
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2018) Volume 9, Issue 12
Background: Mask ventilation is the primary technique of ventilation before insertion of any airway device. Difficulties in mask ventilation have been associated with serious complications, such as death or hypoxic brain damage. If the anesthetist can predict which patients are likely to prove difficult to ventilate, he/she may reduce the risks of anesthesia considerably. The study was aimed to assess the incidence of and predictive values of anatomical parameters for difficult mask ventilation among patients who underwent elective surgeries at Wolaita Sodo University teaching and referral Hospital and Sodo Christian Hospital.
Methods: Institutional based cross sectional study was conducted from July 1 to August 30, 2017 in two hospitals of wolaita zone. The study was conducted on 278 patients of which 101 (36.3%) were males and 177 (63.7%) were females. Patient demographics, incidence and predictive values of anatomical parameters for difficult mask ventilation were studied among elective patients who took general anesthesia.
Result: The incidence of difficult mask ventilation (grade III) was 2.2%; whereas, impossible mask ventilation (grade IV) was 0.4%. Highest percent of difficult mask ventilation (grade III) was occurred in patients with obstructive sleep apnea, BMI˃26 kg/m2 and Mandibular Protrusion Class C.
Conclusion: Modified Mallampatti class III and IV and Mandibular protrusion class B and C are highly accurate parameters with high specificity, negative predictive value and positive predictive value to predict difficult mask ventilation.
Keywords: Difficult mask ventilation; Impossible mask ventilation; Anatomical parameters
Mask ventilation is an integral skill for all anesthetists. It forms the starting point of the majority of general anesthetics and more importantly, it is an essential fall-back technique for maintaining oxygenation during a failed or difficult intubation. Despite its importance, less attention is devoted to mask ventilation in research papers and textbooks, with a larger focus on difficult or failed intubation [1].
Difficult mask ventilation is defined as a situation in which: “It is not possible for the anesthesiologist to provide adequate ventilation because of one or more of the following problems: inadequate mask seal, excessive gas leak, or excessive resistance to the ingress or egress of gas [2].
Failure to anticipate difficult mask ventilation before anesthesia induction is in 57% of the patients who were ultimately difficult to ventilate [3-5]. There is a wide variation in the reported incidence of difficult mask ventilation (DMV) in the literature. Whereas one study reported an incidence as low as 0.08%, another reported a 15% incidence. The highest incidence (15%) was reported from a retrospective study of subjects who had difficult intubation. The majority of prospective studies, on the other hand, reported a lower incidence. 0.9% [4], 5% [5] and 7.8% [6,7].
The large prospective study of 22,660 MV attempts used a DMV grading scale and reported an incidence of 1.4%. Because this is the large and most recent study and because the reported incidence is in agreement with several other studies 1.4% may be considered the most likely estimate in the general population [8].
Study area and period
Study was conducted in wolaita Sodo University teaching referral hospital (WSUTRH) and Sodo Christian hospital (SCH) in Wolaita Sodo town. The study was conducted from July 1- August 30, 2017.
Study design
An Institution based cross-sectional study was used.
Study population
Surgical patients admitted to Wolaita Sodo university teaching and referral hospital and Sodo Christian hospital. Patients who were scheduled for elective surgery under general anesthesia at WSUTRH and SCH from July 1- August 30, 2017 were selected.
Eligibility criteria
Patients who underwent elective surgery under general anesthesia are included. However, critically ill patients in which airway assessment is difficult; Age less than 18 years; Psychiatric patients; and Patients scheduled for thyroid and maxillofacial surgeries were exclusive.
Sample size determination and Sampling technique
Sample size was determined using finite population correction formula by assuming the prevalence as 0.5 and 5% margin of error at 95% confidence interval using the following formulas:
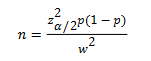
Where n=sample size, z=1.96, p= 0.5, w=0.05, CI= 95% & ἀ=5%; n=(1.96)2 × 0.5 (1−0.5) (0.05)2=384;
Since source populations are less than 10,000, correction formula was used. Based on this, nf=n/(1+n/N), N=833 (estimated target population in the study period). Nf=(1+384/833) which was nf=263. When 10% non-response rate was added, final nf would be 286.
Therefore, a total sample size of 286 elective surgical patients was planned to participate in this study.
Data collection technique
Structured questionnaire prepared in English and Amaharic was used. During data collection ten, BSc holders and one MSc holder was involved as data collector and supervisor respectively. Patients scheduled for elective surgery under GA was assessed at the waiting room immediately before their entry to the operation room. Then, after adequate preparation of necessary equipment’s each patient was observed for difficult mask ventilation in the operation room while qualified anesthetist applying mask ventilation and one anesthetist grading mask ventilation according to Han’s Mask Ventilation Classification and Description Scale.
Data quality assurance
One full day training was given for the data collectors and supervisor. During data collection, close supervision and follow up was made. The collected data was cross checked for its completeness, clarity and consistency.
Ethical considerations
Ethical clearance was obtained from Department of Research Ethics Review Committee (DRERC), Addis Ababa University. Then, a letter of support and permission was given to the hospital administrators. Informed verbal consent was secured from every study participants. Confidentialities and anonymity was ensured.
Data analysis
Data with complete information was entered to SPSS version 20. The descriptive statistics and Receiver Operating Characteristics (ROC) curve was performed. The validity of parameters (screening tests) such as sensitivity, specificity, positive predictive values and negative predictive values was performed using crosstabs.
Operational definitions
American Society of Anesthesiologists (ASA) [9] physical status: is a method of categorizing patients’ physical state developed by the ASA task force which classifies patients according to their physical status (systemic wellbeing). It is classified into six classes:
Class definition
ASA 1: Normal healthy patient
ASA 2: Patient with mild systemic disease (no functional limitations)
ASA 3: Patient with severe systemic disease (some functional limitations)
ASA 4: Patient with severe systemic disease that is a constant threat to life (functionality incapacitated)
ASA 5: Moribund patient who is not expected to survive without the operation
ASA 6: Brain-dead patient whose organs are being removed for donor purposes
E: If the procedure is an emergency, the physical status is followed by “E” (for example, “2E”)
Kyphosis (hunch back) overinflated thoracic & sacral curves
Scoliosis is exaggerated lateral deviation of 3rd to 6th thoracic vertebrae
Kyphoscoliosis (KS) is a deformity of the spine characterized by abnormal curvature of the vertebral column in two planes (coronal and sagittal). It is a combination of Kyphosis and scoliosis.
General anesthesia: medically induced reversible loss of consciousness, loss of protective reflexes resulting from administration of one or more general anesthetic agents
Difficult airway: is defined as the clinical situation in which a conventionally trained
Anesthetist experiences difficulty with facemask ventilation of the upper airway, difficulty with tracheal intubation, or both
Difficult mask ventilation is a situation in which: “It is not possible for the anesthesiologist to provide adequate ventilation because of one or more of the following problems: inadequate mask seal, excessive gas leak, or excessive resistance to the ingress or egress of gas.”
Classification description: Han’s Mask Ventilation Classification and Description Scale
Grade 0 Ventilation by mask not attempted
Grade 1 Ventilated by mask
Grade 2 Ventilated by mask with oral airway or other adjunct
Grade 3 Difficult mask ventilation (Inadequate, unstable, or 2 person technique)
Grade 4 Unable to mask ventilate
Inter incisor distance (IID): It is the distance between the upper and lower incisors. A value of less than 3 patient’s fingers or less than 3cm predicts difficult airway.
Mandibular protrusion (MP): the lower incisors can be brought in front of the upper incisors: inability to bring the lower incisors to the upper or Mandibular protrusion class B & C suggests difficulty.
Mallampatti class (MMC): The Mallampatti classification correlates tongue size to pharyngeal size. This test is performed with the patient in the sitting position, head in a neutral position, the mouth wide open and the tongue protruding to its maximum. Classification is assigned according to the extent the base of tongue is able to mask the visibility of pharyngeal structures into four classes, I-IV:
Class I: Visualization of the soft palate, fauces; uvula, anterior and the posterior pillars.
Class II: Visualization of the soft palate, fauces and uvula.
Class III: Visualization of soft palate and base of uvula.
Class IV: Only hard palate is visible. Soft palate is not visible at all. Mallampatti class III & IV suggests difficult laryngoscopy. Class 3 or 4 suggests a significant chance that the patient will be difficult to intubate.
Sternomental distance (SMD): is the distance from the suprasternal notch to the mentum and measured with the head fully extended on the neck with the mouth closed. A value of less than 12 cm is found to predict a difficult airway.
Surgical patients: are patients who admitted to all available wards in hospital and who undergo surgery.
Thyromental distance (TMD): is defined as the distance from the mentum to the thyroid notch while the patient’s neck is fully extended. A value of less than 6 cm predicts difficult airway.
Obstructive sleep apnea (OSA) is frequent episodes of apnea during sleep, snoring, and daytime symptoms, which include sleepiness, impaired concentration, memory problems and morning headaches.
Personal socio-demographic characteristics
The study was conducted on 278 patients of which 101(36.3%) were males and 177(63.7%) were females. The highest number of cases 57.6% (n=160) were belonged to the age group of 18-40. The mean age of study population was 36.21 ± 10.9 (minimum 18 and maximum 76). Out of 278 Patients 163(58.6%), 108 (38.8), 7 (2.5%) were ASA physical status class I, II, and III respectively. There were no cases with ASA physical status class IV or V. Majority of cases was within ASA physical status class I and age group 18-40. The numbers of female patients were higher than males with the ratio of (1.7:1)(Table 1).
| Variable | Category | Frequency | Percentage |
|---|---|---|---|
| Sex | M | 101 | 36.3 |
| F | 177 | 63.7 | |
| Age group | 18-40 | 160 | 57.6 |
| 41-60 | 111 | 39.9 | |
| ≥ 60 | 7 | 2.5 | |
| ASA physical status | I | 163 | 58.6 |
| II | 108 | 38.8 | |
| III | 7 | 2.5 |
Table 1: Socio-demographic characteristics of elective surgical patients who took general anesthesia at WSUTRH and SCH 2017.
The incidence of difficult mask ventilation (grade III) is higher in males, ASA physical status class II and within age group 41-60. Impossible mask ventilation (grade IV) was occurred within age group 41-60 and the patient was female with ASA physical status class II. Highest percent of mask ventilation grade II was occurred in male patients, within age ≥ 60 years and by ASA physical status class III (Table 2).
| Variable | Category | Frequency | Mask ventilation n (%) | |||
|---|---|---|---|---|---|---|
| Grade | ||||||
| I | II | III | IV | |||
| Sex | M | 101 | 89 (88.1) | 9 (8.9) | 3 (13) | - |
| F | 177 | 164 (92.7) | 9 (5.1) | 3 (1.7) | 1 (0.6) | |
| Age group | 18-40 | 160 | 153 (95.6) | 4 (2.5) | 3 (1.9) | - |
| 41-60 | 111 | 97 (87.4) | 10 (9) | 3 (2.7) | 1 (0.9) | |
| ≥ 60 | 7 | 3 (42.9) | 4 (57.1) | - | - | |
| ASA physical status | I | 163 | 152 (93.3) | 10 (6.1) | 1 (0.6) | - |
| II | 108 | 97 (89.6) | 5 (4.6) | 5 (4.6) | 1 (0.9) | |
| III | 7 | 4 (57.1) | 3 (42.9) | - | - | |
Table 2: Socio-demographic characteristics and distribution of mask ventilation in elective surgical patients who took general anesthesia at WSUTRH and SCH 2017.
Predictive values of anatomical parameters for difficult mask ventilation
The incidence of difficult mask ventilation was 6(2.2%). Incidence of grade I and II were 91 %( 253) and 6.5 %( 18) respectively (Table 3).
| Parameter | Category | Frequency n (%) | Mask ventilation n (%) | |||
|---|---|---|---|---|---|---|
| Grade | ||||||
| I | II | III | IV | |||
| IID | ˂3 cm | 1(0.4) | - | 1 (100) | - | - |
| ≥ 3 cm | 277 (99.6) | 253 (91.3) | 17 (6.1) | 6 (2.2) | 1(.4) | |
| OSA | Present | 3 (1.1) | - | 1 (33.3) | 2 (66.7) | - |
| Absent | 275 (98.9) | 253 (92) | 17 (6.2) | 4 (1.5) | 1 (.4) | |
| Old Age | ≤ 55years | 268 (96.4) | 250 (93.3) | 11 (4.1) | 6 (2.2) | 1 (.4) |
| ˃55years | 10 (4.6) | 3 (30) | 7 (70) | - | - | |
| KS | Present | - | - | - | - | - |
| Absent | 278 (100) | 253 (91) | 18 (6.5) | 6 (2.2) | 1 (.4) | |
| NM | FM | 277 (99.6) | 253 (91.3) | 17 (6.1) | 6 (2.2) | 1 (.4) |
| Limited | 1 (0.4) | - | 1 (100) | - | - | |
| NC | ≤ 40cm | 274 (98.6) | 253(92.3) | 17 (6.2) | 4 (1.5) | - |
| ˃40 cm | 4 (1.4) | - | 1 (25) | 2 (50) | 1 (25) | |
| Dentition | Lost | 1 (0.4) | - | 1 (100) | - | - |
| Not lost | 277 (99.6) | 253 (91.3) | 17 (6.1) | 6 (2.2) | 1 (.4) | |
| HOS | W | 5 (1.8) | - | 2 (40) | 2 (40) | 1 (20) |
| NW | 273 (98.2) | 253 (92.7) | 16 (5.9) | 4 (1.5) | - | |
| BMI | ≤ 26 kg/m2 | 275 (98.9) | 253 (92) | 18 (6.5) | 4 (1.5) | - |
| ˃26 kg/m2 | 3 (1.1) | - | - | 2 (66.7) | 1 (33.3) | |
| SMD | ˂12 cm | 4 (1.4) | 1 (25) | 2 (50) | - | 1 (25) |
| ≥ 12 cm | 274 (98.6) | 252 (92) | 16 (5.8) | 6 (2.2) | - | |
| TMD | ˂6 cm | 3 (1.1) | - | 2 (66.7) | - | 1 (33.3) |
| ≥ 6cm | 275 (98.9) | 253 (92) | 16 (5.8) | 6 (2.2) | - | |
| MP | A | 270 (97.1) | 253 (93.7) | 13 (4.8) | 3 (1.1) | 1 (.4) |
| B | 5 (1.8) | - | 4 (80) | 1 (20) | - | |
| C | 3 (1.1) | - | 1 (33.3) | 2 (66.7) | - | |
| MMC | I | 261 (93.5) | 244 (93.3) | 13 (5) | 3 (1.1) | 1 (.4) |
| II | 10 (3.6) | 9 (90) | 1 (10) | - | - | |
| III | 7 (2.9) | - | 4 (57.1) | 3 (42.9) | - | |
| BMI: Body Mass Index; HOS: History of Snoring; IID: Inter Incisor Distance; KS: kyphoscoliosis; MMC: Modified Mallampatti Class; MP: Mandibular Protrusion; NC: Neck Circumference; NM: Neck Mobility; OSA: Obstructive Sleep Apnea; SMD: Sternomental Distance; TMD: Thyromental Distance | ||||||
Table 3: Anatomical parameters and their distribution with mask ventilation among elective surgical patients who took general anesthesia at WSUTRH and SCH 2017.
The highest percent of grade III DMV was occurred in patients with OSA, BMI ˃26 kg/m2, Mandibular protrusion class C followed by Neck cercumfrence˃40 cm, history of snoring, Modified Mallampatti Class (MMC) III and Mandibular protrusion class B. Impossible mask ventilation (Grade IV) was occurred in patients with Neck cercumfrence˃40cm, history of snoring, BMI˃26 kg/m2, TMD˂6 cm, SMD˂12 cm. IID˂3 cm, old age˃55 years, Kyphoscoliosis, limited neck mobility and lost dentition have no relation with DMV or IMV. Highest percent of mask ventilation grade II was occurred in patients with IID<3 cm, Limited neck mobility and lost dentition followed by Mandibular Protrusion (MP) class B, old age>55 years and TMD<6 cm (Table 3).
All of the anatomical parameters showed highest specificity and negative predictive value for difficult mask ventilation. MMC class III &IV and Mandibular protrusion class B and C followed by OSA, neck circumference˃40 cm, history of snoring and BMI ≥ 26 kg/m2 showed highest accuracy, sensitivity and positive predictive value to predict difficult mask ventilation grade (III). Anatomical parameters (IID˂3 cm, TMD˂6 cm, SMD˂12 cm, lost dentition, limited neck mobility and old age˃55years) showed 0 sensitivity and PPV to predict DMV (grade III) (Table 4).
| Parameter | Sn % | Sp% | PPV% | NPV% | Area | Accuracy% |
|---|---|---|---|---|---|---|
| Inter incisor distance | 0 | 99.6 | 0 | 97.8 | 0.498 | 49.8 |
| TMD | 0 | 98.9 | 0 | 97.8 | 0.494 | 49.4 |
| SMD | 0 | 98.5 | 0 | 97.8 | 0.493 | 49.3 |
| BMI | 33.3 | 99.6 | 66.7 | 98.5 | 0.665 | 66.5 |
| History of Snoring | 33.3 | 98.9 | 40 | 98.5 | 0.661 | 66.1 |
| Dentition | 0 | 99.6 | 0 | 97.8 | 0.498 | 49.8 |
| Neck circumference | 33.3 | 99.3 | 50 | 98.5 | 0.663 | 66.3 |
| OSA | 33.3 | 99.6 | 66.7 | 98.5 | 0.665 | 66.5 |
| Neck mobility | 0 | 99.6 | 0 | 97.8 | 0.498 | 49.8 |
| Kyphoscholiosis | - | 100 | - | 97.5 | 0.5 | 50 |
| Old Age | 0 | 96.3 | 0 | 97.8 | 0.482 | 48.2 |
| MMC III & IV | 50 | 98.5 | 42.9 | 98.9 | 0.743 | 74.3 |
| Mandibular protrusion B &C | 50 | 98.2 | 37.5 | 98.9 | 0.741 | 74.1 |
| *Sn: Sensitivity; Sp: Specificity; PPV: Positive Predictive Value; NPV: Negative Predictive Value |
||||||
Table 4: Sensitivity, specificity, positive predictive values and negative predictive values for preoperative anatomical parameters against mask ventilation grade III among elective surgical patients who took general anesthesia at WSUTRH and SCH 2017 G.C.
Receiver operating curve
Receiver operating characteristics curve (ROC) above revealed that MMC class III and IV and Mandibular protrusion class B and C, BMI ≥ 26 kg/m2, OSA and above the reference line (0.5) (Figure 1) mask ventilation in the study population.
For more than three decades, poor airway management was recognized as a serious patient safety concern, emphasizing the need for a careful airway assessment and identifying the predictors for a difficult airway [10].
Moreover, the airway risk assessment tools in widespread use were mostly focused on one specific aspect of a difficult airway (i.e. difficult laryngoscopy, difficult intubation). In More recent years, this paradigm has shifted to a more functional approach with greater emphasis placed on the overall importance of the airway patency. Indeed, due to early data demonstrating the significant risk of respiratory depression associated with sedation, The Joint Commission and Centers for Medicare and Medicaid Services has implemented policies to ensure evaluation of the risk for a difficult airway prior to procedures. Moreover, the 2013 American Society of Anesthesiology [11-13] Practice Guidelines for Management of the Difficult Airway caution about the risks of a difficult mask ventilation due to upper airway obstruction and recommend an airway risk assessment before every anesthesia procedure is performed [14].
In our study, we found the incidence of difficult mask ventilation (grade III) as 2.2 % (6/278). There is a wide variation in the reported incidence of DMV in the literature. Whereas one study reported an incidence as low as 0.08%, another reported a 15% incidence. The highest incidence (15%) was reported from a retrospective study of subjects who had difficult intubation. The majority of prospective studies, on the other hand, reported a lower incidence. 0.9% [6], 5% [3] and 7.8% [7]. The large prospective study of 22,660 MV attempts used a DMV grading scale and reported an incidence of 1.4%. Because this is the large and most recent study and because the reported incidence is in agreement with several other studies 1.4% may be considered the most likely estimate in the general population [8].
As we can see from the literature review our result is almost similar to the one which was done on large prospective study of 22,660 even if there is a little difference. So, the probable explanation for this difference result may be because of differences in the population characteristics.
In our study highest percent of DMV was occurred in patients with OSA, BMI ˃26 kg/m2, Mandibular protrusion class C followed by Neck circumference˃ 40 cm, history of snoring, MMC III and Mandibular protrusion class B. We found IID˂3 cm, old age˃55years, Kyphoscoliosis, limited neck mobility and lost dentition have no relation with DMV.
Similarly In a prospective study of 1502 patients, [3] performed a multivariate analysis and found five anatomical risk factors to be significantly associated with DMV and thus may be used as predictors. These were: age older than 55 year, Body Mass Index (BMI) more than 26 kg/m2, lack of teeth, history of snoring, and presence of a beard. The presence of at least two of these factors indicated a high likelihood of DMV. Similarly, an analysis by [7] found age, weight, history of snoring, male gender, and Mallampatti Class IV to be significantly associated with DMV.
In our study a total of 278 patients were investigated and only one case with impossible mask ventilation (grade IV) was encountered. A study by [8] on 22,660 patients found the rate of grade IV as 0.16% (n=37), while another study by the same researcher identified the rate of grade IV as 0.15% (n=77) in 53,041 patients given mask ventilation [15]. In a study of 576 patients by [7] they stated they did not encounter grade IV MV. When the literature is examined, these studies were completed on very broad patient series and we see the rate of grade IV MV is very low.
In our study, impossible mask ventilation (Grade IV) was occurred in patients with Neck cercumfrence˃40 cm, history of snoring, BMI ˃26 kg/m2, TMD˂6 cm, SMD˂12 cm.
We found IID˂3 cm, old age˃55 years, Kyphoscoliosis, limited neck mobility and lost dentition have no relation with IMV. History of snoring and limited Thyromental distance are risk factors for impossible mask ventilation [16].
Regarding predictive values of anatomical parameters, our study showed that poor sensitivities and positive predictive values but good specificity and negative predictive values for DMV. In this study MMC III & IV, MP class B and C followed by OSA, BMI˃26 kg/m2, NC>40 cm showed higher accuracy, positive predictive value and sensitivity for difficult mask ventilation grade (III). Anatomical parameters (IID˂3 cm, TMD˂6 cm, SMD˂12 cm, lost dentition, limited neck mobility and old age˃55years) showed 0 sensitivity and PPV for DMV (grade III) which was comparable with similar studies performed by [17].
Strength
There was no research done on the predictive values of anatomical parameters and incidence of difficult mask ventilation in our country even in Africa. Therefore, it can help as a baseline data for researchers and stake holders.
Our study was done only on those patients whose age was above 18 years. Those patients whose age below 18 years was excluded from the study.
Modified Mallampatti class III &IV and Mandibular protrusion class B and C are highly accurate parameters with high specificity, negative predictive value, and positive predictive value to predicted difficult mask ventilation (grade III).
Anatomical parameters (IID˂4 cm, TMD˂6 cm, SMD˂12 cm, lost dentition, limited neck mobility and old age˃55years) are not related with DMV (grade III).
The authors declare that they have no competing interests and this research work is sponsored by Addis Ababa University.