Andrology-Open Access
Open Access
ISSN: 2167-0250
ISSN: 2167-0250
Perspective - (2024)Volume 13, Issue 5
Among men, even before COVID-19, the popularity of testosterone therapy since 2000 likely outpaced the clinical need. There have been a number of proposed reasons for this, such as increased direct-to-consumer marketing for low testosterone treatments and the rise of clinics based around testosterone prescribing hidden under the guise of Men’s health. Much of this growth was seen from 2000-2013 in older men before a decline around the time the Food and Drug Administration (FDA) restricted the indications and voiced safety concerns around testosterone therapy. Still, since that time and especially through the COVID-19 pandemic, there appeared to be raising interest in testosterone therapy in a new demographic.
Utilizing individual state controlled substance prescribing databases, we sought to capture the breadth of testosterone use patterns for all peoples filling prescriptions, including those going outside of their insurance to ‘get help’. Our combined findings pointed to answers that raised more questions [1,2].
Many more men are using testosterone therapy than before-why?
Testosterone therapy has seen continued growth, but it seems this leapt to new levels during the pandemic. We know some conditions had rising prevalence during that timeunemployment and with it the loss of health insurance and wages to afford to seek healthcare for chronic conditions, mental health problems like anxiety, depression, substance abuse, loneliness and of course COVID-19. It seems likely the nonspecific symptoms of hypogonadism that overlap with many of those conditions, researched in the vacuum of the internet, could easily point men to errantly self-diagnose hypogonadism and seek out treatment for it.
Most of these men are different than those studied why?
The testosterone trials showed modest efficacy in several areas for men averaging 72 years of age [3]. The TRAVERSE study showed showed testosterone gel was likely safe for men averaging 63 years old [4]. The problem is that in our recent study, nearly 80% of men on testosterone therapy in 2022 were younger than 65 and over a quarter were younger than 45. There exists no large-scale safety or efficacy data for long term testosterone therapy for these men. We found 1.3 million men under treatment trusting research that may not apply to them and we cannot guess at the harms and benefits of testosterone [1]. Testosterone therapy is purported to reduce the risk of diabetes and improve bone density, but recent analyses have not supported those hypotheses [5,6].
What else have we gotten wrong?
In most large trials, testosterone gels are used to assess efficacy and safety, largely due to sponsorship and also ease of use [3,4]. But at least 60% of men are using injectable testosterone and while the relative equivalence in safety of the testosterone gels has been assumed, the little research available suggests that is not the case and that there may be an excess of cardiovascular risk from using these over topical formulations shown in Figure 1 [2,7].
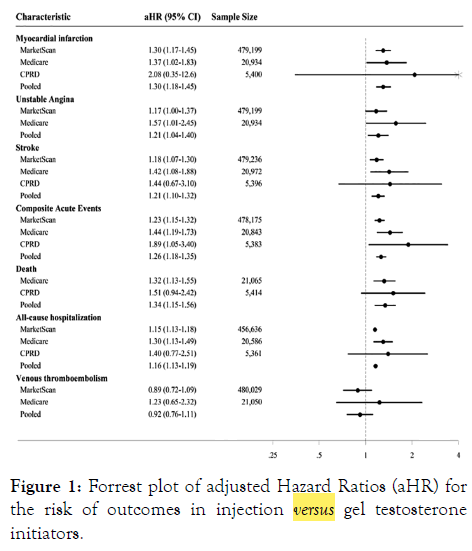
Figure 1: Forrest plot of adjusted Hazard Ratios (aHR) for the risk of outcomes in injection versus gel testosterone initiators.
Many of these men have sought care through virtual clinics [8]. These telehealth operations are not known for using evidencebased guidelines to diagnose and treat people seeking care [9]. They are part of a business model designed to grow their clientele, which they have done quite successfully. In our study in Texas, men’s health clinics are multiplying with mid-level supervisory models of care. In 2021, a single physician signed off on prescriptions for over five thousand unique patients-thirteen different patients every single day of the calendar year. In contrast, the average doctor treated five patients per year. The ease of access to and profitability of testosterone therapy is undoubtedly contributing to the trend of increased use.
It has been purported that average testosterone levels in American men have been declining and more recently, identified the correlation between lower testosterone levels and increased mortality [10]. This is justifiably concerning but has led to the shortsighted answer of 'just make the little numbers big' to solve the problem.
This approach has not worked for other negative correlates with health-we have stopped using niacin to increase High- Density Lipoprotein (HDL), we no longer try to transfuse people’s hemoglobin back to normal levels, and we have seen the harm in trying to medicate the blood sugars of people with diabetes back to normal as well. Medications have mostly not been a sustainable answer to problematic health trends-this is true even with testosterone, where both clinical trials and real-world experience have shown extremely poor adherence [2,4,11].
The societal impact of this focus on testosterone is that it takes away healthcare resources, efforts and spending from more sustainable and holistic approaches to health, the sad irony being that is what most patients are actually seeking. The effects of unaddressed healthcare issues-obesity, sedentary lifestyle, poor diet, lack of affordable food options, poor sleep, lack of support for mental health, environmental toxins-all are glossed over in the rush to ‘Treat’ a number [12,13]. It is not that simple, men show a delay in health-seeking behavior and traditional healthcare utilization likely leading to our higher morbidity and mortality rates across a number of conditions including cardiovascular disease and cancer [14].
We need more accessible and acceptable programs directed towards opening up health discussions for men. This has been shown to be effective for blood pressure control and mental health through a community-based approach in barbershops and for weight management utilizing professional football (soccer) clubs. We need more of these innovative approaches to meet men where they are more open to discussion of these modifiable risk factors for disease and it is time to move beyond reducing men’s health to a discussion about testosterone.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Selinger S (2024). The Pandemic Epidemic: Time to Move Beyond Testosterone Prescribing for Men. Andrology. 13:328.
Received: 15-Sep-2024, Manuscript No. ANO-24-34123; Editor assigned: 18-Sep-2024, Pre QC No. ANO-24-34123 (PQ); Reviewed: 02-Oct-2024, QC No. ANO-24-34123; Revised: 09-Oct-2024, Manuscript No. ANO-24-34123 (R); Published: 16-Oct-2024 , DOI: 10.35248/2167-0250.24.13.328
Copyright: © 2024 Selinger S. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.