in the U.S. are living with Human Immunodeficiency Virus (HIV); about one-third of these cases are linked directly or indirectly to injection drug use [1-3]. In spite of substantial increases in effective HIV prevention over the past fifteen years,[4]delays in diagnosis are still problematic [5] and new HIV cases have appeared in the U.S. at a steady rate of about 56, 300 annually during the past decade [6]. In 2003, more than one quarter (11,236) of the 43,171 AIDS cases reported in the U.S involved injection drug use [7]. Although considerable progress has been made in reducing the impact of the HIV epidemic, there remains excess mortality among HIV infected patients diagnosed with substance use dependence [8].
Substance abuse is a major causative precursor to both drug overdose admissions and chronic viral illnesses such as HIV, and Hepatitis B and C Virus (HBV and HCV). Furthermore, HIV/ AIDS and overdose are two of the major contributors to mortality in intravenous drug users (IDU). In particular, there is a demand for research expanding HAART therapy coverage to reduce HIV transmission among high-risk, vulnerable populations. The “seek, test, treat, and retain” model is based on the idea that by increasing HIV testing and effective enrollment into treatment plans with Highly Active Antiretroviral Therapy (HAART), the viral load among HIV positive individuals would be reduced resulting in decreased transmission of HIV at a population level [9]. However, studies assessing the correlation between drug abuse, overdose, and HIV are challenging because of the difficulties in enrollment and retention in the most at-risk populations. As such, clinical research is needed to aggressively seek out high-risk, hard-to-reach substance abusers and to offer them HIV testing, access to treatment, and the necessary support to remain in treatment-both for HIV and for substance abuse [10].
Given the strong co-dependence between the epidemics of HIV/ AIDS and drug overdose, the goals of this systematic review are to assess the impact of HIV/AIDS on the current drug overdose epidemic. Firstly, this review will compare various studies from the United States, Canada, Puerto Rico, Europe, Asia, and Africa that address the impact of overdose on the mortality of HIV positive individuals. Using these studies we will derive an estimate of crude mortality rate due to overdose in HIV positive persons in each region. Secondly, we will review various demographic factors and comorbidities that may contribute to substance dependence and overdose in individuals with HIV. We will also discuss the impact of overdose due to prescription drugs and recreational drugs on the mortality of HIV positive persons. In addition, the impact of overdose due to acetaminophen will be discussed. Lastly, we will discuss how various end-organ diseases associated with HIV - like viral hepatitis, HIV associated liver disease, HIV Associated Neurocognitive Dysfunction (HAND), and HIV Associated Nephropathy (HIVAN) – can contribute to mortality due to drug overdose.
This systematic review summarizes the recent literature regarding the impact of HIV/AIDS on the current drug overdose epidemic with respect to the post-HAART era. The current study defined the pre-HAART era occurring prior to 1997 and the post-HAART era occurring after 1997. This year was chosen as the inflection point because several articles have shown that at approximately this point most persons for whom HAART would be recommended were prescribed HAART [11-14]. To identify the contribution of overdose on the mortality in HIV infected persons during the pre-HAART and post-HAART era literature searches were conducted. Similarly, to understand the contribution of end-organ disease on overdose mortality in HIV infected persons we conducted literature searches on HIV associated nephropathy (HIVAN), HIV/HCV associated hepatic fibrosis, and HIV associated neurocognitive disorders (HAND). We used the PubMed database as the primary source for our searches. Data pooling across studies was used to calculate the Overdose Mortality rate (OMR) per study and Crude Overdose Mortality Rate (COMR) per region, which are defined below.
HIV or AIDS or HAART AND overdose, HIV or AIDS or HARRT AND overdose AND ICU, HIV or AIDS or HAART AND opioid AND dependence, HIV or AIDS or HARRT AND acetaminophen, HIV or AIDS or HAART AND hepatitis AND toxicity, HIV or AIDS or HAART AND nepropathy AND HIVAN, HIV or AIDS or HAART AND dementia AND HAND.
The following inclusion criteria were used:
• Cohort studies on the use of prescription drugs, opioids, cocaine, amphetamines and mortality in HIV infected individuals.
• Studies in which the overdose mortality rate could be derived from the available data in the article in persons infected with HIV.
The following exclusion criteria were used:
• individual case reports, commentaries, and letters;
• studies published more than 20 years ago;
• studies published using a patient population more than 20 years ago.
Overdose Mortality Rate (OMR)
The proportion of deaths due to overdose in relation to all causes of death in HIV infected persons is defined as the overdose mortality rate. For each study the OMR was derived by the Number of Overdose Deaths divided by Total Deaths (N). The studies were categorized into the following regions: Asia, Canada, Europe, Puerto Rico, and USA.
Crude Overdose Mortality Rate (COMR)
The OMRs derived from each study were categorized into the following regions: USA, Canada, Puerto Rico, Europe, and Asia. For each region the Crude Mortality Rate was calculated by using the following formula: Σ [ (OMR) x N Total Deaths] / Σ N Total Deaths
The 95% Confidence Interval (CI) for the mean crude mortality rate was calculated using an alpha value of .05 using Microsoft Office 12 Excel (Seattle, WA).
AIDS-related Causes of Death
The causes of death that are categorized as AIDS-defining illnesses as defined by the Centers for Disease Control and Prevention are listed below:
• Candidiasis of the esophagus, bronchi, trachea, or lungs
• Cervical cancer, invasive
• Coccidioidomycosis, disseminated or extrapulmonary
• Cryptococcosis, extrapulmonary
• Cryptosporidiosis, chronic intestinal (greater than one month’s duration)
• Cytomegalovirus disease (other than liver, spleen, or nodes)
• Cytomegalovirus retinitis (with loss of vision)
• Encephalopathy, HIV related
• Herpes simplex: chronic ulcer(s) (more than 1 month in duration); or bronchitis, pneumonitis, or esophagitis
• Histoplasmosis, disseminated or extrapulmonary
• Isosporiasis, chronic intestinal (more than 1 month in duration)
• Kaposi sarcoma
• Lymphoma, Burkitt’s (or equivalent term)
• Lymphoma, immunoblastic (or equivalent term)
• Lymphoma, primary, of brain
• Mycobacterium avium complex or M kansasii, disseminated or extrapulmonary
• Mycobacterium tuberculosis, any site (pulmonary or extrapulmonary)
• Mycobacterium, other species or unidentified species, disseminated or extrapulmonary
• Pneumocystis jiroveci pneumonia
• Pneumonia, recurrent
• Progressive multifocal leukoencephalopathy
• Salmonella septicemia, recurrent
• Toxoplasmosis of brain
• Wasting syndrome due to HIV
Non-AIDS Related Causes of Death
Are those deaths not attributable to any of the AIDS-defining illnesses as listed above (e.g., acute coronary syndrome, cerebral vascular accident, infection, liver disease, malignancy, overdose, trauma, sepsis, suicide, etc.)
Asia
We identified 3 studies that analyzed a total of 1,207 deaths in HIV-infected persons (Table 1). Using population pooling, we found the COMR during the HAART era was 5.30% while the COMR during the post-HAART era increased to 19.50% (95% Confidence Interval (CI) 10.51-28.39) in Asia. The 95% CI could not be calculated for Asia during the pre-HAART period since only one study was found.
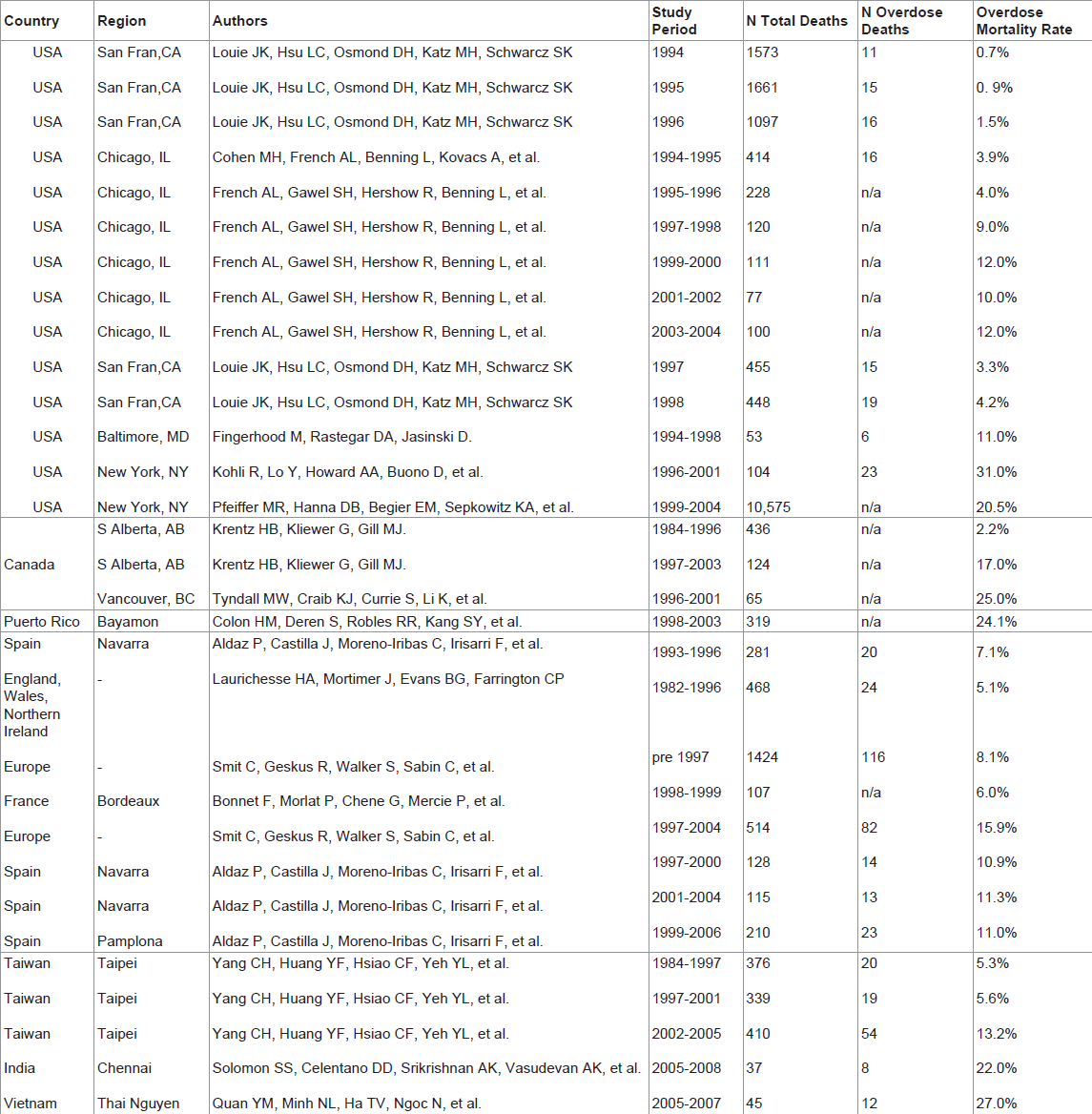 |
Table 1: Overdose Mortality Rate (OMR) Derived from Individual Cohort Studies.
Canada
Overdose mortality rates in each of 3 studies are summarized in Table 1. Using a cohort population derived from 2 analyzable studies with a total of 625 deaths in HIV-infected persons we found the COMR in the pre-HAART era was 2.20% while the COMR during the post- HAART era increased to 19.75% (11.91-27.59) in Canada. The 95% CI could not be calculated for Canada during the pre-HAART period since only one study was found.
Europe
We identified four studies and one meta-analysis, which included 22 studies across Europe, analyzing a total of 3,247 deaths in HIVinfected persons (Table 1 for summary). Using population pooling, we found the COMR in the pre-HAART era was 7.26% (5.53-8.99) while the COMR due to overdose during the post-HAART era increased to 13.63% (10.56-16.70) in Europe.
Puerto rico
The post-HAART COMR in Puerto Rico was 24.10% using one cohort study that analyzed the cause of death in 319 cases (Table 1). Insufficient studies were found to calculate the COMR during the pre- HAART era and to calculate the confidence interval.
United States
Overdose mortality rates in each of 6 studies are summarized in Table 1. Using a pooled population derived from 6 studies analyzing a total of 17,016 deaths in HIV-infected persons we found that the COMR in the pre-HAART era was 1.36% (0.03-2.79) while the COMR during the post-HAART era increased to 19.75% (11.91-27.59) in the United States.
We identified 17 cohort studies that analyzed the cause of death in 22,414 cases of HIV infected individuals who died from overdose in the United States, Canada, Puerto Rico, Europe, and Asia. Insufficient studies were found to derive the overdose mortality rate for South American and African countries. We found that the COMR worldwide during the pre-HAART era was 4.03% (0.90-7.16) where as the crude overdose mortality rate increased to 17.54% (12.42-22.66) during the post-HAART era. Regional COMR and pooled analysis are summarized in Figure 1 and Table 2.
| Crude Overdose Mortality Rate | USA (95% CI) | Canada (95% CI) | Europe (95% CI) | Puerto Rico (95% CI) | Asia (95% CI) | Mean (95% CI) |
|---|---|---|---|---|---|---|
| Pre- HAART | 1.36% (0.03-2.79) | 2.20% (n/a) | 7.26% (5.53-8.99) | n/a | 5.30% (n/a) | 4.03% (0.9-7.16) |
| Post-HAART | 18.96% (13.39-24.53) | 19.75% (11.91-27.59) | 13.63% (10.56-16.70) | 24.1% (n/a) | 19.5% (10.51-28.39) | 17.54% (12.42-22.66) |
Table 2: Crude Overdose Mortality Rate (COMR) During the Pre-HAART & Post-HAART Era.
Increasing Mortality due to Overdose since the Introduction of HAART
The major findings of this systematic review are that the crude overdose mortality rate worldwide has significantly increased in the post-HAART era. Prior to the introduction of ARV and HAART, HIV patients died from AIDS-related disease primarily, like opportunistic infections and AIDS related malignancies After ARV came to the market, overdose became a leading cause of death in HIV+ patients -and is some cases the number one cause- as death due to AIDS-related causes declined in the U.S., [16-24] Canada, [25,26] Latin America, [27] Europe, [28-35] Asia, [36-39] and Africa [40]. Currently, intravenous drug users (IDU) with HIV are more likely to die from overdose, liver disease, or other non-AIDS-related causes, while in the early HAART era they were more likely to die from AIDS-related causes. The beginning of the HAART era differed between country to country, but in most developed countries it began in the mid nineties. In 1996 the International AIDS Society-USA(IAS-USA) provided the first HAART guidelines for HIV-1 infected adults in the developed world. Many studies have cited 1997 as the approximate beginning of the HAART era [41-44]. After the introduction of HAART, death due to AIDS related diseases, which includes the AIDS defining opportunistic diseases and AIDS associated malignancies, have dropped dramatically throughout the world, while death due to non-AIDS related conditions, like drug overdose and liver disease, have risen to become the top causes of death in persons infected with HIV.
United States: Our main findings in the United States indicated a significant increase in the COMR in the post-HAART era. A major study analyzing the causes of mortality in 53 HIV patients followed at a primary care clinic in Baltimore, Maryland between 1994 and 1998 found that of those who died, HIV was the cause of death in a little over half of patients (55%) followed by liver disease (15%) and drug overdose (11%) [45]. After the widespread use of HAART in the U.S. less HIV patients were dying from AIDS-related disease. A study from San Francisco analyzing a total of 5234 deaths among men with HIV from 1994 to 1998, showed a decline in the rate of HIV- or AIDS-related deaths and an increase in the proportion of deaths associated with non–HIV or non–AIDS-related causes, likely reflecting the beneficial effects of HAART in this population. In 1996 the most common cause of death in this population of males in San Francisco were non-AIDSrelated malignancies (33%) followed by death due to drug overdose (18%) [46].
Another study showed that accidental drug overdose is the primary cause of death in IDU with HIV. This study assessed the cause of mortality in 10,575 IDU with HIV who died between 1999 and 2004 in New York City and showed that accidental drug overdose was the most frequent contributing cause of death among IDU with HIV [47]. Another study done during the period of 1996-2001 in New York City that analyzed a total of 104 deaths in persons with HIV showed that among the HIV-infected participants, 20.5% of the deaths were due to substance abuse during the post-HAART era [48].
Over the decade, the trend in decreased mortality due to AIDS and increased mortality due to overdose and other non-AIDS causes has also been observed in women with HIV. A study enrolling women with HIV between 1994 to 1995 analyzing a total of 414 deaths in HIVinfected persons found that only 3.9% of the deaths were attributed to overdose. This study also showed a steep drop in all cause mortality in 1996 (26% annual decrease) with a similar slope drop with AIDS-related death (39% annual decrease). The decrease in death from non-AIDSrelated deaths had less of a decrease (10% annual change). Again the top two causes of non-AIDS-related death in this subpopulation were liver failure followed by overdose. This study showed that the majority of women enrolled in this study (80%) were still dying primarily from AIDS-related death [49].Over the decade, the rate of non-AIDS-related death in women with HIV increased. A second study analyzing a total of 636 deaths in persons diagnosed with HIV, from a representative U.S cohort, showed that over the decade the cause of death from non-AIDS causes now accounts for the majority of deaths. This study showed that in 1995-1996 four percent of the deaths in HIV-infected women were due to overdose, while in 2003-2004 the percentage of deaths due to overdose increased to 12% while the proportion of deaths due to AIDSrelated causes dramatically decreased over the decade [50].
Canada: Overall, we found a significant rise in the Canadian COMR for the post-HAART era. Thus, the trend of increasing mortality due to drug overdose in persons with HIV appears consistent across the North American continent. Using a cohort population derived from 2 studies that analyzed a total of 625 deaths in HIV-infected persons we found the proportion of deaths due to overdose in the pre-HAART era (prior to 1997) was 2.2% while the percentage of deaths due to overdose during the post-HAART era (1997 onwards) increased to 19.8% in Canada. One study from Southern Alberta, Canada between 1984 to 2003 analyzing 560 deaths in HIV positive individuals showed that deaths from AIDS-related causes have decreased significantly, but deaths from non-AIDS-related conditions have increased. In the pre-HAART era 90% of all deaths were AIDS-related while only 67% were AIDS-related in the current HAART era. The proportion of non- AIDS-related deaths increased from 7% pre-HAART to 32% in the late ninties. During 1984 to 1996 only 2.2% of the deaths were due to drug overdose while during 1997 to 2003 the proportion of deaths due to drug overdose increased to 17%. Drug overdose was the leading cause of non-AIDS-related death, followed by hepatic disease, non-AIDSrelated malignancies, and cardiovascular disease [51]. A study from British Columbia assessing the cause of death in 65 IDU with HIV found that the leading cause of death was overdose accounting for 25% of deaths [52].
Similarly, over half of HIV positive patients admitted to Intensive Care Units (ICU) in British Columbia had a history of drug and alcohol dependence[53].A study in British Columbia done in 2 teaching hospitals between January 1999 and January 2006, using a total of 7,015 ICU admissions, of these 309 were HIV-positive, found that 56% (173 of 309) of the HIV patients had drug or alcohol dependence, whereas only 7.4% (502 of 6706) of the HIV-negative group were dependent on drugs or alcohol. In contrast, a study done in 1995 using a total of 65 ICU admissions found that only 8% of the ICU admissions were related to drug use. The vast majority of the admissions in this early or pre-HAART era was due to AIDS-related diseases caused by either AIDS defining opportunistic infections or by malignancies associated with AIDS presenting as respiratory failure (54%) sepsis (15%) or neurological disease (12%) [54]. This study analyzed the cause of admission for all the HIV patients who were admitted to an ICU in an academic medical center in New York City between November 1, 1991 and October 31, 1992 (65 HIV patients were admitted to the ICU out of a total of 1,550 total hospital admissions for HIV patients during this study period).
Puerto Rico: Unfortunately, insufficient studies were found in order to derive the pre-HAART mortality rate for this country. One study from Puerto Rico published in 2006 compared the mortality in a population of 637 Puerto Ricans who are intravenous drug users (IDU ) residing in New York to a population of 319 Puerto Rican IDU residing in Puerto Rico and found that the later group was more at risk of dying from drug overdose. In Puerto Rican IDU residing in NYC, 50% of the deaths were from AIDS-related deaths while the leading cause of death other than AIDS was drug overdose at 13%. Puerto Rican IDU residing in Puerto Rico were less likely to die from AIDS-related deaths (37%) but more likely to die from drug overdose (24.1%) as compared to Puerto Rican IDU residing in New York [55].
Europe: Many European studies confirm the trend of decreasing mortality due to AIDS-related causes in persons with HIV while deaths from non-AIDS-related causes are on the rise. Using a pooled population derived from all studies across Europe, we found a significant increase in the COMR in the post-HAART era. In one large study in Spain, mortality by cause of death was analyzed for the period 1999-2006 in the cohort of persons aged 20-59 years diagnosed with HIV and residing in Navarre, Spain. The causes of death were grouped into the following categories: AIDS or HIV infection or the non-AIDS related causes like hepatic disease, non-AIDS defining cancers, drug addiction or overdose, cardiovascular disease, and suicide. There were 210 deaths among 1145 persons diagnosed with HIV. About 50% of the deaths in HIV patients were not primarily AIDS-related deaths. The risk factors most associated with excess mortality in non-AIDS-related deaths are hepatic disease (standardized mortality ratio (SMR) 69.0, CI: 48.1 to 78.6) and drug overdose or addiction (SMR 46.0, CI: 29.2 to 69.0) [56].
A study done in England, Wales, and Ireland analyzing the cause of death in 468 HIV-infected persons who died between 1982 to 1996 found that the majority of the deaths were due to AIDS-related causes and only 5.1% of the deaths were due to overdose in this pre-HAART era [57]. A French study done in Bologna that analyzed the cause of death in 107 persons diagnosed with HIV between 1998-1999 found that AIDS-related events are no longer the major causes of death in HIVinfected patients in the era of HAART. More than half of the deaths were attributed to non-AIDS related causes; the major contributors were hepatitis B- or C-associated cirrhosis (14%), non HIV-related malignancies (11%), cardiovascular events (10%), and suicide and overdose (6%) [58]. A study from Italy assessing the mortality rates in a retrospective cohort of 3,753 IDU attending public treatment centres in the metropolitan setting of Bologna who died between 1978 to 2004 showed that death due to overdose became the primary cause of death in 1997 coincidently as the overall mortality rate owing to AIDS-related causes decreased substantially [59]. In Italy excess mortality of AIDS and overdose was found to be most concentrated on the lower social strata and in young adults [60]. A larger study using a cohort derived from 22 different studies across Europe analyzing the cause of death in 1,938 HIV-infected persons which occurred either in the pre-HAART era (pre-1997) or in the post-HAART era (1997 onwards) found that percentage of deaths due to overdose doubled (from 8.1% to 16%) after the introduction of HAART [61]. These studies further demonstrate that while death due to AIDS-related causes have decreased since the introduction of HAART, certain causes of death that are not primarily AIDS-related, like drug overdose and liver disease, are becoming major contributors to mortality in persons with HIV.
Asia: Many developing countries in the East have also seen an increase in death due to overdose in HIV patients since the use of HAART has become available in these countries. Using a pooled population across all studies we found a significant increase in the COMR in the post-HAART era (5.3% to 11.24% ). A Taiwanese study assessing the causes of death among 1,125 HIV-infected patients who died between 1984 to 2005 was done in three different study periods: before the introduction of HAART (pre-HAART: from 1 January 1984 to 31 March 1997), in the early HAART period (from 1 April 1997 to 31 December 2001), and in the late HAART period (from 1 January 2002 to 31 December 2005). In the pre-HAART era 76% of deaths were attributable to AIDS-related causes, compared with 36% in the late- HAART era. The proportion of death due to overdose during the early- HAART era was 5.3% and increased to 13.2% in the late-HAART era. Throughout the study periods the causes of non-AIDS-related death (sepsis, accidental death, overdose) increased to become the primary causes of death [62]. A smaller study from Vietnam assessed the causes of death in 45 IDU with HIV who died between 2005 and 2007 in Thai Nguyen province. These authors found that only one-third of the cases of death were AIDS-related, the majority of the deaths were non-AIDSrelated with drug overdose being the major contributor in this category [63]. Another study done in Chennai, India assessed the causes of death in 37 IDU with HIV between 2005 and 2008 and found that the leading causes of death were from non-AIDS related causes (62%), with overdose being the largest single contributor at 22% [64]. In resourcepoor areas where access to HARRT is not guaranteed, AIDS-related infections and malignancies may still be the primary causes of death in individuals with HIV. A study assessing the predictors of mortality in 50 HIV patients in Bangalore India between 2003 and 2005 found that recurrent diarrhea was the highest risk factor associated with mortality, followed by tuberculosis, and opportunistic infections [65]. 11.1.6). Africa: A study in South Africa using a population of 605 HIVinfected patients who were prescribed HAART in a hospital in Pretoria were prospectively followed from July 2004 to December 2006. In this population 204 of the patients had died primarily due to opportunistic infections (42.7%) and advanced AIDS (37.3% ), whereas HIV/AIDS – related cancers represented 8.3% of deaths. Other causes of death were hepatitis (2.9%) and stroke (1.5%). No cases of death due to overdose was observed in this population, but 5.9% of the deaths were attributed to lactic acidosis secondary to antiretroviral therapy (ART) related complications. There was no reported cases of patients who died of non-AIDS malignancies. Tuberculosis was a major contributor to death in this population; 42.7% of the deaths due to opportunistic infections were attributed to this disease. This study highlights the persistence of a relatively high overall mortality rate in persons with HIV living in resource poor settings, with AIDS being a major contributor to mortality, despite access to HAART, in patients who lack optimal care and live in substandard conditions [66].
Factors Contributing to Excess Mortality due to Overdose in HIV Patients
Demographic factors: Race and ethnicity, [67,68] socioeconomic inequalities, [69,70] gender, [71] and drug addiction [72-76] have been described as factors contributing to poor outcomes in HIV positive populations. For example, a study showed that American women were more likely to be dependent on prescription opioid medication, especially if they have a history of comorbidity and substance abuse history [77]. In the past, fatal overdoses were considered a predominantly urban issue but that no longer is the case. The rate of fatal overdoses in rural areas — 7.8 deaths per 100,000 people — is as high as it is in cities, where the rate is 7.9 deaths per 100,000 people [78].
Chronic pain: As HIV-infected persons are living longer they are more likely to develop diseases causing chronic pain, like neuropathy, and become opioid dependent as compared to persons who are seronegative [79,80]. In 2005, 8% of individuals with HIV had prevalent long-term opioid use, which was more than double the prevalence among HIV negative individuals [81]. A national survey of HIV primary health care providers reported that almost one-third of HIV positive patients reported having chronic pain and approximately one-fifth of them receive prescription opioid medication, at least half of these patients were addicted to their opioid prescription medications. The authors of this study found that few providers followed recommended guidelines for chronic opioid therapy in nonmalignant pain [82].
Between 1999 and 2005, the annual number of unintentional drug overdose deaths in the U.S. more than doubled—from 11,155 to 22,448 [83]. In 2002, drug overdose became the second leading cause of unintentional injury death in the nation, trailing slightly behind motorvehicle injuries [84]. Previously overdoses were primarily due to illegal narcotics, like heroin and cocaine, with most of the death occurring in urban areas. The rise in death due to overdose in recent years is primarily attributed to pharmaceutical drugs for pain management with opioids, acetaminophen, and methadone being the top culprits [85-87]. The rise in number of opioid prescriptions over the years has facilitated an epidemic of overdose of prescription pain killers as the leading cause of fatal overdoses. Earlier this decade, most of the concern was focused on oxycodone [88]. In recent years, the most common opioid attributed to mortality from drug overdose is now the pill form of methadone, which is increasingly prescribed because it costs a fraction of the cost as compared to brand versions of oxycodone [89].
Acetaminophen
Acetaminophen overdose is the leading cause for calls to Poison Control Centers (>100,000/year) and causes more than 56,000 emergency department visits, 2,600 hospitalizations, and an estimated 458 deaths due to acute liver failure each year [90]. Acetaminophen has also received much attention since it is now the leading cause of acute liver failure in the U.S. causing about 1,600 cases per year. There is controversy regarding whether HIV patients are at increased risk for overdosing on acetaminophen at therapeutic levels. Some authors have suggested that people with HIV should avoid behaviors such as chronic use of alcohol or acetaminophen that deplete glutathione [91,92]. Glutathione (GSH), a cysteine-containing tripeptide, is essential for the viability and function of virtually all cells. In vitro studies showing that low GSH levels both promote HIV expression and impair T cell function suggested a link between GSH depletion and HIV disease progression. It has been shown that there is a progressive decrease in baseline CD4 glutathione levels throughout the progression of HIV disease [93].
Effect of HIV on Acetaminophen metabolism
Some studies have shown that patients with chronic disease and immunodeficiency states, like HIV and Hepatitis have lower concentrations of glutathione (GSH) and may have decreased ability to metabolize acetaminophen into its glucoronide metabolites. One urine study found that the concentration of the glucuronide conjugate is significantly lower in AIDS patients when simultaneously compared with concentrations found in healthy individuals and symptoms-free HIV-seropositive subjects [94]. Although the previous mentioned study found a correlation between GSH levels and progression of HIV, other studies have not found a difference. For example, another urine study found that the molar concentrations of APAP and its glucuronide and sulphate metabolites were not associated with disease state in HIV/ AIDS patients versus healthy controls [95]. Some authors conclude that although low GSH levels have been observed in patients with HIV and Hepatitis, there is no convincing evidence that these populations are at higher risk for OD at therapeutic levels [96]. However, there have been reports that when acetaminophen is taken with certain ARV, i.e. didanosine, patients are at risk for hepatitis and pancreatitis even with therapeutic levels of drug [97].
Intravenous Drug Users (IDU)
HIV-infected persons with a history of intravenous drug use are more likely to become addiction to prescription opioids [98], which is especially concerning since a large proportion of HIV disease is directly attributed to intravenous use [99]. Studies have shown that there is improved survival and decrease transmission of HIV when HIV-infected persons are treated for their opioid dependence [100-103]. HIV/AIDS and overdose are two of the major contributors to mortality in IDUs. Drug addiction has been linked with risky behaviors such as needle sharing and risky sexual behavior, like promiscuity and unprotected sex, which are associated with increased transmission of HIV [104-106]. An estimate of the crude mortality rate of IDU from AIDS-related causes is estimated to be 0.78% per year, while the non- AIDS mortality rate is estimated to be higher at 1.08% per year [107]. Furthermore, studies have shown that treating opioid dependence in HIV positive individuals reduces transmission of HIV [108-111]. Treating withdrawal symptoms may be as important as treating opioid dependence. When patients do not have adequate treatment of their opioid dependence, withdrawal symptoms have been linked to a fivefold increase risk of death in treated HIV patients [112]. Clinicians should not be hesitant to aggressively treat opioid dependence; there is little harm in treating opioid dependence in HIV patients. Therapeutic doses of buprenorphine/naloxone have been shown to be safe and do not produce measurable hepatic toxicity in opioid-dependent patients with HIV [113] . However, antiretrovirals (ARV) may increase or decrease methadone levels so patients should be monitored for withdrawal or toxicity when they start or stop antiretrovirals [114]. By offering HIV testing and treatment as well as adequate treatment for substance abuse both transmission of HIV and drug-related death can drastically be reduced.
Recreational Drug Overdose while on HAART
Some studies suggest that since certain recreational drugs are metabolized by the liver they may potentially interact with antiretrovirals [115,116]. All protease inhibitors (PIs) and nonnucleoside reverse transcriptase inhibitors are substrates and potent inhibitors or inducers of the cytochrome P450 system [117,118]. Protease inhibitors (PI) may inhibit metabolism of amphetamines, ketamine, LSD, and PCP and overdoses of these “rave drugs” while on PI, particularly ritonavir, have been reported. PI when given with midazolam or triazolam can result in prolonged sedation by inhibiting their metabolism. PI may induce or inhibit opioid metabolism, while other antiretrovirals, like nevirapine and efavirenz induce methadone metabolism, leading to opioid withdrawal [119].
End organ disease (kidney, liver, brain): HIV associated nephropathy (HIVAN), HIV/HCV associated hepatic fibrosis, and HIV associated neurocognitive disorders (HAND), all may contribute to the ability of chronically ill infected patients to respond to drug overdose.
Kidney disease: In HIV-related nephropathy (HIVAN), impaired drug clearance, may worsen drug toxicity. It has been found that the length of duration with HIV disease increases relative risk for nephropathy [120]. There is also an increase risk of HIV-related nephropathy when co-infected with viral hepatitis [121]. A study showed that patients with HIVAN there is a strong correlation with serum creatinine as an index for chronic damage on renal histology [122]. The nephropathy is thought to result from the HIV infection itself, [123] and not as a side-effect from HAART. Although, there have been case reports of overdose with indinavir (both acute and chronic) resulting in nephrolithiasis [124].
Liver disease: Some authors believe that liver disease is now the most common non-AIDS-related cause of death in HIV patients, accounting for 14%-18% of all deaths in this population and almost half of deaths among hospitalized HIV-infected patients [125]. HIV-related liver disease and coinfection with viral hepatitis is a major contributor to morbidity and mortality in persons with HIV and contributes to the mortality associated with overdose, [126-128] especially with acetaminophen. There are data that suggests that HIV-infected persons may have impaired ability to metabolize acetaminophen [129]. Mortality due to overdose is higher in HIV positive individuals as compared to HIV negative persons due to factors such as drug use behavior, systematic disease and liver damage accounting for the majority of this association [130,131]. Hepatitis C virus-Human immunodeficiency virus (HCV-HIV) coinfections are identified in up to 30% of patients infected with HIV and in 8% of patients infected with HCV [132]. Coinfection with HBV or HCV is related to an accelerated course of liver disease in HIV patients. In addition, there is a strong association between opioid dependence and liver disease, 20% opioid addicts die from liver related causes [133]. Chronic exposure to viral hepatitis, ARV-associated hepatitis, and the use of alcohol and other toxins in the setting of immunosuppression have resulted in increasing rates of end-stage liver disease (ESLD) in HIV patients.
For some patients with HIV and ESLD, liver transplantation becomes necessary. HIV disease is no longer considered an absolute contraindication to liver transplantation by most transplant centers worldwide [134]. HBV/HIV coinfected patients have successfully undergone liver transplantation with excellent results in terms of survival, control of HBV replication after transplantation and signs of mitochondrial toxicity in hepatocytes [135]. However, HCV/HIV coinfected patients require special management strategies, [136] in order to improve success after transplantation.
Brain disease: HIV-associated neurocognitive dysfunction (HAND) is recognized as common sequelae of infection. The HAND spectrum consists of asymptomatic neurocognitive impairment (ANI) to HIV-associated mild neurocognitive disorder (MND) to HIV-associated dementia (HAD). Early in the epidemic more than half of all HIV-positive patients developed HAD. With the advent of and widespread use of ARV the prevalence of HAD has decreased dramatically, while less severe ANI and MND have risen as individuals are living longer with the disease [137]. Patients with HAND may be more likely to overdose as a result of impaired behavioral control and may be more difficult to diagnose because of their altered mental status. In France, a study assessing the neurological complications in 210 patients with HIV admitted to a medical ICU between 2001 and 2008 found the predominate neurological complications consisted of delirium (45%), coma (39%), seizures (32%) and/or intracranial hypertension (21%) [138].
In the HAART era, AIDS-related causes of death have declined, while deaths due to overdose have significantly increased and become a leading cause of death in persons with HIV. The rise in death due to overdose in recent years is primarily attributable to pharmaceutical drugs for pain management with opioids (especially methadone) and acetaminophen. HIV-related liver diseases are not only major contributors to HIV morbidity and mortality, but also contribute to the mortality associated with overdose which may be explained by impaired drug metabolism (e.g., acetaminophen), decreased drug clearance, hindrance of the ability to physiologically respond to drug overdose. Future goals in HIV research should focus on improving drug dependence treatment, expanding methods to report overdoses and drug misuse, and establishing markers to prognosticate poor outcomes in order to improve clinical decision making for HIV positive patients with drug overdose emergencies.