
Journal of Clinical Trials
Open Access
ISSN: 2167-0870

ISSN: 2167-0870
Research - (2022)Volume 12, Issue 5
Objective: To improve the quality of health care, the Ministry of Health and Welfare of Taiwan start to launch a project in June 2015, providing community outreach services and outpatient psychiatric treatment to schools, institutions for child and adolescent patients with mental disabilities. The main purpose of this study was to analyze the development of the project and intended to promote medical service quality for child and adolescent patients.
Methods: Service team members from eight medical centers and psychiatric hospitals in Taiwan, providing both outreach community services and outpatient psychiatric treatment. We collected the personal information and assessment scale scores of all patients from January 2016 to December 2021 (N=432).
Results: The findings revealed significant improvement in the scores of C-GAS, PSP, CGI-S, and CGI-I (p<0.001). The scores of the self-reported assessment scale ASEBA also showed significant improvement for internalizing problems, externalizing problems and total problems (p<0.001). Most of the disabled children and adolescents have benefited greatly from this project, including presenting less disruptive behavior, fewer hospital readmissions, and more improved adaptation.
Discussion: This 6-year community-based follow-up treatment shows that the majority of disabled patients continue experiencing an improved condition after intervention.
Community mental health outreach services; Community-based medical service model; Comorbidities; Mental disability; Outpatient psychiatric treatment
Enormous progress has been studied in recognizing, diagnosing, and treating child and adolescent with mental disabilities and psychiatric disorders, such as intellectual disabilities, Autism Spectrum Disorder (ASD), Attention Deficit Hyperactivity Disorder (ADHD) and so on [1]. The behavior of Child and adolescent patients with mental disabilities and psychiatric disorders may be difficult to manage due to behavioral abnormalities, including angry and irritable mood, impulsive, aggressive, destructive, obsessive, ritualistic, self-stimulating and self-harm behaviors that might cause potential physical and psychological harm to their parents as well as other caregivers, siblings, teachers or classmates [2]. They are at increased risk for developing emotional and behavioral difficulties; moreover, they often have lower academic performance and poor psychosocial adjustment. Parents or caregivers will experience overwhelming caring burdens, and thus need more support from medical and education specialists to help them go through the stressful period [3,4].
The overall goal of treatment is to reduce impairments and the extent of disability. Early intervention for child and adolescent patients with mental disabilities can facilitate their cognitive, communication, self-care ability, emotion regulation skills, and thus enhance their social adaptation, reduce further medical use and costs, as well as avoiding further morbidity and disability [5]. Previous studies in Taiwan have indicated that enhancing parenting skills and providing sufficient family support during early intervention correlated with the positive outcome of children [6]. In order to reduce delay in medical treatment, decrease admission and relapse rates, the family members, caregivers, and teachers of child and adolescent patients with mental disabilities must acquire more knowledge about psychosis and behavioral disturbance and management skills to address their mood and behavioral problems, and mental health services may provide them with related practical knowledge and management skills [7].
The lack of mental health care for children and adolescents has always been considered an important public health issue. Based on a study in Taiwan [1,2], the prevalence of early onset of mental illness in childhood was approximately 22.7%, and it was estimated about 14.8 to 20.3% of the children and adolescents in grade 7 to 9 need the psychiatry services. However, only 2.5% of the population aged 10 to 14 sought and took the mental health services. The survey indicated that the mental health services received by children and adolescents in Taiwan are far below the requirements. Furthermore, it not only reflected the importance of improving the utilization of psychiatry services in children and adolescents with mental disabilities and psychiatric disorders, but highlighted the importance of medical professionals actively entering the community to provide mental health services.
In Taiwan, Child and adolescent patients with mental disabilities and psychiatric disorders, especially the students of special education classes and schools, often do not receive adequate medical services from the current National Health Insurance system. Many parents and teachers in Taiwan said that their children and students with mental disabilities and psychiatric disorders have received insufficient medical service, resulting in having great suffering and stress while taking care of them. The current Taiwan Health Insurance System cannot fully assist these disabled children and adolescents indeed.
In view of the current shortcomings of Taiwan’s health care system, the Ministry of Health and Welfare of Taiwan first has launched a project since June 2015 and provided community mental health outreach services and outpatient psychiatric treatment for child and adolescent patients with mental disabilities and psychiatric disorders for schools and social welfare institutions. This project provided special budgets to all the contract cooperation hospitals in Taiwan to set up a special clinic in the hospital and assign a professional medical team (a child psychiatrist, a clinical psychologist, a case manager) to offer outreach services to the community, schools, and social welfare institutions (Figure 1).
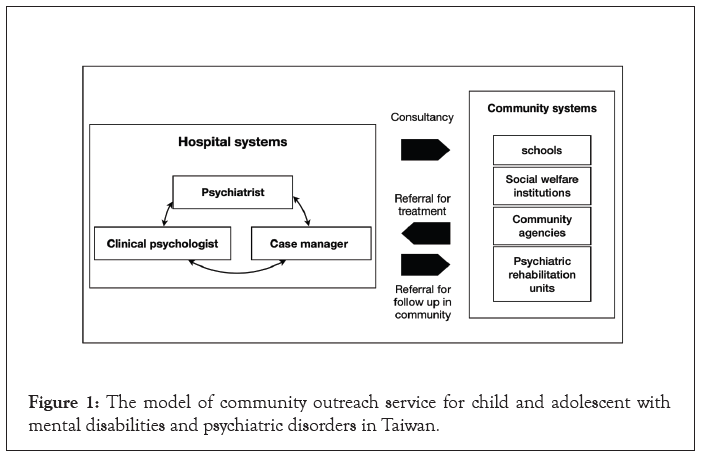
Figure 1: The model of community outreach service for child and adolescent with mental disabilities and psychiatric disorders in Taiwan.
The main purpose of this project was to promote the current mental service quality for child and adolescent patients with mental disabilities and psychiatric disorders in Taiwan, including establishing mutual referral and integrating mental community care for child and adolescent patients with mental disabilities and psychiatric disorders. This project would make up for the deficiency of the original medical resources for child and adolescent patients with mental disabilities and psychiatric disorders providing from National Health Insurance program through early detection and management.
In the period from January 2016 to December 2021, nationwide eight cooperative hospitals, including medical centers and psychiatric hospitals engaged in this project (Figure 2). The service team members from the eight cooperative medical centers and psychiatric hospitals in Taiwan provided both outreach services and outpatient psychiatric treatment, and collected the personal information and survey data of all the disabled patients. The outcome and effectiveness of community mental health outreach services combined with outpatient treatment must be evaluated. In the present study, we intend to analyze the demographic data and assessment scale scores of the outpatients and evaluate the effectiveness of outreach services and outpatient treatment for child and adolescent patients with mental disabilities and psychiatric disorders.
Figure 2: The location of 8 cooperative medical centers and psychiatric hospitals. Note:  Medical centers;
Medical centers;  psychiatric hospitals
psychiatric hospitals
Data source and study procedure
In this project, the service team members from eight medical centers and psychiatric hospitals in Taiwan provided both outreach community services and special outpatient psychiatric treatment. In the special outpatient clinic of this project, the psychiatrists have to spend more than 30 minutes for each outpatient visit (Figure 3). Both psychiatrists and clinical psychologists tried to comprehensively evaluate and deal with the outpatients’ mental disabilities and psychiatric disorders. The case manager kept following up each outpatient’s mental health status during and after the treatment course with telephone and outreach service. The service team members made great efforts to cooperate and work with both the outpatient’s family members and caregivers during the provision of outreach services and in the special clinic. Case conferences and symposiums might be arranged for some outpatients with challenging behavioral and emotional problems in the community.
Figure 3: The connection among patients, the project-executing groups and community agencies.
The Ministry of Health and Welfare of Taiwan also provided another fund into establishing a management center for the supervision of special clinics and outreach services in eight nationwide hospitals. The management center constructed an information platform to collect and organize the questionnaire data of each outpatient from special clinics of all cooperative hospitals. The personal information and survey data of all outpatients treated at the special clinics were uploaded onto the information platform, and the information of all outpatients was protected by delinking any identifying information from the main database and sources. In 2021, we totally provided a nationwide medical service and outreach treatment to 30 regional psychiatry centers, 30 social welfare institutions, and 41 schools, including general and special schools. Also, we connected the longterm care service and exchanged some professional experiences with judicial systems if needed, constructing a more complete communitybased social care network (Figure 3).
The institutional review board of Kaohsiung Municipal Kai-Syuan Psychiatric Hospital has approved this study to evaluate the quality and outcome of medical service for child and adolescent patients with mental disabilities and psychiatric disorders. We collected the personal information and survey data of all patients from the eight hospitals in this project from January 2016 to December 2021. Specifically, the basic data of these outpatients were collected at the first patient treatment visit and comprised information on age, gender, source of referral, and major diagnoses. We used structural assessment scales to assess the patients’ condition, including the Clinical Global Impression-Severity Scale (CGI-S), Children's Global Assessment Scale (C-GAS), and Achenbach System of Empirically Based Assessment (ASEBA). During the subsequent service and outreach treatment period, the psychiatrist recorded the scores of CGI-S, the Clinical Global Impression-Improvement Scale (CGI-I), Personal and Social Performance Scale (PSP) and C-GAS in every visit, and ASEBA scores were also obtained from the patients’ parents or caregivers at least once every three months. The inclusion criteria were being a patient and having complete first service and outreach treatment and basic data available on the information platform. Excluded were those patients with age of 18 years and older, loss to follow-up after the first service and outreach treatment, and incomplete data of assessment scales from the subsequent service and outreach treatment.
Structural assessment scales
C-GAS: Three common scales, Children’s Global Assessment Scale (C-GAS), Axis-V in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Global Assessment of Functioning (GAF), and Axis-VI in ICD-10 Global Assessment of Psychosocial Disability (GAPD), have been used as important global assessment of functioning in clinical work, as well as in epidemiological studies and treatment research.
C-GAS is a measure for assessing the severity of psychiatric disturbance and social disability. It has a range of 1 to 100 and provides anchor point descriptions of behavioral function. It is designed for use with children from 4 to 16 years of age. C-GAS can identify the effectiveness of psychiatric treatment, have predictive value, and can measure changes over time. Some studies have reported the reliabilities of C-GAS range from fair to substantial [8].
PSP scale: The PSP scale is a reliable and valid measurement tool of patients' personal and social functioning, widely used for the assessment of social functioning in adult patients with schizophrenia. It is a clinician-administered scale, rating behavior on a 6-point Likert-scale in four main areas: (1) socially useful activities; (2) personal and social relationships; (3) self-care and (4) disturbing and aggressive behaviors. For each domain, a clinician rates the functional impairment as absent, mild, manifest, marked, severe, and very severe. The PSP is a 100-point single-item rating scale, subdivided into 10 equal intervals. A total final decile score ranging from 0 to 100 is derived by differentially weighting the four domain scores [9].
The Taiwanese Mandarin Version of PSP (TMV-PSP) is a reliable and valid instrument for the assessment of social functioning in patients with schizophrenia. PSP scores showed a positive correlation with GAF scores and significant correlations with the severity and improvement in CGI scale scores at follow-up. High inter-rater reliability and testretest reliability were also found [9].
CGI-S and CGI-I scale: The CGI scale was developed for use in clinical trials to provide a brief, useful and stand-alone assessment of the clinician’s view of the patient's global functioning before and after initiating a medical treatment. It was also an understandable quantification method that could facilitate treatment over time. The CGI provides an overall clinician-rated summary measure that all available information, including a knowledge of the patient's history, psychosocial circumstances, symptoms, behavior, and the impact of the symptoms on the patient's ability to function. Inherent to the validity of the CGI is the requirement of a trained clinician with knowledge of the patient to administer the scale.
The CGI is comprised of three ordinal scales, designated as Severity of Illness (CGI-S), Global Improvement (CGI-I) and Efficacy Index. The CGI-S rates the severity of the patient's illness, on a 7-point scale ranging from “normal” 1 to “extremely ill” 7, according to the clinician's experience of patients suffering from the same condition. The CGI-I assesses the extent of clinical change in the patient at the point of assessment compared with baseline (initiation of treatment), and likewise has a 7-point scale, from “very much improved” 1 to “very much worse” 7 [10].
Achenbach System of Empirically Based Assessment (ASEBA)
ASEBA created by Thomas Achenbach, is a questionnaire used to assess and identify adaptive, maladaptive behavior and overall functioning in children and adolescents. ASEBA is used in various situations, including mental health, school, research, and forensic settings, and it can be self-reported or administered by lay interviewers. ASEBA can be used to assess multiple age groups, including preschoolaged children, school-aged children, adults, and older adults.
The system includes report forms for multiple informants-the Child Behavior Checklist (CBCL) is used for caregivers to fill out ratings of their child's behavior, the Youth Self Report Form (YSR) is used for children to rate their own behavior, and the Teacher Report Form (TRF) is used for teachers to rate their pupil's behavior. The ASEBA seeks to capture consistencies or variations in behavior across different situations and with different interaction partners. Scores for individuals in each age group are norm-referenced. ASEBA has been translated in one hundred languages, with various multicultural applications [11].
Statistical analysis
We did statistical analyses on the study data in two stages. First, we identified demographic variables with descriptive statistics. Subsequently, we assessed treatment effectiveness by using the paired sample t test.
All analyses were conducted using Statistical Package for Social Science software version 17 for Windows (International Business Machines SPSS Statistics, IBM Corp., Chicago, Illinois, USA). The differences between groups were considered significant if p-value were smaller than 0.05 (two-tailed).
We collected the personal information and assessment scale scores of 432 child and adolescent patients under the age of 18 who completed data of the first and following service and outreach treatment from the database in this project from January 2016 to December 2021. Table 1 shows the demographic and clinical characteristics of those patients. We compared first scores of C-GAS, PSP, CGI-S, CGI-I, and ASEBA of those patients with their latest scores, and data analysis results are listed in Table 2.
| Characteristics | 2016(n=101) | 2017(n=121) | 2018(n=24) | 2019(n=33) | 2020(n=90) | 2021(n=63) | All(n=432) |
|---|---|---|---|---|---|---|---|
| Gender | |||||||
| Male | 76 | 88 | 16 | 29 | 61 | 48 | 318 |
| Female | 25 | 33 | 8 | 4 | 29 | 15 | 114 |
| Age | |||||||
| 0 to 6-year-old | 10 | 16 | 4 | 17 | 1 | 6 | 54 |
| 7 to 12-year-old | 49 | 68 | 10 | 7 | 33 | 36 | 203 |
| 13 to 18-year-old | 42 | 37 | 10 | 9 | 56 | 21 | 175 |
| Source of referral | |||||||
| Coming on their own | 60 | 63 | 9 | 27 | 44 | 36 | 239 |
| Psychiatric hospitals or clinics | 7 | 8 | 1 | - | 1 | 4 | 21 |
| Institutions | 5 | 9 | 7 | 1 | 18 | 2 | 42 |
| Schools | 29 | 41 | 7 | 5 | 27 | 21 | 130 |
| Major diagnosis | |||||||
| Attention-deficit/hyperactivity disorder | 41 | 56 | 6 | - | 22 | 19 | 144 |
| Multiple disabilities | 5 | 1 | - | - | 1 | - | 7 |
| Autism spectrum disorder | 28 | 27 | 9 | 26 | 32 | 23 | 145 |
| Intellectual disability | 15 | 19 | 6 | 7 | 19 | 7 | 73 |
| Developmental delay | 4 | 4 | - | - | - | 1 | 9 |
| Other disabilities | 8 | 14 | 1 | - | 6 | 8 | 37 |
| Other psychiatric disorder | - | - | 2 | - | 10 | 5 | 17 |
Table 1: Demographic and clinical characteristics of patients.
| Mean ± SD | ||
|---|---|---|
| Assessment scales | First scores of service and outreach treatment | Latest scores of service and outreach treatment |
| C-GAS | 57.93 ± 11.943 | 68.30 ± 9.735*** |
| PSP | 58.12 ± 13.026 | 67.94 ± 10.768*** |
| CGI-S | 4.03 ± 0.953 | 3.17 ± 0.931*** |
| CGI-I | 3.19 ± 0.737 | 2.88 ± 0.964*** |
| ASEBA | ||
| Internalizing problems | 63.91 ± 11.607 | 61.56 ± 12.082*** |
| Externalizing problems | 63.82 ± 10.297 | 61.80 ± 11.090*** |
| Total problems | 67.34 ± 9.718 | 65.68 ± 10.616*** |
Note: *p<0.05, ** p<0.01, *** p<0.001; C-GAS: Children's Global Assessment scale; PSP: Personal and Social Performance scale; CGI-S: Clinical Global Impression - Severity scale; CGI-I: Clinical Global Impression - Improvement scale; ASEBA: Achenbach System of Empirically Based Assessment
Table 2: The analysis of assessment scales’ scores of patients (N=432).
From the database in this project, the 432 patients are composed of 318 males and 114 females. The major diagnosis of these patients was autism spectrum disorder (n=145, 34%), attention-deficit/ hyperactivity disorder (n=144, 33%), and intellectual disability (n=73, 17%). They were referred to a psychiatrist for persistent psychiatric outpatient treatment and for further evaluation and management of a possible psychiatric disorder from schools (n=130, 30%), institutions (n=42, 10%), and psychiatric hospitals or local medical departments (n=21, 5%; Table 1).
Comparison of the first assessment scale scores with the latest assessment scale scores revealed significant improvement of all index, including C-GAS, PSP, CGI-S, and CGI-I scores (p<0.001). The scores of the self-reported assessment scale ASEBA also showed significant improvement for internalizing problems, externalizing problems and total problems (p<0.001) of ASEBA (Table 2).
Our project can be considered as secondary and tertiary prevention, which involves screening and further direct treatment. With early intervention, it may be possible to recognize a condition, slow its progression, prevent or minimize complications and limit any resulting disability. Furthermore, with the direct medical treatment, it may improve the quality of life of those affected by limiting complications and disabilities, reducing the severity and progression of mental disabilities and providing rehabilitation to restore functionality and self-sufficiency [5]. Most child and adolescent patients with autism spectrum disorder and intellectual disabilities have psychiatric comorbidities and other emotional and behavioral problems that require more medical services [12,13]. However, parents or caregivers of these child and adolescent patients often complain about the shortage of medical service, referral and care resources, and high financial and caring burdens [14]. In Taiwan and other developed countries, parents of child and adolescent with mental disabilities and psychiatric disorders still face many barriers and challenges when attempting to access timely, appropriate health services in their communities, such as the accessibility and affordability to healthcare resources [15].
In recent years, several countries in Asia, such as Singapore, Japan and South Korea, have begun providing community mental health outreach services for people with mental disabilities and psychiatric disorders. In Singapore’s national project for mental health of child and adolescent patients, mental health professionals joined together to form community-based multidisciplinary teams that worked directly with school counselors, providing consultation services to child and adolescent patients with mental health disorders [16,17]. This community mental health service model in Singapore has shown favorable results from CGI scale and Strength and Difficulties Questionnaire (SDQ) and adequate costeffectiveness for child and adolescent patients with mental illness [18]. In 2011, the Japanese Ministry of Health, Labor and Welfare set up the Japan Outreach Model Project to provide multidisciplinary outreach services for adult patients with mental disorders in the community. Different from the ordinary outpatients accepting the care of public insurance in Japan, the participants in this model of outreach services had lower readmission rates, improvement of social functioning and fewer problematic behaviors [19]. In South Korea, one of the most common forms of community mental health outreach services is school-based screening and treatment linkage programs. There are three official institutions conducting this program, showing that the key elements for successful screening and referral programs were an effective school/community mental health center/Office of Education network, the parents' financial support and perception of their child's mental health status as being problematic, and the teachers' active engagement. Therefore, an effective network for community mental health and improvements in parents' and teachers' perceptions regarding mental health are needed for more successful treatment linkage [20].
According to the result of our survey, the national project in Taiwan that integrated outreach services with outpatient psychiatric treatment for child and adolescent patients with mental disabilities and psychiatric disorders provided more effective medical services and treatment. The scores of clinical structural assessment scales, including C-GAS, PSP, CGI-S, and CGI-I revealed significant improvement of outpatients’ disease severity and their adaptive functioning (p<0.001; Table 2). The quality and effectiveness of intervention programs and the results of the self-report assessment scale ASEBA were also similar to the outpatients and their family (Table 2).
Comparing the community mental health service model in Singapore, our service teams in this project provided the similar outreach service to both child and adolescent patients with mental disabilities and their parents or caregivers, and we also made great efforts to identify and manage their follow-up medical intervention and further arrangement. Previous research has found that community mental health services in Singapore, Japan, South Korea and Taiwan are well-received by schools and institutions in the community. Especially in one Singapore’s study, many indices of clinical improvements have showed a great positive change in CGI-S, and also on the SDQ [18]. On the other hand, our study findings in this project not only presented clinical improvement by CGI-S, CGI-I, and ASEBA, but also showed functional improvement by C-GAS and PSP (Table 2).
Based on the study results of this project and daily observations from parents, caregivers, and teachers, most patients who have accepted the community mental health outreach services and medical treatment, presented fewer mood symptoms or behavioral disturbance, more improved adaptation, and higher academic performance at schools and institutions. Community mental health outreach services can integrate outpatient psychiatric treatment for child and adolescent patients with mental disabilities and psychiatric disorders, who need further psychiatric referral and treatment. Outreach programs are considered a key strategy for providing services to underserved populations and play a central role in delivering health-care services. This medical service model may help child and adolescent patients to improve their symptoms at the early stage of psychiatric disorders, and prevent further morbidity and disability due to delayed identification and treatment.
On the basis of more than six years’ experience in executing this project, the medical service model indeed enabled early detection and intervention of psychiatric disorders in child and adolescent patients with mental disabilities and promoted the quality of health care and medical service under fair partnership and cooperation with the patients’ family members, caregivers, and teachers. Our survey provided some information regarding this project, and further research on this medical service model is needed for implementing more effective public mental health policy for child and adolescent patients with mental disabilities and psychiatric disorders.
Study limitations
Our study results should be interpreted with caution due to the following major limitations. First, this project was assigned to only eight hospitals from different areas in Taiwan. The study results and conclusion may not be totally applicable to all areas in Taiwan. Second, it should be taken into considered that every outpatient had a different outreach service and outpatient treatment status during the treatment period. The number and frequency of outpatient treatment of each outpatient and the resources of medical services varied due to different diagnoses and illness severity in all outpatients. Furthermore, during the year of 2021, the COVID-19 pandemic hit and many schools were closed, child and adolescent patients with mental disabilities and psychiatric disorders have experienced a more severe impact than their peers. We did not discuss the further negative influence of the COVID-19 pandemic.
Considering the limitation of methodology, some outpatients were lost to follow-up due to some unavoidable circumstances; we did not analyze comprehensive information of those missing data. Also, we did not have a control group to compare the experiment effect in this study. Finally, many confounding variables that may affect the functioning of child and adolescent patients were not considered in this study, including the socioeconomic status, the parents’ level of education, the difference of using and not using medication, and the utilization of related educational and counseling resources.
This study has been approved by the institutional review board of Kaohsiung Municipal Kai-Syuan Psychiatric Hospital (IRB NO. KSPH-2022-03) on March 22, 2022 for the purpose of evaluating the quality and outcome of medical service for child and adolescent patients with mental disabilities and psychiatric disorders.
The named authors declare no potential conflicts of interest.
Hsieh, Hsu and Tsai conceived of the presented idea and wrote the main manuscript text. Li, Ou and Chang verified the analytical methods and prepared the figures and tables. Chen supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
The authors thank the original data sources from the Ministry of Health and Welfare of Taiwan.
The authors acknowledge the cooperation of all the staff at medical centers and psychiatric hospitals in Taiwan. The authors also thank the study participants who took part in this study and thank Frank Huang-Chih Chou, Director of Kaohsiung Municipal Kai-Syuan Psychiatric Hospital, for the comments and suggestions.
The authors thank the financial support for this project and original data sources from the Ministry of Health and Welfare of Taiwan.
The named authors declare no potential conflicts of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Hsieh W, Hsu C, Li W, Tsai C, Ou T, Chang C, et al. (2022) The Outcome of Nationwide Community Outreach Service for Child and Adolescent with Mental Disabilities and Psychiatric Disorders in Taiwan: A 6-Year Follow-up Study. J Clin Trials. 12:510.
Received: 21-Sep-2022, Manuscript No. JCTR-22-19326; Editor assigned: 23-Sep-2022, Pre QC No. JCTR-22-19326 (PQ); Reviewed: 07-Oct-2022, QC No. JCTR-22-19326; Revised: 14-Oct-2022, Manuscript No. JCTR-22-19326 (R); Published: 21-Oct-2022 , DOI: 10.35248/2167-0870.22.12.510
Copyright: © 2022 Hsieh W, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.