Emergency Medicine: Open Access
Open Access
ISSN: 2165-7548
ISSN: 2165-7548
Mini Review - (2016) Volume 6, Issue 1
The care of the critically sick and injured often begins in the Pre-hospital setting; recent studies demonstrate that early diagnosis, within the first three hours of presentation combined with aggressive fluid resuscitation, early antibiotics administration and lactate measurements can improve the outcomes of patients with severe sepsis.
The Pre-hospital Sepsis Project (PSP) is a multifaceted study that aims to improve the out-of-hospital care of patients with sepsis by means of knowledge translation and enhancement of skills. Since 2005, our PSP study group has been researching sepsis in the out-of-hospital environment. In a recent publication our PSP group found that out-of-hospital shock index and respiratory rate are highly predictive of ICU admissions for patients presenting sepsis. The Pre-hospital Sepsis Score (PSS) was developed using this data, with maximum points total of 4 points, incorporating respiratory rate, fever and shock index. The patient population can be stratified based on the PSP-S: 1 point is low risk, 2 points is moderate risk, and 3-4 point is high risk.
The care of the critically sick and injured often begins in the Prehospital setting; recent studies demonstrate that early diagnosis, within the first three hours of presentation combined with aggressive fluid resuscitation, early antibiotics administration and lactate measurements can improve the outcomes of patients with severe sepsis [1,2].
Severe sepsis and septic shock are common and expensive medical emergencies. With an estimated yearly incidence of 751,000 cases (3.0 per 1000 population) in the United States each year, severe sepsis and septic shock are associated with significant mortality and consumption of health care resources with estimated costs of $16.7 billion dollars annually [3,4].
The Systemic Inflammatory Response Syndrome (SIRS) is a proinflammatory state, the term SIRS has routinely been associated with both infectious (sepsis) and noninfectious processes, such as an autoimmune disorder, pancreatitis, vasculitis, thromboembolism, burns, or surgery (Figure 1). Systemic inflammatory response syndrome (SIRS), sepsis, severe sepsis, and septic shock were initially defined in 1991 by a consensus panel convened by the American College of Chest Physicians (ACCP) and Society of Critical Care Medicine (SCCM) [5]. These definitions were reconsidered in 2001 again in 2012 [4,6] (Table 1).
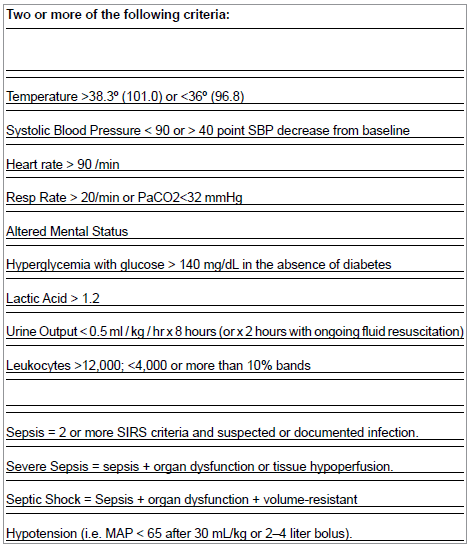
Table 1: Recommended criteria for NOM for children with blunt abdominal trauma.
Sepsis is a clinical syndrome that complicates severe infection. It is characterized by signs of inflammation (vasodilation, elevated white cells, capillary permeability) occurring in tissues that are remote from the infection site. If left untreated this response can lead to Multiple Organ Dysfunction Syndrome (MODS), which is the cause of the high mortality. Early identification and the institution of goal-directed therapies can improve outcomes and mitigate progression to a state of shock and multi-organ dysfunction.
The Sepsis Continuum is the evolution of a complicated untreated infection. Sepsis Continuum definitions include:
Sepsis- Presence (probable or documented) of infection together with SIRS. Severe sepsis — Severe sepsis refers to sepsis-induced tissue hypo perfusion or organ dysfunction with any of the following thought to be due to the infection elevated lactate, or oliguria. Severe Sepsis (Sepsis induced hypotension) is defined as a systolic blood pressure (SBP) <90 mmHg or mean arterial pressure (MAP) <70 mmHg or a SBP decrease >40 mmHg or less than two standard deviations below normal for age in the absence of other causes of hypotension. Septic shock- Septic shock is defined as sepsis-induced hypotension persisting despite adequate fluid resuscitation. Septic shock is a primary vasodilatory or distributive shock that results from a marked reduction in systemic vascular resistance, often associated with an increase in cardiac output.
The Pre-hospital Sepsis Project (PSP) is a multifaceted study that aims to improve the out-of-hospital care of patients with sepsis by means of knowledge translation and enhancement of skills [7-9]. Since 2005, our PSP study group has been researching sepsis in the out-ofhospital environment. One initial study found in 2006 that a poor understanding of the principles of diagnosis and management of sepsis was observed in a cohort of United States Advanced EMS providers, suggesting the need for enhancement of education [7]. Other studies demonstrated that the out-of-hospital shock index and respiratory rate have high predictability for ICU admission [8], whereas recent PSP research has been focusing on the utility of point of care lactate in the Pre-hospital arena [9].
The Pre-hospital Sepsis Score (PSS) was developed based on previous research collected between 2004- 2006. Patients included were adult cases (≥18 years of age) transported by Emergency Medical Services to a major academic center with the diagnosis of sepsis as defined by ICD-9-CM diagnostic codes. Physiologic variables studied included Mean Arterial Pressure (MAP), Heart Rate (HR), Respiratory Rate (RR) and Shock Index (SI). This study demonstrated that out-ofhospital shock index and respiratory rate are highly predictive of ICU admissions for patients presenting sepsis [8].
The PSS has maximum points total of 4 points, incorporating respiratory rate, fever and shock index, defined as the quotient of the heart rate divided by the systolic blood pressure; normally approximately 0.5, but in shock (e.g., rising pulse rate with falling blood pressure), the index may reach 1.0, for example a Systolic of 80 mm Hg combined with a Heart Rate of 125 yields a Shock Index of 1.6.
For the purposes of our Pre-hospital Sepsis Score, we defined fever as core body temperature of ≥ 38°C/100.4°F and is the only obligate variable allotted with 1 point for the socre. Shock index ≥0.7 is given two points and a respiratory rate ≥22 breaths per minute (BPM) is given one point for a total maximum score of 4 points. The patient population can be stratified based on the PSP-S: 1 point is low risk, 2 points is moderate risk, and 3-4 point is high risk (Table 2).
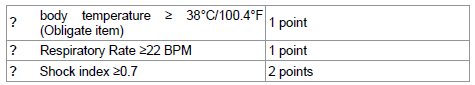
Table 2: The Prehospital Sepsis Score.
In a landmark 2001 study Rivers et al. [10] demonstrated that aggressive resuscitation and early goal-directed therapy (EGDT) of patients with severe sepsis or septic shock resulted in an absolute mortality reduction of 16%, an effective reduction in the incidence of multi-organ dysfunction, and a decline in the use of health care resources. Since then several studies have looked at the value of aggressive simple interventions such as early identification and fluid resuscitation in the first three hours of care of the patient with sepsis syndromes [1,2]. The surviving sepsis campaign guidelines recommends a “three hour bundle” that includes early identification, early antibiotics, lactate measurement and fluids resuscitation [4]. Elements of this “early” bundle are amenable to initiation in the Pre-hospital setting, thus we believe that implementation of early identification by means of our Pre-hospital Sepsis Score, integrated with aggressive Pre-hospital fluid resuscitation and even perhaps point of care lactate [11-14] can lead to earlier, more aggressive resuscitative care and the potential to positively affect outcomes.
Although care of the sick and injured often begins in the Prehospital setting, there is limited data available related to predictors and interventions specific to sepsis in the Pre-hospital work environment? Knowledge of sepsis is relevant to the EMS provider, as the Pre-hospital team has first contact with the patient. Improved recognition of severe sepsis would allow the EMS team to appreciate the patients’ acuity, and presumably, lead to a more informed decision, but also would allow for improved communication between the crew and medical control or the receiving facility as well as initiation of important resuscitative interventional that can benefit the critical care continuum.
Analogous to Pre-hospital alert protocols for trauma, stroke, or patients with myocardial infarctions, improved recognition of sepsis and early notification may not only decrease time to treatment, but also may allow for advance notice to be provided to the receiving Emergency Department. As sepsis has been increasingly recognized by the medical community as an illness that requires immediate treatment and a large amount of resources, advance notification from EMS providers that they are transporting a septic patient may allow the receiving hospital to prepare for their arrival.
Our Pre-hospital Sepsis Project Study group has looked at the Critical Care Continuum in Sepsis [7-9]. In this particular paper we believe that there is potential for implementation of an early warning system for sepsis that integrates the Pre-hospital Sepsis Project Score potentially assisting EMS in notifying hospitals and making point of entry decisions. Further studies should include cost-effectiveness analysis well as a prospective methods validation of this integrated clinical decision scheme and perhaps the utility of Pre-hospital point of care lactate measurements.