Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Research Article - (2023)Volume 8, Issue 6
Background: New-borns in particular, are at higher risk for Unplanned Removal of Orogastric Tube (UROGT). However, there is a lack of studies identifying the incidence and risk factors for UROGT in China.
Purpose: The objective of this study is to examine the current incident of UROGT in our NICU and risk factors that contribute to it.
Methods: This observational study was conducted in a single NICU, including 111 new-borns who received orogastric tubes between October 2022 and February 2023. The proportion and incidence rate of UROGT was analysed, subsequently the univariate and multivariate logistic models were employed for risk factor investigation.
Results: The proportion of UROGT was 56.8% and the incidence was 7.2 per 100 tube days. An increased risk of UROGT was associated with higher agitation scores Odds Ratio (OR=17.82, P=0.001), absence of oral feeding (OR=0.02, P=0.007), fixation tape loosening (OR=22.75, P=0.027) and tape wetting (OR=12.6, P=0.021).
Conclusions: The incidence of UROGT was found to be significantly higher in our NICU. New-borns with higher agitation scores, absence of oral feeding and fixation tape loosening and wetness were more likely to be at risk of UROGT.
Gastric feeding tube; New-born; Unplanned Removal of Orogastric Tube (UROGT); Neonatal Intensive Care (NICU)
Feeding tubes, including Orogastric (OG) or Nasogastric (NG) tube, are routinely employed in the Neonatal Intensive Care Unit (NICU) to support preterm or critically ill infants through enteral nutrition, medication administration and gastric decompression [1]. While NG tubes are inserted through the nose, OG tubes are passed through the mouth and into the stomach [2,3]. However, due to the small nasal passages of new-borns, inserting feeding tubes through the nose may lead to partial nasal obstruction, increasing the risk of apnea of prematurity, airway resistance and the amount of energy consumed for breathing. Based on the above reasons, in China, orogastric tubes were the preferred option prior to the introduction of nasogastric tubes in the NICU [4]. However, the increased mobility of orogastric tubes within the oral cavity also translates to a higher risk of dislodgement when compared to nasogastric tubes [5].
However, in the NICU, most studies have focused on Unplanned Extubation (UE), which refers to the accidental removal of a tracheal cannula. The reported rates of UE in NICUs range from 0.72 to 5.36 extubations per 100 ventilated days [6]. Various risk factors have been identified for UE, including infant agitation, tube manipulation, loosening of fixation tape or wet tape and a high nurse-to-patient ratio [7]. However, little attention has been given to the unplanned removal of orogastric tubes, leading to repeated insertions. In previous study showed enteral feeding tubes are prone to rapid development of microbial biofilms, which may serve as reservoirs for pathogens. Therefore, frequent reinsertion of orogastric tubes may increase the risk of infection or contribute to the development of Necrotizing Enterocolitis (NEC) in infants [8,9].
Unplanned Removal of Orogastric Tubes (UROGT) involves the unintentional displacement of the feeding tube, potentially necessitating repeated insertions. This not only extends hospital stays but also amplifies infection risk, radiation exposure and the likelihood of oesophageal or gastric injury [10]. Neonates are particularly susceptible to UROGT, with one study reporting a 31.2% incidence of orogastric tube displacement in preterm new-borns, compared to a 12% incidence for nasogastric tubes [11]. Unfortunately, there are currently no investigation on the incidence of UROGT in China's NICU and risk factors associated with it are also absent.
To address these gaps, we conducted an observational study within a single Chinese NICU to systematically assess the incidence of UROGT and explore its associated risk factors.
Study design
This study was an observational study conducted for a period of five months, from October 2022 to February 2023, in a 120-bed capacity NICU of China. The institutional review board of the hospital approved the research and eligible patients with orogastric tubes were recruited and observed by nurses. Of the 122 patients initially enrolled, 11 were excluded, as they either underwent tube placement during surgery, were transferred to another hospital due to congestive heart diseases or died in the unit.
The inclusion criteria were infants with doctor-determined indications for orogastric tube insertion, those whose feeding tube was placed for more than 24 hours and those with no gastrointestinal system malformations. The exclusion criteria were infants with a nasogastric tube or those with a tube that was only used for single gastric lavage or medication administration.
Sample size
We conducted case-control study design to investigate the risk factors associated with UROGT. The case group included participants who experienced at least one UROGTs event and the control group comprised those who had never experienced such an event. The sample size was computed using the PASS 2021 software. Based on our pilot study, we estimated the UROGTs rate to be 30% and assuming the lowest odds ratio to be 8, the significance to be 0.05 and the power to be 0.8, we calculated that a sample size of 100 new-borns was required for the study (Figure 1).
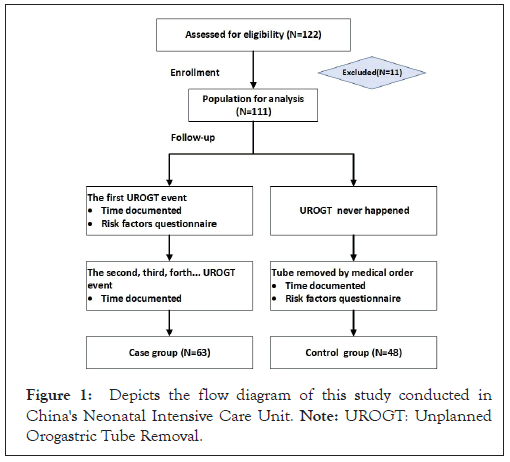
Figure 1: Depicts the flow diagram of this study conducted in China's Neonatal Intensive Care Unit. Note: UROGT: Unplanned Orogastric Tube Removal.
Tube insertion
Tube insertion was performed by registered nurses in the NICU who had at least one year of clinical NICU experience. Prior to the study, they received training on the insertion procedure and the measurement method by the lead researchers to minimize potential biases and complications. The insertion depth was estimated using a weight-based equation (length=3 × weight (kg) +12 cm) and was confirmed by radiological examination.
A pediatric disposable stomach tube kit (VERACON, Suzhou, Jiangsu, China) consisting of a silicone lumen tube with a diameter of F 6.0 or F 8.0, a pack of sterile liquid paraffin and sterile gloves were used for the study. Routine sedatives or analgesics were not administered to new-borns requiring an orogastric tube in our NICU [8-10].
Tube maintenance
The orogastric tube was securely fixed in place using water-resistant tape, which was attached to one cheek, crossed over the tube and affixed to the other cheek. The tube was extended slightly from the infant's mouth and maintenance care details were consistently recorded in the electronic nursing record. Nursing staff in our NICU followed 8-hour shifts, ensuring continuous care across all day, evening and night periods. Consequently, the secured tube was checked every 8 hours. If the tape showed signs of loosening or significant wetness, the tube was promptly replaced, adhering to the manufacturer's recommendation of changing tubes weekly [11].
Risk factors investigation
In this study, a questionnaire tool consisting of five items was used, based on a similar study on unplanned endotracheal extubation in new-borns and a pilot study. The tool included the time of every unplanned tube removal as the dependent variable and the new-borns basic information (including sex, gestational age, birthday and birth weight), patient-related factors (position, ventilation support, agitation score and medical activities before removal), feeding-related factors (enteral feeding or oral feeding) and nursing-related factors (number of patients assigned and length of NICU careers) as the independent variables.
To objectively assess the nurse’s perception of each baby’s level of agitation, a 6-point likert scale was designed, with scores ranging from 0 (none) to 5 (most affected) [12]. The content validity of the tool was assessed by four NICU experts, including two chief nurses with at least five years of work experience, one neonatologist and one registered nurse, who evaluated the content obtained from the pilot study. The content was validated in a group of five pre-term and five term newborns. The questionnaire took approximately 10 minutes for a nurse to complete.
Data collection
After enrolment, a registered nurse collected the basic information from medical records, including gestational age, birth weight and days of life. Subsequently, the assigned nurses completed the questionnaire after the first unplanned removal of the orogastric tube, providing information on the time of occurrence, tube fixation and length of NICU career related to the event. In cases where UROGT recurred, the nurse just recorded the time of recurrence. If UROGT did not occur during placement and the infant's condition improved, the doctor decided on the planned removal of the orogastric tube and scores for related factor items in the questionnaire were collected by registered nurses before the removal.
Statistical analysis
AIn the statistical analysis, the proportion of UROGT was calculated by dividing the number of patients who experienced the event by the total number of eligible patients and then multiplying the result by 100. The incidence of UROGT was determined per 100 orogastric tube days, by dividing the number of UROGTs events by the number of orogastric tube days and multiplying the result by 100. Kaplan-Meier survival curves were generated to analyse the survival rate. All risk factors were initially analysed in the univariate model and the significant risk factors (P<0.10) were selected for the multivariable logistic regression model to obtain independent risk factors. Data processing was performed using Statistical Package for the Social Sciences (SPSS) statistics 20.0 software International Business Machines Corporation (IBM Corp). Categorical data were described using percentages and proportions. Continuous variables were described as mean ± standard deviation if they followed a normal distribution or median Inter Quartile Range (IQR) if they did not.
Participant characteristics
This study included a total of 111 new-borns who were inserted with an orogastric tube. Among of them, 63.1% (70/111) was male, the mean gestational ages were 35.3 ± 3.5 weeks and the birth weights were 2382.7 ± 740.1 g.
Incidence of UROGT
Over the course of the five-month investigation period, a substantial number of infants experienced unplanned removal events. Specifically, 63(56.8%) infants encountered a single unplanned removal, 15(13.5%) infants had two such incidents and an additional 8(7.2%) infants endured three occurrences. In total, there were 132 instances of UROGT events during this period. The overall proportion of UROGT for the entire study duration was 56.8% (63/111). Furthermore, the cumulative duration of orogastric tube placement amounted to 1718.1 days, resulting in an incidence rate of 7.2 per 100 tube days (132/1718.1).
Kaplan-Meier curve
During the study period, we defined the occurrence of the first UROGT as the 'event', while the duration of tube placement without UROGT served as the 'follow-up time’. The cumulative survival rate exhibited a pattern of decline over time, with rates of 61.6% in the first week, 42.5% in the second week, 35.3% in the third week, 27.7% in the fourth week, 27.7% in the fifth week, 20.8% in the sixth week following the initial tube insertion. Illustrates the survival rate for the orogastric tube group (Figure 2).
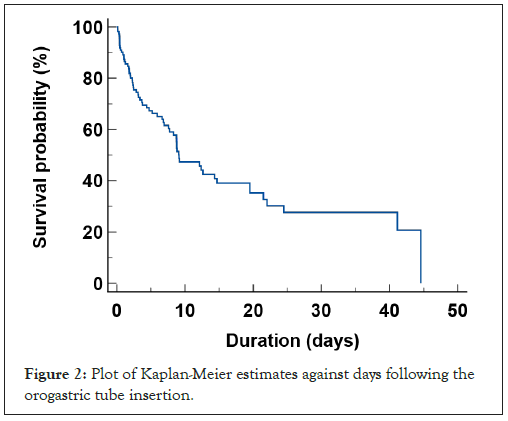
Figure 2: Plot of Kaplan-Meier estimates against days following the orogastric tube insertion.
Baseline comparison
The 63 infants experienced events of UROGT were allocated to the case group and the remaining 48 were matched as the control group. The mean gestational ages were 35.0 ± 3.6 weeks and 35.6 ± 3.5 weeks and the birth weights were 2312.2 ± 756.2 g and 2475.2 ± 715.8 g in the case and control groups, respectively. The majority of both groups (92.1% in the case group and 95.8% in the control group) had an initial tube size of 6F. The mean insertion length was 18.6 ± 2.1 cm in the case group and 18.7 ± 2.1 cm in the control group. None of these factors showed statistically significant differences between the two groups (P>0.05), as detailed in (Table 1). For categorical variables, Chi-Square (χ²) was used to test the differences between the two groups and a t test was used for continuous variables.
| Variables | Case | Control | at/χ² | P-value |
|---|---|---|---|---|
| (Sex) male | 41(65.1) | 29(60.4) | 0.25 | 0.614 |
| Female | 22(34.9) | 19(39.6) | - | - |
| Gestational age (weeks) | 35.0 ± 3.6 | 35.6 ± 3.5 | 0.81 | 0.419 |
| Birth weight (g) | 2312.2 ± 756.2 | 2475.2 ± 715.8 | 1.15 | 0.252 |
| (Orogastric tube size) 6F | 58(92.1) | 46(95.8) | 0.66 | 0.418 |
| 8F | 5(7.9) | 2(4.2) | - | - |
| Insertion length (cm) | 18.6 ± 2.1 | 18.7 ± 2.1 | 0.19 | 0.849 |
Note: χ²: Chi-Square.
Table 1: Comparison of baseline characteristics between the two groups.
Univariate risk factor analysis
F control group (89.6% vs. 61.9%, P=0.017). Nasal Intermittent Positive Pressure Ventilation (NIPPV) was the predominant ventilator mode in the case group (22.2%), while in the control group, NIPPV and High Flow (HF) modes were equally utilized (4.2% each). Furthermore, the average agitation score prior to tube dislodgment in the case group was notably higher at 2.6 ± 1.8, in contrast to the control group's score of 0.2 ± 0.5 (P<0.001). Regarding enteral feeding practices, a significantly larger proportion of control group participants (95.2%) had received oral feeding, compared to the case group where this figure stood at 56.0% (P<0.001).
In the context of fixation factors, infants in the case group were more likely to experience issues such as loose fixation, tape starting to lift and tape getting wet (all P<0.001). Additionally, the mean length of NICU nursing experience was notably higher in the case group at 5.8 ± 4.4 years compared to the control group's 3.1 ± 2.4 years (P<0.001). This information is provided in further detail in (Table 2).
| Category | Variables | Case (N=63) | Control (N=48) | t/χ² | P-value |
|---|---|---|---|---|---|
| Basic factors | DOL when insertional | 1.65(0.55-6.47) | 0.86 (0.64-7.47) | 0.363 | 0.717 |
| Weight when insertion | 2651.8 ± 563.8 | 2474.8 ± 685.7 | 1.45 | 0.149 | |
| Ventilation | Ventilation support | - | - | 12.01 | 0.017 |
| CMV | 5(8) | 1(2.1) | - | - | |
| NIPPV or CPAP | 14(22.2) | 2(4.2) | - | - | |
| HF | 5(7.9) | 2(4.2) | - | - | |
| None | 39(61.9) | 43(89.6) | - | - | |
| Agitation | Agitation scores | 2.6 ± 1.8 | 0.2 ± 0.5 | 10.3 | <0.001 |
| Medical activity before removal | - | - | 1.17 | 0.28 | |
| Yes | 6(9.5) | 2(4.2) | - | - | |
| None | 57(90.5) | 46(95.8) | - | - | |
| Feeding | Enteral feeding | - | - | 1.27 | 0.26 |
| Yes | 50(79.4) | 42(87.5) | - | - | |
| None | 13(20.6) | 6(12.5) | - | - | |
| Oral feeding | - | - | 18.23 | <0.001 | |
| Yes | 28(56.0) | 40(95.2) | - | - | |
| None | 22(44.0) | 2(4.8) | - | - | |
| Fixation | Loose fixation | - | - | 22.41 | <0.001 |
| Yes | 28(44.4) | 2(4.2) | - | - | |
| None | 35(55.6) | 46(95.8) | - | - | |
| Tape starting to lift | - | - | 10.42 | 0.001 | |
| Yes | 15(23.8) | 1(2.1) | - | - | |
| None | 48(76.2) | 47(97.9) | - | - | |
| The proportion of tape getting wet | - | - | 22.16 | <0.001 | |
| ≥50% | 12(19.0) | 0 | - | - | |
| <50% | 23(36.5) | 6(12.5) | - | - | |
| None | 28(44.4) | 42(87.5) | - | - | |
| Work load | Number of patients assigned | 9.1 ± 2.3 | 8.5 ± 2.2 | 1.34 | 0.183 |
| Number of critical patients assigned | 7.4 ± 2.8 | 7.0 ± 2.1 | 0.85 | 0.395 | |
| Length of NICU nursing career (years) | 5.8 ± 4.4 | 3.1 ± 2.4 | 3.82 | <0.001 |
Note: CMV: Controlled Mechanical Ventilation; NIPPV: Nasal Intermittent Positive Pressure Ventilation; CRAP: Continuous Positive Airway Pressure; HF: High Flow; DOL: Days of Life; NICU: Neonatal Intensive Care Unit; χ²: Chi-Square.
Table 2: Univariate factors for unplanned removal of the orogastric tube.
Days of Life (DOL) is the difference between the time of initial orogastric tube insertion and the date of birth and is described as the median and Inter Quartile Range (IQR).
Agitation scores ranged from 0 (none) to 5 (most agitation), which was assessed by the assigned nurse.
Medical activity including blood draw or puncture, bathing, transportation, weighing or radiology study.
Multivariable risk factor analysis
In the multivariable logistic regression analysis, various factors, including ventilation support, agitation scores, oral feeding, loose fixation of the tube, tape starting to lift, proportion of the tape wet and length of NICU nursing career, were considered.
The analysis revealed several significant associations with the incidence of unplanned removal of the orogastric tube. Notably, agitation scores exhibited a substantial impact, with a one-point increase corresponding to a staggering 17.82 times higher risk of UROGTs (OR=17.82, P=0.001, 95%, Class Interval (CI=3.01-105.38). In contrast, new-borns who had initiated oral feeding during tube placement experienced a significantly reduced risk, approximately 0.02 times lower (OR= 0.02, P=0.007, 95% CI=0.01-0.35). Additionally, neonates with loose fixation of the tube faced a considerably elevated risk, with an odds ratio of 26.48 compared to those with secure fixation (OR=22.75, P=0.027, 95% CI=1.46-482.12). Wetting of the fixation tape also emerged as a predictive factor for UROGTs (OR=12.6, P=0.021, 95% CI=1.47-108.45), as summarized in (Table 3).
| Variables | B | Standard error | Wald χ² | P-value | OR | 95% CI for OR |
|---|---|---|---|---|---|---|
| Ventilation support (Yes vs. None) | -1 | 1.34 | 0.55 | 0.458 | 0.37 | 0.03-5.16 |
| Agitation scores (continuous variable) | 2.88 | 0.91 | 10.09 | 0.001 | 17.82 | 3.01-105.38 |
| Oral feeding (Yes vs. None) | -3.81 | 1.4 | 7.37 | 0.007 | 0.02 | 0.01-0.35 |
| Fixation tape loosening (Yes vs. None) | 3.28 | 1.48 | 4.9 | 0.027 | 26.48 | 1.46-482.12 |
| Tape starting to lift (Yes vs. None) | 1.4 | 1.46 | 0.92 | 0.337 | 4.04 | 0.23-70.01 |
| Tape getting wet (Yes vs. None) | 2.53 | 1.1 | 5.33 | 0.021 | 12.6 | 1.47-108.45 |
| Length of NICU nursing career (years) | 0.28 | 0.16 | 3.14 | 0.066 | 1.33 | 0.97-1.84 |
Note: CI: Confidence Interval; OR: Odds Ratio; NICU: Neonatal Intensive Care Unit; χ²: Chi-Square.
Table 3: Presents the results of logistic regression analysis for the risk factors associated with unplanned removal of orogastric tubes.
In this single-centre study conducted in China, we observed an occurrence rate of 56.8% for UROGTs in the NICU, with an incidence of 7.2 per 100 tube days. Our findings highlight the significant impact of specific factors, including higher agitation scores in new-borns, absence of oral feeding and issues related to the loosening and wetting of fixation tape, on the incidence of unplanned tube removal.
Tubes and catheters are the main appliances used in the NICU, providing daily health treatment for the administration of medicines and milk to critical new-borns [13]. Patients who experienced unplanned removal of medical devices had more medical complications, such as bleeding, pulmonary, aspiration and nosocomial infection [14]. According to a study involving adult ICU patients, nasogastric tubes, endotracheal tubes and central catheters are most commonly subjected to unplanned removal. Reducing the incidence of and mitigating the risk factors for these events have been a major topic in the NICU.
Previous studies have mainly focused on strategies to reduce the incidence of UE of the Endo Tracheal Tube (ETT), which may cause common adverse effects in patients, including lung collapse, cardiovascular instability, trauma to the upper respiratory tract, ventilator-associated pneumonia and so on [15]. A study including 182 neonates requiring mechanical ventilation in Australia showed that the UE rate in the neonatal population was 4.75 per 100 days of ventilation [16]. Similarly, a recent study from South Korea showed that 32.1% of new-borns in the NICU had experienced UE, with an incidence of 6.56 per 100 ventilation days. Although orogastric tubes are less important than ETT, orogastric tubes are still valuable devices that can provide enteral nutrition and allow gastric decompression, especially for preterm babies [17]. In contrast, there are few studies reporting the incidence of unplanned removal in our country. In this study, the reported incidence of UROGT was 7.2 per 100 tube days, which was higher than that of UE in other studies. Therefore, the medical teams in our NICU should begin to recognize UROGT as a significant problem and strive to reduce this rate [18]. Our results revealed an incidence of UROGT, which can act as a baseline to understand the current situation. This will strongly support initiatives of quality improvement aiming at reducing the rate in the NICU [19].
Another essential part of the quality improvement study is to determine the type of intervention needed based on the risk factors. Factors associated with UE in the NICU have been investigated in the published articles. Patient agitation, poor fixation of the ETT, frequent suction, nurses working night shifts and/or overtime and a higher patient-to-nurse ratio were related to an increased number of UE events in the NICU [20]. Recent literature provides various strategies to help reduce UE rates. Strategies to proactively reduce agitation during ETT placement have been proven to be effective in decreasing the incidence of UEs. However, the methodology for reducing the incidence of UEs is not directly applicable for the orogastric tube.
In this study, we found four risk factors for unplanned removal of tubes, including higher agitation scores, absence of oral feeding and the loosening and wetting of fixation tape. Among these four risk factors, our study found that the odds ratios of fixation factors, including tape loosening and wetness, were higher, indicating their pertinence as key risk factors for UROGT [21]. Therefore, improving fixation techniques and ensuring frequent observation of fixed tubes may reduce the incidence of unplanned tube removal. Such findings are consistent with those found in studies on UE, which showed that fixation tape method was the main risk factor for UE in new-borns. Moreover, a quality improvement study also supported our results in that the main solution for UE was that the tape securing the tube became loose [22]. For future projects aiming to reduce the incidence of UROGT, we recommend that loose tape be promptly reinforced and that any tape found to be “too wet” be promptly replaced.
In addition, we found that if the baby was very active, they could unintentionally pull out their own feeding tube, resulting in UROGT. Our study also revealed that infant agitation was the common factor associated with UE in the NICU [23,24]. However, these findings do not indicate that sedative-analgesic medications should be administered to calm agitated babies during orogastric tube placement. Jung’s study on the risk factors for UE in Korea showed that the administration of sedative-analgesic medications did not prevent UE in new-borns. From the author’s perspective, it is important to design an easily applicable tool to accurately assess infant agitation. Nonpharmacological strategies for minor agitation include non-nutritive sucking, breastfeeding and skin-to-skin contact to reduce the incidence of accidental dislodgment of various tubes in the NICU [25]. Recently, an Infant Driven Feeding (IDF) approach was introduced for oral feeding. Based on this strategy, feeding should always be initiated before crying occurs, which may dramatically reduce agitation [26].
In our unit, when an infant was deemed physiologically stable, we began oral feeding at 32 to 34 weeks gestational age. Oral feeding was previously delayed for several days or weeks but most can start oral feeding much sooner. In this study, neonates who started oral feeding sooner were at lower risk for UROGT. Therefore, our team recommends that infants, especially preterm babies, begin oral feeding as early as possible. Not only is it an effective way to decrease the risk of UROGTs, but it can also help shorten the time to full oral feedings and the length of hospital stay [26].
A few limitations should be mentioned in regard to this study. First, this study was a single-centre study conducted in one children’s hospital; therefore, selection bias is possible. Second, due to the lack of recent literature on UROGTs, we selected risk factors for unplanned extubation of endotracheal tubes that were previously studied in published articles. Therefore, some related factors may not be identified. Third, this study only included new-borns with orogastric tubes. Since the guidelines for tube insertion and maintenance may differ from those for nasogastric tubes, our results may not be applicable to nasogastric tubes.
The proportion of UROGT during the study period was 56.8%, with an incidence of 7.2 per 100 tube days in our NICU. New-borns with the following conditions were more likely to be at risk of UROGT: Higher agitation scores, absence of oral feeding and fixation tape loosening and wetness. These results would be valuable for reducing the incidence of UROGT in the subsequent quality improvement project. By considering the above results this has provided our neonatal intensive care unit with a benchmark for improvement. It has also created staff awareness of the risk of UROGT and promoted staff engagement to reduce UROGT.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Chen J, Fang X, Huang C, Dai Y (2023) The Incidence of Unplanned Orogastric Tube Removal (UROGT) and Associated Risk Factors in a Chinese NICU: A Study Before Quality Improvement Initiative. Clin Pediatr. 08:252.
Received: 30-Oct-2023, Manuscript No. CPOA-23-28359; Editor assigned: 02-Nov-2023, Pre QC No. CPOA-23-28359 (PQ); Reviewed: 16-Nov-2023, QC No. CPOA-23-28359; Revised: 23-Nov-2023, Manuscript No. CPOA-23-28359 (R); Published: 30-Nov-2023 , DOI: 10.35248/2572-0775.23.08.252
Copyright: © 2023 Chen J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.