Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Short Communication - (2024)Volume 13, Issue 5
Fluorescence-guided open radical prostatectomy with enhanced nerve visualization. Prostate cancer exhibits very high incidence and mortality worldwide. According to a recent publication-The Lancet Commission on Prostate Cancer, it is projected that over the next 20 years, cases of this disease will double, with an 85% increase in associated deaths. The study estimates that between 2020 and 2040, global prostate cancer cases will rise from 1.4 million to 2.9 million annually [1].
Many efforts have been made for early disease detection, yet its incidence continues to grow alarmingly. Conversely, radical prostatectomy has been documented to provide excellent longterm survival in selected prostate cancer patients, reducing the risk of pelvic recurrence and metastatic spread [2,3]. However, during prostatectomy procedures, the cavernous nerve, which branches to provide penile innervation, may undergo compression, tension, or resection-related injury, resulting in erectile dysfunction in up to 85% of patients [4,5]. This occurs because the nerve and its branches are small, located between the prostatic capsule and the prostatic fascia, making them difficult to visualize and avoid within a confined anatomical space.
Two main factors contribute to erectile dysfunction postprostatectomy: Disease progression involving the gland and adjacent tissues, and intraoperative nerve injuries due to inadequate visualization.
Early diagnosis helps prevent dysfunction caused by disease progression. Regarding intraoperative factors, precise technique plays a important role in avoiding complications. Despite advancements such as video laparoscopy and robotic surgery, which enhance visualization and maneuverability in tight anatomical spaces, intraoperative injuries to pudendal nerves and subsequent erectile dysfunction still occur.
Moreover, these technologies are not universally accessible, with open radical prostatectomy remaining the most common procedure globally. At this juncture, the ability to visualize pudendal nerves in detail during surgery emerges as a critical challenge, despite ongoing advancements. Our team focused on enhancing nerve visualization during surgical interventions.
To achieve this goal, drawing on experiences in other anatomical areas to prevent iatrogenic nerve damage, we employed autofluorescence principles [6]. Pudendal nerves emit autofluorescence when illuminated with Near-Ultra Violet Light (NUVL), without the need for injected substances. Images were captured using a specialized camera (Dendrite™) and displayed on a high-resolution screen, highlighting nerve locations in the surgical field.
The use of this technology enabled our prostatectomy team to meticulously preserve nerves, thereby preventing erectile dysfunction and other neurological complications in the postoperative period, as documented shown in (Figures 1A and 1B).
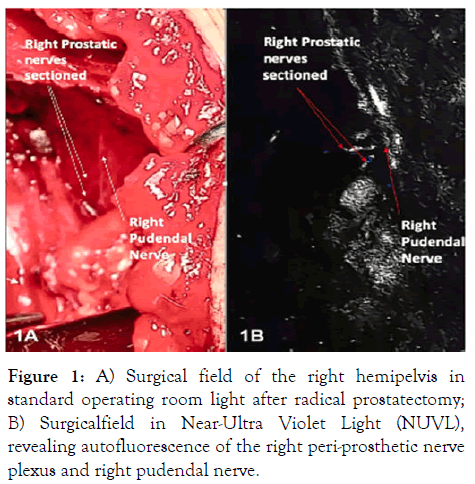
Figure 1: A) Surgical field of the right hemipelvis in standard operating room light after radical prostatectomy; B) Surgicalfield in Near-Ultra Violet Light (NUVL), revealing autofluorescence of the right peri-prosthetic nerve plexus and right pudendal nerve.
Currently, fluorescence is commonly used to delineate lymphatic areas in tumors (Sentinel Lymph Node) or demonstrate vascular perfusion of various organs following injection of different substances. However, nerves, except for major nerve trunks, are not typically visualized in this manner [7]. Thus, our innovation lies in successfully demonstrating the pudendal nerve and its branches using autofluorescence under NUVL, captured with a user-friendly, high-visibility camera.
We report a novel, simple-to-use technique that does not require injected substances, aiding in the prevention of one of the most feared postoperative functional complications related to erectile function in radical prostatectomy via the common laparotomy approach for prostate cancer, a frequent and increasingly prevalent disease. This innovation offers a crucial advancement in surgical practice, particularly in the context of prostate cancer, which is projected to see a dramatic increase in incidence and mortality over the coming decades. By improving intraoperative visualization of critical nerves, our technique holds promise for better surgical outcomes and enhanced quality of life for prostate cancer patients worldwide.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Harraca JL, Degiovanni R, Degiovanni D, Sylvestre Begnis Santiago (2024) The Importance of Improving Visualization of Pudendal Nerves during Radical Prostatectomy. Andrology. 13:326.
Received: 19-Jun-2024, Manuscript No. ANO-24-32039; Editor assigned: 21-Jun-2024, Pre QC No. ANO-24-32039 (PQ); Reviewed: 05-Jul-2024, QC No. ANO-24-32039; Revised: 21-Jul-2024, Manuscript No. ANO-24-32039 (R); Published: 19-Jul-2024 , DOI: 10.35248/2167-0250.24.13.326
Copyright: © 2024 Harraca JL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.