Journal of Psychology & Psychotherapy
Open Access
ISSN: 2161-0487
ISSN: 2161-0487
Research Article - (2016) Volume 6, Issue 3
This survey describes the data of 60 adults in treatment for a mental health problem, referring to three
parameters: attachment, alexithymia and metacognitive functions. In order to investigate the relationship between the psychological features mentioned above in patients with Emotional Disorders, they have been grouped into the three Clusters operationally defined in DSM-5: Cluster A (the “odd, eccentric” Cluster), Cluster B (the “dramatic, emotional, erratic” Cluster), and Cluster C (the “anxious, fearful” Cluster).
We conducted a two-step analysis: firstly, a preliminary exploratory analysis based on non-parametric tests; then, in order to investigate the structure of the relationship among the instrumental variables, we applied Spearman’s rho correlation for each cluster.
As we expected, patients with Cluster C Personality Disorder score lower rates of disorganized attachment (lower levels of anxiety attachment and avoidance attachment), lower levels in emotional dysregulation (Alexithymia), and a little higher levels in metacognitive functioning than the other two groups (Cluster A and B). Furthermore, there is a relationship between attachment styles and some specific typologies of disorders: indeed, while preoccupied attachment seems to be a specific feature of patients with Cluster C personality disorders, most of Cluster A and B patients showing the most dysfunctional pattern, the Fearful Avoidant attachment. Finally, Spearman’s rho correlation indicates statistically significant correlations in patients with Cluster A personality disorders between the inability to identify and describe emotions and the ability to understand others’ Emotional States.
Keywords: Adult attachment styles; Emotional Dysregulation; Metacognitive functions; Personality disorders
Personality disorders are a class of mental disorders characterized by enduring maladaptive patterns of behaviour, cognition, and inner experience associated with significant distress or disability [1]. The patients with personality disorders show mental rigidity. They see themselves free of all responsibility for the problems. It means they do not assume responsibility for their own actions and decisions. Indeed, another person seems to be responsible for the internal or external conflicts. In other words, symptoms are ego-syntonic and these characteristics are so deep-seated that are very difficult to change. Although their life stories are recognized as crucial windows into their personality, personality disorders seem to show common patterns: disorders negatively affect a person’s behaviors, influence the interpersonal relations and reduce the abilities of representing emotions and mental events [2-5].
Metacognitive impairment is crucial to explaining difficulties in life tasks of patients with personality disorders and leads to resistance in psychotherapy [3,4,6,7]. Different studies, conducted by the 3rd Center of Cognitive Psychotherapy in Rome, demonstrated that patients with personality disorders have metacognitive deficits and that there are differences in metacognitive processing across these patients. For example, some patients with personality disorders find it difficult to describe their emotions, while others are less able to distinguish fantasy from reality. Many studies have provided strong evidence for a link among metacognition and psychopathology. More specifically, they payed attention to metacognition as an important factor in mental health [5,6,8], because it allows the patients to perceive themselves as intentional agents [9] and monitor feelings [4]. Furthermore, metacognition includes important constructs such as:
- The theory of mind, or ToM [10,11],
- The romantic attachment [7,13-18],
- The emotive expression [19,20],
- The social cognition [21].
Early attachment experiences have a significant formative influence on romantic attachment [16,17,22], as well as facilitating the development of metacognitive functions [23-27].
Bowlby’s [16,17] attachment theory is a useful framework for understanding how early adverse experiences influence later emotional and behavioural development. According to Bowlby, proximity seeking of the attachment figure in the face of threat is the “set-goal” of the attachment behavioural system. Early experiences with caregivers gradually give rise to a system of thoughts, memories, beliefs, expectations, emotions, and behaviours about the self and others. As children develop in line with environmental and developmental changes, they incorporate the capacity to reflect and communicate about past and future attachment relationships. According to Bowlby’s attachment theory, Hazan and Shaver [28] classified adults into these attachment styles: secure, dismissing, preoccupied, and fearful. Later, Collins and Read [23] assumed a precise relationship between adult attachment styles and metacognitive functioning [24-27]. To determine the relationship between attachment style and metacognition, Kobak and Hazan [29] assumed that Internal Working Models (IWM) represented a flexible basis for developing adult attachment style. The internal working model is a cognitive framework comprising mental representations for understanding the world, self and others. Furthermore, adult attachment styles play a role in the process of partner selection, allowing the ability to build trusting relationships. Secure attachment is a healthy attachment style that enables individuals to work autonomously, as well as with others when appropriate. Secure attachments - characterized by internal regulatory mechanisms - allow individuals to be flexible and constructive in their interpersonal relationships, learning about when and where it is appropriate to use metacognitive functioning.
Furthermore, traumatic events could interfere with a child’s normal growth and development, damaging the ability in identifying and verbalizing feelings, including external-oriented thinking [18,30,31]. Indeed, ethological theories have identified alexithymia a result of environmental influences, which is a defense mechanism against experiences perceived too severe and traumatic. If the primary caregivers are insufficiently empathic or responsive due to internal predisposition (for example, low frustration tolerance) or external circumstances (for example, long-term illness), this may result in impaired development of the regulation and expression of affects [18].
In order to investigate the relationships between attachment styles, emotional dysregulation, and metacognition in patients with personality disorders, Alaimo and Cascio [32] compare the results of 120 adults, recruited during cognitive-behavioural therapy in ISPEM (Caltanissetta). The control group (male, n=35; female, n=25) was formed of 60 adults without mental health problems (mean=30,07; st. dev.=14,09). Instead, the experimental group (male=35; female=25) was formed of 60 patients with personality disorders (mean=31,88; st. dev.=12,21). Psychological testing and psychological interview have been used as a baseline measure. Evaluation has been conducted by three therapist (or mental health professionals) expert in mental health treatment. The most important aspects of the first survey (2015) included:
- Marked differences between the experimental and control group in investigated features. More specifically, patients with personality disorders (experimental group, insecure attachment) scored higher levels in emotional dysregulation (Alexithymia) and lower levels in metacognitive functioning;
- A negative correlation between Alexithymia (emotional dysregulation as facial imitation, mentalization, empathy, and internal working models-of-self and others) and metacognitive functioning in both groups. Furthermore, the correlation was statistically significant (,716** in the control group; ,639** in the experimental group).
As we expected, patients with personality disorders in the experimental group experienced anxiety and avoidance more than the control group [6]. At the same time, according to the literature in this field [2,6], the experimental group scored higher levels in emotional dysregulation and lower levels in metacognitive functions [32].
The aim of this survey was to examine in depth the performance of the experimental group (patients with personality disorders). Indeed, they have been grouped into the three Clusters operationally defined in DSM-5 [1], as follows:
Cluster A
–– Paranoid personality disorder, characterized by a pattern of irrational suspicion and mistrust of others, interpreting motivations as malevolent
–– Schizoid personality disorder, characterized by a lack of interest and detachment from social relationships, apathy, and restricted emotional expression
–– Schizotypal personality disorder, characterized by a pattern of extreme discomfort interacting socially, and distorted cognitions and perceptions
Cluster B
- Borderline personality disorder, characterized by extreme “black and white” thinking, instability in relationships, self-image, identity and behaviour often leading to self-harm and impulsivity
- Narcissistic personality disorder, characterized by a pattern of grandiosity, need for admiration, and a lack of empathy
- Histrionic personality disorder, characterized by a pervasive attention-seeking behaviour including inappropriately seductive behaviour and shallow or exaggerated emotions
- Antisocial personality disorder, characterized by a pervasive disregard for the law and the rights of others
Cluster C
- Avoidant personality disorder, characterized by pervasive Feelings of social inhibition and inadequacy, extreme sensitivity to negative evaluation
- Dependent personality disorder, characterized by pervasive psychological need to be cared of by other people
- Obsessive-compulsive personality disorder, characterized by rigid conformity to rules, perfectionism, and control to the point of satisfaction and exclusion of leisurely activities and friendships
As the literature has widely demonstrated [2,3,5,8,33,34], personality disorders have different expression patterns, regardless of the Clusters. Considering that patients with personality disorders experience several relationship problems (such as adult attachment and emotional dysregulation) and that this is largely due to deficits in metacognition, we assume that there are group differences in Cluster A, B, and C’s performance.
Instruments
Psychological testing and psychological interview were used as a baseline measure for carrying out the difference between the healthy group and the patients with personality disorders [32]. Assessments was conducted by a competent team of therapists, exactly three mental illness experts, which were agree in evaluating the mental health disease. The general approach in cases of doubt has been to exclude the cases (problem of comorbidities). Then, participants were invited to complete the following tests:
- Experiences in Close Relationships Inventory, ECR Brennan et al. which is a self-report questionnaire composed of 36 items rated on a 7-point Likert scale (whereby 1=strongly disagree and 7=strongly agree). It defines the adult attachment styles [35], as detailed below: secure style of attachment= “1”, the preoccupied style of attachment= “2”, dismissive avoidant style of attachment= “3”, fearful avoidant style of attachment= “4”. Previous studies demonstrated that ECR has high reliability: Cronbach’ α of 0.93 for the Anxiety scale and 0.95 for the Avoidance scale [36].
For this survey, researchers have adopted the Italian version of Picardi, Vermigli, Toni, D’Amico, Bitetti, and Pasquini (2002), which has a good internal consistency (Cronbach’s α=0.89 for each scale).
- Toronto Alexithymia 20-item (TAS-20) scale [30,31], which is a self-report questionnaire composed of 20 items rated on a 5-point Likert scale (whereby 1=strongly disagree and 5=strongly agree). The total score therefore ranges from 1 to 100. This test defines the ability to identify and describe emotions, as follows: high alexithymia= “2”, alexithymia= “1”, non-alexithymia= “0”. The TAS-20 uses cutoff scoring: equal to or less than 51=non-alexithymia, equal to or greater than 61=alexithymia. Scores between 52 to 60=possible alexithymia.
Furthermore, the TAS-20 has three subscales, congruent with the alexithymia construct: Difficulty Identifying Feelings (DDI), Difficulty Describing Feelings (DDE), and Externally-Oriented Thinking (POE). The instrument has a good internal consistency (Cronbach’s α=0.81) and adequate levels of convergent and concurrent validity.
Metacognitive Functions Screening Scale, MFSS-30 [2], which is a self-report questionnaire composed of 30 items rated on a 4-point Likert scale (whereby 0=strongly disagree and 3=strongly agree). The total MFSS-30 score is the sum of responses. Furthermore, the MFSS-30 provides 4 sub-scales: CRE, as the ability to understand others’ Emotional States; CRC, as the ability to understand Causal Relationships; CDD, as the ability to Judge the Distance of objects from one another and from ourselves; CDP, as the ability to Ponder Situations and Problems. MFSS-30 has a good internal consistency (Cronbach’s alpha=0.88) and adequate levels of convergent and concurrent validity. Furthermore, Cronbach’s α for the coefficients of subscale ranges from 0.70 to 0.79 [2]. For further information on MFSS-30, visit the web site http://www.stateofmind.it/2014/02/Metacognitive-functionsscreening- scale/
Participants
This survey examined 60 patients with personality disorders, aged 18-65 years old (mean=31.88 years; SD=12.21 years), recruited during cognitive-behavioural therapy in ISPEM (Caltanissetta). Clinical interview and psychological testing have been used as a baseline measure and participants have been grouped into the three Clusters operationally defined in DSM-5 (2013), as follows: Cluster A, 26.67%; Cluster B, 26.67%; Cluster C, 46.67%.
Procedure
The participants were informed about the purpose of the study and they gave their informed consent. The experimental procedure was explained, and they participated in the study by filling out the questionnaires, anonymously and voluntarily, without time restrictions. They were tested individually in a quiet room which was arranged for the experimental procedure. A two-step analysis was conducted: an explorative analysis was first conducted, based on nonparametric tests (useful when there are no assumptions about the population distribution). Then, in order to investigate the structure of the relationship among the instrumental variables, Spearman’s rho was applied. To compare the scores belonging to the different scales and to obtain a unique distribution of values, the following transformation procedure [37] was applied:
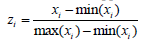
This procedure yelded a new set of scores zi Є (0,1).
Table 1 shows the average and standard deviations of the investigated variables (Experiences in Close Relationships, Alexithymia, and Metacognitive Functions) in patients with personality disorders.
| Personality Disorders | |||||
|---|---|---|---|---|---|
| Cluster A | Cluster B | Cluster C | Total | ||
| Gender (%) | Female | 6 | 4 | 15 | 25 |
| Male | 10 | 12 | 13 | 35 | |
| Age | Average | 32,94 | 35,06 | 29,46 | 31,88 |
| St. Dev. | 13,64 | 12,22 | 11,28 | 12,21 | |
| Experiences in Close Relationships (ECR, total score) | Average | 0,67 | 0,72 | 0,53 | 0,64 |
| St. Dev. | 0,11 | 0,06 | 0,13 | 0,10 | |
| Anxiety (ECR) | Average | 0,63 | 0,78 | 0,56 | 0,65 |
| St. Dev. | 0,16 | 0,09 | 0,12 | 0,12 | |
| Avoidance (ECR) | Average | 0,71 | 0,67 | 0,50 | 0,60 |
| St. Dev. | 0,16 | 0,12 | 0,24 | 0,17 | |
| Alexithymia (TAS-20, total score) | Average | 0,64 | 0,62 | 0,54 | 0,59 |
| St. Dev. | 0,11 | 0,07 | 0,09 | 0,10 | |
| Difficulty Identifying Feelings (DDI) | Average | 0,59 | 0,56 | 0,57 | 0,57 |
| St. Dev. | 0,17 | 0,14 | 0,16 | 0,16 | |
| Difficulty Describing Feelings (DDE) | Average | 0,70 | 0,61 | 0,49 | 0,60 |
| St. Dev. | 0,20 | 0,20 | 0,18 | 0,19 | |
| Externally-Oriented Thinking (POE) | Average | 0,82 | 0,72 | 0,58 | 0,74 |
| St. Dev. | 0,23 | 0,24 | 0,21 | 0,23 | |
| Metacognitive Functions (MFSS-30, total score) | Average | 0,44 | 0,44 | 0,54 | 0,47 |
| St. Dev. | 0,08 | 0,07 | 0,11 | 0,09 | |
| CRE, as the ability to understand others' Emotional States | Average | 0,28 | 0,25 | 0,40 | 0,31 |
| St. Dev. | 0,17 | 0,14 | 0,19 | 0,17 | |
| CRC, as the ability to understand Causal Relationships | Average | 0,44 | 0,44 | 0,54 | 0,47 |
| St. Dev. | 0,20 | 0,17 | 0,19 | 0,19 | |
| CDD, as the ability to Judge the Distance of Objects from one another and from ourselves | Average | 0,50 | 0,54 | 0,60 | 0,55 |
| St. Dev. | 0,12 | 0,09 | 0,12 | 0,11 | |
| CDP, as the ability to Ponder Situations and Problems | Average | 0,57 | 0,53 | 0,60 | 0,57 |
| St. Dev. | 0,16 | 0,17 | 0,17 | 0,17 | |
Table 1: Distribution of subjects by personality disorders.
As we expected, patients with Cluster C personality disorders score lower rates of disorganized attachment (which means lower levels of anxiety and avoidance attachment) and lower levels in emotional dysregulation (Alexithymia), such as in Difficulty Describing Feelings (DDE) and Externally-Oriented Thinking (POE). In addition, they seem to achieve a somewhat higher rate of metacognitive functioning than the other two groups (Cluster A and B), especially in the ability to understand others’ Emotional States (CRE), where Cluster A and B seem to have much lower scores than Cluster C personality disorders.
Furthermore, no securely attached adults are in this survey’s group (Table 2) and most of the patients with Cluster C personality disorders were assigned to “No-Alexithymia” group (Table 3).
| Cluster A % | Cluster B % | Cluster C % | |
|---|---|---|---|
| Secure attachment | 0% | 0% | 0% |
| Dismissing Avoidant attachment | 0% | 0% | 100% |
| Preoccupied attachment | 12,5% | 12,% | 75% |
| Fearful Avoidant attachment | 33% | 33% | 33% |
Table 2: Styles of adult attachment.
| Experiences in Close Relationships | Metacognitive Functions | TAS – 20 total score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anx. | Avoid. | ECR (total score) | CRE | CRC | CDD | CDP | MFSS-30 (total score) | DDI | DDE | POE | TAS – 20 (total score) | |
| Anxiety | - | |||||||||||
| Avoidance | -,117 | - | ||||||||||
| ECR (total score) | ,559 | ,736 | - | |||||||||
| CRE | ,170 | -,662 | -,380 | - | ||||||||
| CRC | ,218 | -,451 | -,200 | ,357 | - | |||||||
| CDD | -,408 | -,367 | -, 555 | -,018 | ,091 | - | ||||||
| CDP | ,086 | -,445 | -,314 | ,182 | -,212 | ,187 | - | |||||
| MFSS-30 (total score) | -,192 | -, 723 | -,668 | ,615 | ,591 | ,580 | ,225 | - | ||||
| DDI | ,105 | -,148 | -,086 | -,178 | ,305 | ,521 | -,083 | ,361 | - | |||
| DDE | ,100 | ,551 | ,472 | -,717 | -,220 | -,228 | -,076 | ,644 | ,010 | - | ||
| POE | ,100 | ,551 | ,472 | -,717 | -,220 | -,228 | -,076 | ,644 | 1.000** | 1.000** | - | |
| TAS – 20 (total score) | ,146 | ,579 | ,545 | -,617 | -,230 | -,156 | -,388 | ,565 | 1.000** | ,768 | ,768 | - |
According to Bonferroni’s method of alpha correlation, results are significant at p<0.00075. Bold results are significant at p<0.000.
Table 3: Spearman’s rho correlation, cluster b personality disorders.
These results give us opportunities to develop an in depth analysis. Considering the relative frequencies of attribute values in each Cluster, patients show significant differences in ECR scores: none of them develops secure attachment, while most show Fearful Avoidant attachment (the most dysfunctional pattern). Indeed, preoccupied attachment seems to be a specific feature of patients with Cluster C personality disorders.
Besides, results indicate that alexithymia scores may change according to the group (Table 4). More specifically, the prevalence rate of alexithymia is significantly higher in Cluster A and B patients (which show the most important difficulty in identifying and describing emotions), than in patients with Cluster C personality disorders.
| Cluster A % |
Cluster B % |
Cluster C % |
|
|---|---|---|---|
| No-Alexithymia | 1% | 1% | 8% |
| Alexithymia | 24% | 24% | 52% |
| High- Alexithymia | 38% | 38% | 24% |
Table 4: Ability to identify and describe emotions.
In order to compare the investigated variable, non-parametric tests (Mann-Whitney U test and Kruskal-Wallis ANOVA test) were used. More specifically, we used the Mann-Whitney U test (known as Wilcoxon Rank sum test) to compare the medians of the two groups (male and female), and the Kruskal–Wallis H test (or One-way ANOVA) for comparing the medians of the three groups (Cluster A, B and C). As we expected, there are significant group differences (Table 5).
| Gender N=60 |
Personality disorders N=60 |
|||
|---|---|---|---|---|
| U | p-value | K-W Anova | p-value | |
| Experiences in Close Relationships (ECR, total score) | 363,000 | ,264 | 23,116 | ,000 |
| Anxiety (ECR) | 368,500 | ,300 | 17,755 | ,000 |
| Avoidance (ECR) | 397,500 | ,547 | 11,833 | ,003 |
| Alexithymia (TAS-20, total score) | 402,500 | ,599 | 10,362 | ,006 |
| Difficulty Identifying Feelings (DDI) | 412,500 | ,707 | ,952 | ,621 |
| Difficulty Describing Feelings (DDE) | 417,000 | ,758 | 11,659 | ,003 |
| Externally-Oriented Thinking (POE) | 417,000 | ,758 | 11,659 | ,003 |
| Metacognitive Functions (MFSS-30, total score) | 418,500 | ,775 | 10,198 | ,006 |
| CRE, as the ability to understand others' Emotional States | 376,500 | ,356 | 8,314 | ,016 |
| CRC, as the ability to understand Causal Relationships | 396,000 | ,532 | 4,180 | ,124 |
| CDD, as the ability to Judge the Distance of Objects from one another and from ourselves | 417,500 | ,763 | 8,392 | ,015 |
| CDP, as the ability to Ponder Situations and Problems | 415,500 | ,738 | 3,024 | ,221 |
According to Bonferroni’s method of alpha correlation, results are significant at p<0.004
Table 5: Results of non-parametric tests (values and significance) on variables for independent groups.
No gender differences were found. Instead, Kruskal-Wallis H test showed that there were statistically significant differences in adult attachment and in emotional dysregulation between groups (Cluster A, B, C).
Post hoc analysis (U-tests) indicated that there was no finding of statistical significance between the pair Cluster A - Cluster B, while there was statistical significance between the Cluster A - Cluster C (Avoidance, p=,002; Anxiety, p=,001; DDE, p=,001; POE, p=,001), and between Cluster B - Cluster C (Anxiety, p=,000; ECR total score, p=,000). Furthermore, patients with Cluster C personality disorders score lower rates of disorganized attachment (lower levels of anxiety attachment and avoidance attachment) than Cluster A and B personality disorders, and lower levels in emotional dysregulation (Alexithymia) than Cluster A personality disorders. According to the most severe forms of PDs, these results could suggest the relationship between adult attachment and the most dysfunctional pattern in individuals with Cluster A and B personality disorders. Indeed, patients with Cluster A and B personality disorders seem to be strongly associated with anxiety disorders and show higher levels in emotional dysregulation. More specifically, patients with Cluster B personality disorders show higher levels in Difficulty Describing Feelings (DDE) and in Externally- Oriented Thinking (POE).
Therefore, in order to investigate the structure of the relationships among the instrumental variables for each group, Spearman’s rho was applied (Tables 3, 6 and 7).
| Experiences in Close Relationships | Metacognitive Functions | TAS – 20 total score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anx. | Avoid. | ECR (total score) | CRE | CRC | CDD | CDP | MFSS-30 (total score) | DDI | DDE | POE | TAS – 20 (total score) | |
| Anxiety | - | |||||||||||
| Avoidance | -,307 | - | ||||||||||
| ECR (total score) | ,848** | ,113 | - | |||||||||
| CRE | -,157 | -,288 | -,274 | - | ||||||||
| CRC | ,487 | ,184 | -,057 | ,043 | - | |||||||
| CDD | ,506 | ,625 | -,050 | ,201 | ,213 | - | ||||||
| CDP | ,067 | -,394 | -,008 | -,181 | ,196 | ,512 | - | |||||
| MFSS-30 (total score) | ,014 | -,379 | -,074 | ,378 | ,604 | ,853** | ,355 | - | ||||
| DDI | ,289 | -,258 | ,163 | -,034 | -,498 | ,175 | ,118 | -,143 | - | |||
| DDE | ,130 | ,406 | ,294 | -,599 | ,260 | -,092 | ,113 | -,326 | ,148 | - | ||
| POE | ,130 | ,406 | ,294 | -,599 | ,260 | ,092 | ,113 | -,326 | ,148 | 1,000** | - | |
| TAS – 20 (total score) | ,294 | ,413 | ,481 | ,803** | -,152 | -,299 | -,086 | -,478 | ,409 | ,627 | ,627 | - |
According to Bonferroni’s method of alpha correlation, results are significant at p<0.00075. Bold results are significant at p<0.000
Table 6: Spearman’s rho correlation, cluster a personality disorders.
| Experiences in Close Relationships | Metacognitive Functions | TAS – 20 total score | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Anx. | Avoid. | ECR (total score) | CRE | CRC | CDD | CDP | MFSS-30 (total score) | DDI | DDE | POE | TAS – 20 (total score) | |
| Anxiety | - | |||||||||||
| Avoidance | -,009 | - | ||||||||||
| ECR (total score) | ,487 | ,822** | - | |||||||||
| CRE | ,074 | -,468 | -,299 | - | ||||||||
| CRC | -,472 | -,459 | -,693 | ,158 | - | |||||||
| CDD | -,147 | -,380 | -,399 | ,376 | ,615 | - | ||||||
| CDP | -,152 | -,283 | ,315 | ,351 | ,616 | ,424 | - | |||||
| MFSS-30 (total score) | -,239 | -,605 | -,604 | ,607 | ,810** | ,811°° | -,310 | - | ||||
| DDI | -,128 | ,515 | ,352 | -,558 | -,430 | -,286 | -,434 | -,565 | - | |||
| DDE | -,109 | ,281 | ,153 | -,453 | ,065 | -,125 | ,177 | -,179 | ,308 | - | ||
| POE | -,109 | ,281 | ,153 | -,453 | ,065 | -,125 | ,177 | -,179 | ,308 | 1,000** | - | |
| TAS – 20 (total score) | ,560 | ,530 | -,606 | ,445 | -,381 | -,310 | -,588 | ,689 | ,461 | ,461 | - | |
According to Bonferroni’s method of alpha correlation, results are significant at p<0.00075. Bold results are significant at p<0.000
Table 7: Spearman’s rho correlation, cluster c personality disorders.
There were no significance in Cluster B (Table 3) and Cluster C (Table 7) personality disorders. Instead, the correlation coefficients shown in Table 6 (Spearman’s rho correlation, Cluster A Personality Disorders) indicated statistically significant bivariate correlations between Alexithymia (TAS -20, total score) and the ability to understand others’ Emotional States (CRE). More specifically, patients with Cluster A personality disorders have difficulty in recognizing emotions (alexithymia) and in emotional awareness. Indeed, these features seem to be positively related.
Personality disorders (PDs) are chronic conditions, which emerge in late adolescence, and typically carry pervasive implications for selfand/ or interpersonal functioning [1]. Indeed, people with personality disorders exhibit characteristics, such as emotional response patterns, which can become problematic and can compromise close relationships [2,3,32,38]. Furthermore, the ability to develop reflective thinking abilities and interact the one’s inner world, require a conscious effort to think about one’s own experiences and improve interpersonal relationships [5,6,39].
This research paper (based on the observation that, in comparison to the normative values, patients with personality disorders reach different scores than patients without personality disorders) refers to three psychological features, or parameters: attachment, alexithymia and metacognitive function [32].
The aim was to examine in depth the performance of patients with Personality Disorders (PD), analyzing the responses of 60 patients with personality disorders, grouped into the three Clusters (Cluster A, B and C).
The results of this survey seem to underline differences between the groups (Cluster A, B and C). More specifically, the comparison of groups by mean and standard deviation (as shown in Table 1) distinguishes patients with Cluster A and B personality disorders from those of Cluster C. Moreover, patients with Cluster C personality disorders score lower levels in adult attachment (ECR total score and its sub-scales, Anxiety and Avoidance) and in emotional dysregulation (TAS 20, total score). Furthermore, Cluster C patients score a little higher levels in metacognitive functioning.
In particular, the results seem to confirm that Cluster C personality disorders have better adult attachment than the other two groups. Indeed, contrary to our first hypothesis, there are no significant differences in metacognitive processing. It could mean that deficits in these abilities are common in all these patients (regardless of the clustering).
Relating to emotional dysregulation (TAS 20), the highest rate of alexithymia was found in Cluster A and B patients (without differences), while the highest percentage of individuals with no-alexithymia (8%) belongs to Cluster C patients. According to the most severe forms of PDs, it could suggest the relationship between emotional dysregulation and the most dysfunctional pattern in individuals with Cluster A and B personality disorders. Furthermore, post hoc tests confirm these results. According to this, lastly, results indicate that patients with Cluster A personality disorders have difficulty in recognizing emotions (alexithymia) and in emotional awareness. Indeed, in Cluster A correlation there is a statistically significant bivariate correlations between inability to identify and describe emotions in the self (Alexithymia) and the ability to understand others’ Emotional States (CRE).
In sum, beyond statistical significance shown in Table 5, Clusters could be distinguished by the attachment styles (ECR total score and sub-scales’ results). In other words, these results seem to suggest that adult attachment styles play an important role in patients with PDs: indeed, this feature could be considered as a “pathognomonic sign”. Even though the disorganized attachment style seems to be common in patients with PDs, the most dysfunctional patterns are in patients with Cluster A personality disorders (specifically schizotypal personality disorder, characterized by odd or eccentric behaviour) and Cluster B personality disorders (specifically antisocial, borderline, histrionic, and narcissistic personality disorders, characterized by dramatic, emotional or erratic disorders). Instead, patients with Cluster C (characterized by anxious, fearful thinking or behaviour) seem to mainly have Preoccupied Attachment, and lower levels in emotional dysregulation than the other two groups (Cluster A and B).
In accordance with the findings of previous studies [5,6,33,34,38], it could be considered useful to carry out a psychological evaluation of attachment pattern (as a basic overview to the assessment of personality), before starting treatment. This consideration is based on the suggestion that there is a relationship between attachment styles and emotional dysregulation. Furthermore, we suggest improving metacognitive skills in treatment, so that patients can be more aware of this process and improve the selective control of it.
Taking into account these suggestions, this study had some limitations. This occurred because of a low number of participants (not sufficient for obtaining results that can be generalized), and a higher number of patients of Cluster C. Indeed, there is a 20% difference between the groups (Cluster A, 26.67%; Cluster B, 26.67%; Cluster C, 46.67%). Further research could clarify the role of attachment styles in emotional dysregulation, and in metacognitive functioning, by increasing sample size and comparing those results.