
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Short Communication - (2021)Volume 12, Issue 6
The use of deep Monitored Anesthesia Care (MAC) has increased significantly with the advent of propofol and the expansion of procedures outside hospital-based operating rooms [1]. During deep MAC, the goal is to provide sedation while preserving spontaneous ventilation and avoiding apnea [2,3]. Maintaining a patent airway is essential for mitigating adverse outcomes from inadequate ventilation and oxygenationrespiratory events being the most prevalent source of reported MAC anesthesia closed claims [4,5].
While heightened vigilance, preoxygenation, and improved monitoring techniques (e.g. capnography and bispectral index) have contributed to MAC safety [6,7]. The availability of airway devices optimized for deep MAC has lagged [2]. Oropharyngeal airways (OPAs) often cannot reach the redundant distal pharyngeal tissue within the upper airway near the epiglottis to stent it open [8]. A recent survey of anesthesia professionals indicated that 88% use jaw thrust and chin lift maneuvers in conjunction with OPAs to maintain patency [8]. These maneuvers can result in post-operative jaw and chin pain for patients, as well as hand pain for clinicians [8,9]. Additionally, this occupies the providers’ hands, limiting their ability to address other tasks. OPA-related adverse effects include coughing, gagging, swelling, damage to teeth intraoral structures, and postoperative sore throat [10-13]. Nasopharyngeal airways may cause epistaxis or increased cardiovascular response, can be difficult to place in patients with nasal abnormalities, and should be avoided in anticoagulated patients [14,15].
Because of the paucity of airways optimized for MAC, clinical workarounds-including use of nasal airways in the oral cavityhave emerged. Smaller-diameter, flexible nasal airways inserted through the mouth are easier to position than hard plastic OPAs, decrease the need for jaw thrust and chin lift maneuvers, and may also reduce postoperative sore throat [10]. In a survey of 293 U.S. anesthesia professionals, more than half (52.8%) have used a nasal airway orally [10]. Despite these perceived benefits, nasal airways are not designed for this purpose and can pose patient safety risks including dislodgement into the airway and airway occlusion, which poses patient safety and liability issues [10].
To reduce this off-label practice and provide a much-needed solution, a newer hybrid airway device combines the flexibility and longer tubing length of the nasal airway with the structural integrity of existing rigid oral devices. The additional tubing length stents open the pharyngeal tissue that current airways are unable to reach. Smaller diameter tubing also eases insertion and mitigates potential oral injury associated with hard airways. One such hybrid airway includes additional patient safety components such as an integrated cushioned bite block to aid in placement and decrease dental trauma, as well as an optional connector that connects to an anesthesia circuit or manual resuscitator. As recent nasal cannulas and masks have been developed to improve oxygenation under deep MAC, the McMurray Enhanced Airway or MEA opens the airway to help improve ventilation (Figure 1) [16].
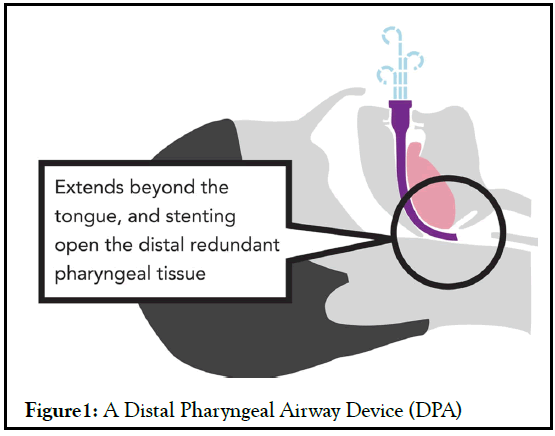
Figure 1: A Distal Pharyngeal Airway Device (DPA)
As the use of deep MAC grows, anesthesia providers need safe, intuitive, effective, and easy-to-place tools designed to reduce apnea and improve oxygenation and ventilation, resulting in improved patient outcomes and patient safety.
Citation: McMurray R (2021) The Need for Improved Airway Management Techniques in Deep MAC. J Anesth Clin Res. 12:1018
Received: 09-Jul-2021 Accepted: 23-Jul-2021 Published: 30-Jul-2021 , DOI: 10.35248/2155-6148.21.12.1018
Copyright: © 2021 McMurray R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.