
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research Article - (2023)Volume 13, Issue 1
Objective: Despite improvements in maxillary and mandibulary osteotomy, complications still result around 20%. Post and intra-operative standard therapies, based on the use of betametasone and tranexamic acid, could help to minimize the onset of side-effects. The aim of our study was to compare the role of a supplementary bolus of methylprednisolone rather than the standard therapy in the onset of postoperative symptoms.
Methods: We enrolled 10 patients, affected by Class II and III Dentoskeletal, submitted to our institution for maxillomandibular repositioning osteotomy between October 2020 and April 2021. Patients were divided in 2 groups as following; 5 patients (Group A) received standard therapy consisting in the administration of 4 mg of Betamethasone, intraoperatively, and 1 gm of tranexamic acid in two administrations. The remaining five patients (Group B) received a supplementary bolus of 20 mg methylprednisolone before the end of the surgery.
All patients received, in the postoperative period, 4 mg of Betamethasone every 12 hours, for 3 days. Postoperative outcomes were evaluated with questionnaire evaluating speaking discomfort, pain when swallowing, feeding discomfort, drinking discomfort, swelling and ache. Each parameter was associated to a numeric rating scale ranging from 0 to 5.
Results: We observed that patients treated with a supplementary bolus of methylprednisolone (Group B) had a statistically significative reduction of all post-operative symptoms as compared with patients of Group A.
Conclusion: Our study highlighted that the additional bolus of methylprednisolone improved all of the 6 parameters investigated by the questionnaire submitted to our patients, resulting in a faster recovery and improvement of the patient’s compliance to surgery. Further studies with larger population are needed to confirm our preliminary results.
Arrhythmia-induced cardiomyopathy; Tachymyopathy; Diagnostic algorithm; Atrial fibrillation
Orthognathic surgery is the branch of surgery dealing with the repositioning of skeletal bases, in order to improve both morpho-functional and aesthetic function [1]. It is usually indicated in patients with dental-skeletal anomalies, syndromic deformities involving the craniomaxillofacial area and disorders affecting temporo-mandibular joint. Therefore, the goal of this kind of surgery is the normalization of the occlusal relationship, with a correct harmonization of the soft tissues [2].
Several studies have shown how skeletal malocclusion could lead to the development of different symptoms, as decreased bite power, temporo-mandibular joint disorders, alteration in mandibular kinetics. Early intervention, with osteotomy for the repositioning of the skeletal bases, has shown a dramatic decline in the onset of dysfunctions in the temporomandibular joint, as well as an improvement in associated symptoms [3]. Many studies have also shown how patients undergoing maxillo-mandibular repositioning surgery report a crucial psycho-physical improvement, with a significant impact on self-confidence [4].
Although over the years surgical time has greatly decreased, as a result of the relevant improvement and predictability of the surgical technique, there is great heterogeneity, between different centers within the same type of surgery in terms of postoperative course [5]. Furthermore, postoperative conditions of patients who underwent orthognathic surgery still represent an open issue. Indeed, edema and hematoma, representing the most common postoperative manifestations, affect patient's immediate perception [6]. The aim of our study was to evaluate the adding of a bolus of methylprednisolone compared to standard therapy in minimizing the side effects.
Patients
We enrolled 10 patients, affected by Class II and III Dentoskeletal, submitted to our institution for maxillomandibular repositioning osteotomy between October 2020 and April 2021. Patients were affected by discrepancy in the maxillomandibular occlusion, complaining of painful symptoms during chewing, and temporo-mandibular joint disorders.
Surgical procedures
Patients underwent pre-surgical orthodontic treatment in order to make dental arches congruent, before the repositioning surgery. Surgery was conducted under general anesthesia, with nasal intubation. Patients underwent to maxillo-mandibular repositioning treatment Le Fort I osteotomy (LFI) and Bilateral Sagittal Split Osteotomy of the mandible (BSSO). Two out of 10 patients (25%) also underwent chin repositioning surgery.
Concomitant medication
Patients were divided in 2 groups as following: 5 patients received standard therapy represented by the administration, intraoperative, of 4 mg of Betamethasone and 1 gm of tranexamic acid, both of them in two administrations (Group A). The remaining five patients received a supplementary bolus of 20 mg methylprednisolone before the end of the surgery (Group B). All patients received, in the postoperative period, 4 mg of Betamethasone every 12 hours, for 3 days.
Questionnaire
The postoperative outcomes were evaluated according to the following questionnaire submitted to patients 24 hours after surgery. The parameters considered were the following; speaking discomfort, pain when swallowing, feeding discomfort, drinking discomfort, swelling, ache. Each parameter was associated to a numeric rating scale where 0 represents “no perceived noise”, while 5 corresponds to “Disorder perceived as disabling”.
Statistical analysis
Mann Whitney test for analysis of non-parametric values was used. Results were considered statistically significant if p value was <0.05. The present study follows the guidelines according to the Declaration of Helsinki on medical protocols and ethics. The treatment plan respects the Declaration of Helsinki and the patient signed a written consent aware of the treatment goals and of the possible consequences and complications. Due to the retrospective nature of this study, it was granted an exemption in writing by our hospital.
We enrolled 10 patients affected by Class II and III Dentoskeletal; median age was 23 years and male/female ratio was 1. Three out of 10 patients (30%) were smokers and no comorbidity has been reported. Five patients (defined as group A) (50%) received intraoperatively, 4 mg of Betamethasone and 1 gm of tranexamic acid in two administrations, followed by 4 mg of Betamethasone every 12 hours, for 3 days. Five patients (defined as group B) (50%) received a supplementary bolus of 20 mg methylprednisolone before the end of the surgery. The result of the questionnaire was summarized in Table 1 and 2 (Group A and Group B, respectively).
| Group A | Speaking Discomfort | Pain swallowing | Feeding Discomfort | Drinking Discomfort | Swelling | Ache |
|---|---|---|---|---|---|---|
| Pt 1 | 4 | 2 | 4 | 3 | 5 | 4 |
| Pt 2 | 3 | 3 | 4 | 3 | 4 | 4 |
| Pt 3 | 4 | 3 | 4 | 3 | 5 | 3 |
| Pt 4 | 5 | 3 | 4 | 3 | 5 | 5 |
| Pt 5 | 3 | 2 | 3 | 3 | 4 | 4 |
Table 1: Result of questionnaire submitted to group treated with Betamethasone and Tranexamic acid.
| Group B | Speaking Discomfort | Pain swallowing | Feeding Discomfort | Drinking Discomfort | Swelling | Ache |
|---|---|---|---|---|---|---|
| Pt 1 | 2 | 1 | 2 | 1 | 2 | 1 |
| Pt 2 | 1 | 1 | 1 | 1 | 1 | 1 |
| Pt 3 | 2 | 2 | 2 | 1 | 2 | 1 |
| Pt 4 | 3 | 1 | 2 | 1 | 1 | 2 |
| Pt 5 | 1 | 1 | 1 | 1 | 1 | 1 |
Table 2: Result of questionnaire submitted to group treated with Betamethasone and Tranexamic acid, plus a Methylprednisolone Bolus before the end of surgery.
In particular, the average score of each parameter was the following:
• Speaking Discomfort: 3.8 (Group A); 1.8 (Group B)
• Pain Swallowing: 2.6 (Group A); 1.2 (Group B)
• Feeding Discomfort: 3.8 (Group A); 1.6 (Group B)
• Drinking Discomfort: 3 (Group A); 1 (Group B)
• Swelling: 4.6 (Group A); 1.4 (Group B)
• Ache: 4 (Group A); 1.8 (Group B)
We observed that patients treated with a supplementary bolus of methylprednisolone (Group B) had a statistically significative reduction of all post-operative symptoms as compared with patients of Group A (p<0.05, **p<0.01 Figure 1).
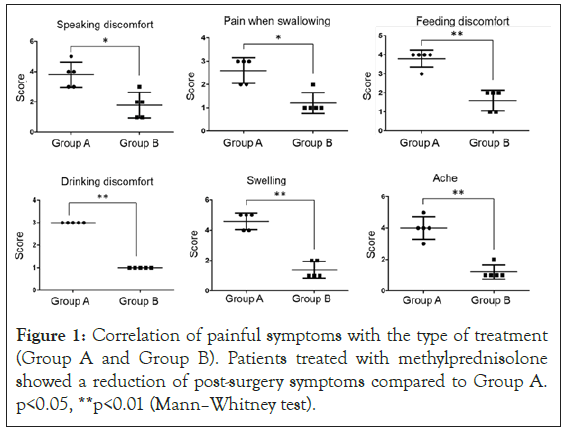
Figure 1: Correlation of painful symptoms with the type of treatment (Group A and Group B). Patients treated with methylprednisolone showed a reduction of post-surgery symptoms compared to Group A. p<0.05, **p<0.01 (Mann–Whitney test).
The main issue related to the bimaxillary surgery is represented by the significant postoperative edema that negatively affects patient's surgery success perception with a consequent lengthening of the functional recovery. The aim of our study was to evaluate the role of additional bolus of Methylprednisolone to the standard therapy in patients treated with Le fort I and BSSO. As previously described, standard treatment consisted in the administration, intraoperatively, of 4 mg of Betamethasone and 1 gm of tranexamic acid in two administrations following by 4 mg of Betamethasone every 12 hours, for 3 days.
Tranexamic acid has been used for years to manage postoperative hematoma, not only in maxillofacial surgery, but also in orthopedic, neurosurgical and cardiac surgery [6,7]. It is an antifibrinolytic that competitively inhibits the activation of plasminogen to plasmin; the latter is an enzyme that degrades fibrin plug, fibrinogen and other plasma proteins, including procoagulant factor V and VIII [8]. Rummasak, et al. [9] showed that, although blood loss is usually within the limits not requiring any transfusion, it can occasionally be massive, with losses ranging from 200 mL to 3400 mL. Several studies showed intraoperative and postoperative blood loss reduction in patients treated with tranexamic acid, both in elective and emergency surgery, with no increase in mortality related to thrombotic cardiovascular events [10]. According to Apipan, et al. [11], 10 mg/kg of body weight is the dose associated with the reduction of intraoperative and postoperative bleeding. According to our results, the administration of tranexamic acid led to a reduction of the entity of the 6 parameters investigated by the questionnaire. As regarding postoperative edema, glucocorticoids have always played a crucial role in post-operative management of patients treated with repositioning of the skeletal bases. Also known as corticosteroids, they have the greatest antiinflammatory power of all steroids, being able to reduce edema, pain, trismus, nausea and vomiting, and promoting nerve healing. Their anti-edema, pain relieving, antiinflammatory effect has been exploited for several years in post-operative management, although there are still no literature agreement as concerns their function related to wound healing, suppression of the adrenergic system and osteonecrosis. They also work reducing endothelial permeability, decreasing the amount of fluids, proteins and macrophages [12].
Their positive effect in oral surgery in reducing post-operative discomfort and sequelae, especially in the third molar surgery, is well known. It is almost certain that swelling and, to some extent, trismus could be significantly reduced by the use of corticosteroids [13-28].
The positive effects of steroids in maxillofacial surgery were emphasized in many studies, in particular in reducing facial edema after Le Fort I osteotomy and BSSO [29]. Young-Kyun Kim, et al. showed the positive effect of these drugs in nerve injury healing, highlighting that the use of steroids during or after surgery can effectively prevent temporary injuries by reducing pressure created by edema [30]. Main steroids used in postoperative therapy are represented by Betamethasone, Methylprednisolone, Dexamethasone, Hydrocortisone and Prednisolone [31]. Methylprednisolone is five times more potent in its anti-inflammatory properties compared to hydrocortisone (cortisol), with minimal mineralocorticoid activities [12].
The onset of action of intravenous methylprednisolone succinate is within 1 hour, with a duration of 1 to 5 weeks. It has an oral bioavailability of 88% approximately, and the half-life elimination is of 0.25 hours, with an oral halflife of 2-5 hours. It has hepatic metabolism and undergoes urinary excretion [32,33]. There are only few studies investigating the role of methylprednisolone in reducing post-operative symptoms, and these are especially related to oral surgery. In particular in impacted three molars, authors agreed on the positive role of Methylprednisolone in reducing postoperative edema, pain and trismus [34,35].
As concerns orthognathic surgery there are only 3 studies focusing specifically on the role of Methylprednisolone. The Authors were agreed in acknowledging the role of these drug in reducing edema and inflammation, especially during the first postoperative hours [36,37]. Indeed, our study is in line with previous reports confirming the effectiveness of standard therapy, also in orthognathic surgery. According to our knowledge, this is the first study that investigates the role of an additional bolus of methylprednisolone to the standard care. Our results showed the statistically significant effect of the methylprednisolone in the reduction of the all 6 parameters investigated especially swelling and ache. Further studies with larger population are needed to confirm our preliminary results.
Our study highlighted that the additional bolus of methylprednisolone to the standard therapy improved all the 6 parameters investigated by the questionnaire submitted to our patients, resulting in a faster recovery and improvement of the patient’s compliance to surgery.
All authors affirm that their study obtained the required ethical clearance and respected all ethical considerations and that, moreover, if the study involved human subjects, signed informed consent was obtained and privacy respected; all the related documents are attached to this submission.
All the patients firmed an informed consent.
All authors affirm that they have played a significant role in the conception, design, data analysis and interpretation, and writing of the manuscript, as stated by the International Committee of Medical Journal Editors (ICMJE): “Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND Drafting the work or revising it critically for important intellectual content; AND Final approval of the version to be published; AND Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.”
We will allow the Editors to make changes to the manuscript, if accepted for publication, during the editing process, and all authors listed in this manuscript acknowledge this submission and sign bellow.
All authors contributed to the study conception and design. Material preparation was performed by Dr Amodeo that discuss with Dr Minieri to better understand the feasibility and the time to administrate the corticosteroids; data collection was performed by Dr Cerbelli; the analysis were performed by Dr Pisano; all the paper was validated by Prof Scopelliti, chief of maxillofacial surgery unit. The first draft of the manuscript was written by Dr Amodeo and presented to other authors to include their suggestions. All authors read and approved the final manuscript.”
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Giulia A, Edoardo C, Annalinda P, Luciana M, Domenico D (2023) The Influence of Bolus of Methylprednisolone on Post-Orthognathic Surgery Symptoms: A Controlled Clinical Trial. J Clin Trials. 13:518.
Received: 06-Mar-2023, Manuscript No. JCTR-23-22051; Editor assigned: 08-Mar-2023, Pre QC No. JCTR-23-22051 (PQ); Reviewed: 22-Mar-2023, QC No. JCTR-23-22051; Revised: 29-Mar-2023, Manuscript No. JCTR-23-22051 (R); Published: 05-Apr-2023 , DOI: 10.35248/2167-0870.23.13.522
Copyright: © 2023 Giulia A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.