International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2020)Volume 8, Issue 6
Background: The pathophysiology of reversible functional scoliosis caused by pelvic obliquity is still widely overlooked. The focus of this retrospective study is to observe the occurrence of myofascial trigger points (MTrPs) in patients with reversible pelvic obliquity causing functional scoliosis and leg length discrepancy (LLD).
Method: A retrospective study of 100 consecutive first-visit patients in a physiatric practice was undertaken. The total number of patients included in the study, 111, was determined so that that the number of participants having a reversible pelvic obliquity, amounted up to 100. A Palpation Meter ® was used to determine the height difference in the iliac crests and scapular angles before and after the aligning manoeuvres instructed to be performed by the patient. The method of establishing pelvic symmetry using patients own muscle strength (Muscle Energy Technique) has been described in authors two previous articles and is here reiterated. The incidence of three known types of functional scoliosis associated with pelvic obliquity was registered: innominate upslip, innominate anterior rotation and torsion of the sacrum. Each of them causes a distinct pattern of functional scoliosis. MTrPs were identified by local muscle palpation, indicated by their referred pain patterns. The MTrPs were treated with dry needling. Only the MTrPs where needling caused a local twitch response or symptomatic pain radiation was registered. Besides, the M. iliopsoas mobility was assessed lying prone
Findings: Eighty-four of them had identifiable MTrPs localized in 36 different muscles. The muscle most frequently harbouring TrPs was the gluteus medius. Moreover, 84 of the 100 had a unilateral shortening of the iliopsoas muscle. This study does not include a follow up. The re-establishment of symmetry during the visit was verified. The fact that the study was implemented by one physician leaves it open to bias. The results have a tentative character calling for further research.
Conclusion: The studies covering reversible pelvic obliquity are still lacking though the condition appears to be quite common among patients suffering from musculoskeletal pain. MTrPs may be considered a major source in producing pain in patients having functional scoliosis. There seems to be a strong correlation between functional scoliosis and occurrence of MTrPs. Functional scoliosis imposes persistent muscle strain that perpetuates TrPs in the paraspinal and associated musculature. Correcting the pelvic obliquity causing LLD and functional scoliosis can contribute to treatment of myofascial pain. Dry needling is widely considered a manageable option in the treatment of MTrPs.
Sacroiliac joint; Scoliosis; Pelvis; Pelvic tilt; Malalignment; Myofascial trigger points; Myofascial pain syndrome; Dry needling
Functional scoliosis is often a result of pelvic obliquity. Pelvic obliquity causes both leg length discrepancy (LLD) and a compensating scoliosis. All three aspects are widely discussed in W Schamberger’s book The Malalignment Syndrome [1]. Schamberger has described the relationship between the asymmetrical alignment of pelvis, trunk, and extremities and asymmetrical weight-bearing patterns, diminished ranges of motion, and increased tension in muscles, tendons, and ligaments. In line with standard literature on manual therapy, he has referred to three possible malalignments of pelvic bones: iliac asymmetry (either rotatory malalignment or upslip); sacral torsion around a diagonal axis; and iliosacral inflare or outflare (medially or laterally rotated ilium). Schamberger has believed that malalignment of pelvis and/or spine is presented in 80% to 90% of total adult population and might be responsible for back pain in 50% to 60% of the cases. Several studies have investigated sacroiliac joint dysfunction, functional scoliosis, and leg length discrepancy as separate entities. However, the possible interdependency of these three conditions has been mostly overlooked. Our three previous articles have studied the three different manifestations of reversible pelvic obliquity. The initial study consisted of 150 neurologic patients of the Helsinki University Central Hospital Department of Neurology referred to physiatrist consultation. Notable was the prevalence of the phenomenon. Of them 87% had a reversible pelvic obliquity [2]. The term reversible in these articles means that all the patients in whom functional scoliosis due to pelvic obliquity could be brought back to symmetry which could be verified during the visit.
The diagnostical criteria concerning the two manifestations of pelvic obliquity causing functional scoliosis and the corresponding muscle energy manoeuvres for re-establishing symmetry in both types of pelvic obliquity are presented in two previous papers [3,4]. Here a summary of their findings is presented. The assessment of three possible pelvic malalignments were added to a usual physiatric examination: The iliac crest levels and inferior scapular angles were measured before and after the self-correcting manoeuvres using a Palpation Meter (PALM®, Performance Attainment Associates, Roseville, MN, USA). The Meter combines a calliper and an inclinometer that produce an estimate using a sine function slide ruler. This instrument has been found to be a valid, reliable, and precise tool to measure scapular position and pelvic crest height difference [5-7]. Diagnostic criteria for functional scoliosis accompanying pelvic obliquity and how symmetry can be re-established:
Iliac asymmetry manifesting as anterior rotation or upslip of the ilium
The practitioner assessed the patients regarding three possible asymmetries: height of iliac crests, the height of scapulae, and anteroposterior position of shoulders. If a difference in the level of iliac crests was observed, for further confirmation, a 12 mm elevation was placed in turn underfoot, and the iliac crest height was compared in both positions. Leg length difference was estimated by the examiner, with the patient lying supine. The examiner placed his thumbs caudal to the medial malleoli and compared the thumbs’ position. Figure 1 is a schematic presentation of anterior rotation and Figure 2 upslip of the ilium. The difference between the findings of both conditions is summarized in Table 1. Figure 3 shows the procedure applied to bring both iliac asymmetries to alignment.
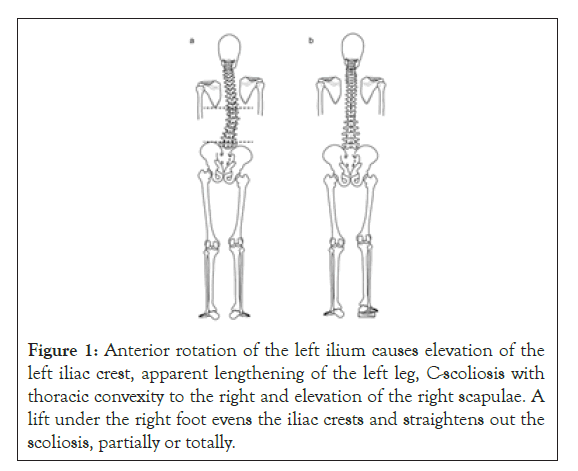
Figure 1: Anterior rotation of the left ilium causes elevation of the left iliac crest, apparent lengthening of the left leg, C-scoliosis with thoracic convexity to the right and elevation of the right scapulae. A lift under the right foot evens the iliac crests and straightens out the scoliosis, partially or totally.
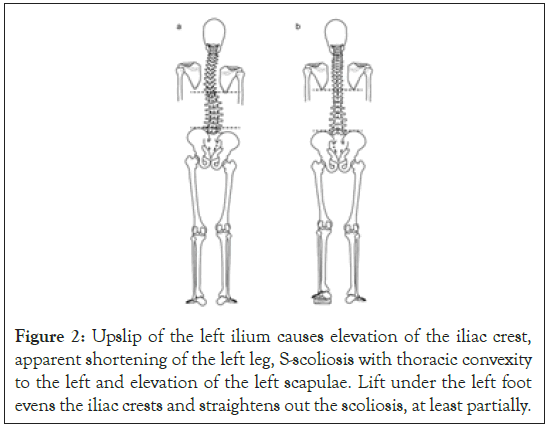
Figure 2: Upslip of the left ilium causes elevation of the iliac crest, apparent shortening of the left leg, S-scoliosis with thoracic convexity to the left and elevation of the left scapulae. Lift under the left foot evens the iliac crests and straightens out the scoliosis, at least partially.
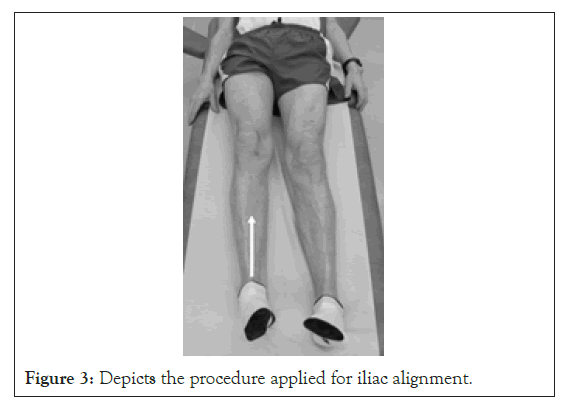
Figure 3: Depicts the procedure applied for iliac alignment.
| Anterior rotation | Up slip | |
|---|---|---|
| Standing with the body weight equally on both feet | Ipsilateral iliac crest and contralateral scapula, higher. Contralateral shoulder, more anterior | Ipsilateral iliac crest and scapulae, higher. Shoulder, more anterior. |
| Standing on a lift (height 12 mm) under the contralateral foot | Iliac crests are even | Contralateral iliac crest elevated |
| Standing on a lift (height 12 mm) under the ipsilateral foot | Ipsilateral iliac crest further elevated | Iliac crests are even |
| Lying in the supine position | Ipsilateral leg longer | Ipsilateral leg shorter |
Table 1: Positional differences between iliac anterior rotation and upslip. It is noteworthy that in anterior rotation, the 12 mm lift under the ipsilateral leg caused the iliac crest to be further elevated, while in upslip, the placement of the lift under the side of the up slip caused the iliac crest to descend to the level of the opposite side.
Diagnostic criteria and re-establishment of symmetry for sacral torsion
After re-establishment of Iliac asymmetry, Iliac crest and scapular angel level was re-assessed using a PALM® tool. Then anteroposterior relationship of inferior sacral lateral angels was compared by palpation. As an indicator of the more ventral angel the palpating thumb sinks deeper on that side. Besides the mutual position of shoulders was assessed. Asymmetry observed in all three points was considered to indicate sacral torsion. See schematic presentation of sacral torsion in Figure 4.
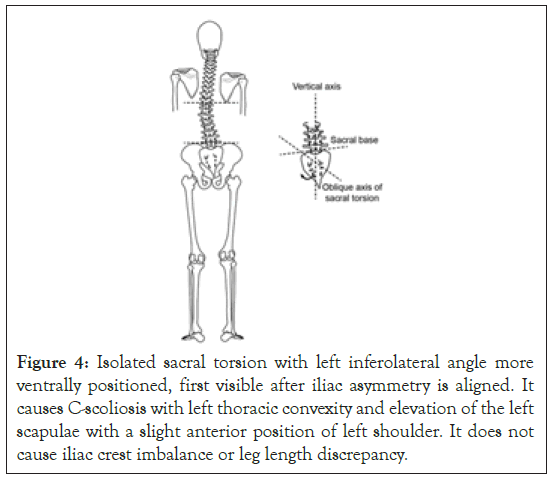
Figure 4: Isolated sacral torsion with left inferolateral angle more ventrally positioned, first visible after iliac asymmetry is aligned. It causes C-scoliosis with left thoracic convexity and elevation of the left scapulae with a slight anterior position of left shoulder. It does not cause iliac crest imbalance or leg length discrepancy.
For the alignment of sacral torsion, patient was instructed to perform a sacrum aligning manoeuvre, mainly involving activation of the gluteus maximus, one side at a time (Figure 5). Subsequently, the height of the scapular angles was measured in up-right position and the anteroposterior relationship of the lateral and inferior sacral angles and shoulders was reassessed. The symmetry of all three aspects indicated the alignment of sacral torsion.
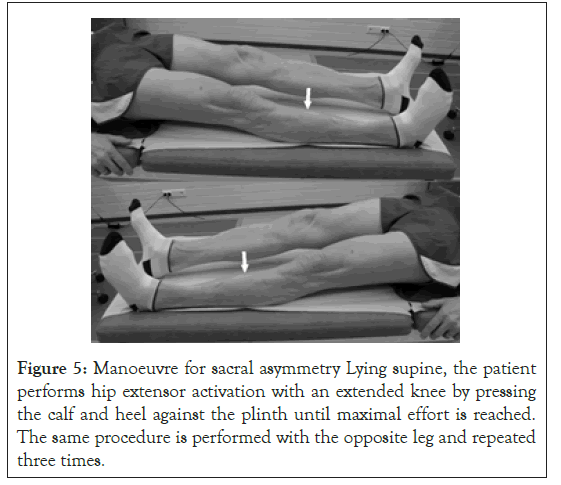
Figure 5: Manoeuvre for sacral asymmetry Lying supine, the patient performs hip extensor activation with an extended knee by pressing the calf and heel against the plinth until maximal effort is reached. The same procedure is performed with the opposite leg and repeated three times.
Both manoeuvres, described above, were performed in a controlled manner to the full range of motion, with maximal strength and without sudden tugging movements. The patients were instructed to continue with the aligning movements; first, once a day and gradually, performing them less frequently. For further demonstration there is a video is available: Timgren J, Self-correcting muscle energy manoeuvres (Video file) (https:// www.youtube.com/watch?v=ZvaHvXKkhY0&t=9s[8].) 2018, June 20 [8].
Trigger points
Although MTrPs have attracted increasing research interest in recent years, their correlation to functional scoliosis has received less attention. This relationship is the focus of the present study. The classic work of Simons and Travell, Myofascial Pain and Dysfunction: The trigger point Manual [9] attributes the pain caused by functional scoliosis to MTrPs but does not take in consideration the reversible nature these three conditions and resorts to the use of shoe lifts for the correction of scoliosis.
Myofascial trigger points (MTrPs) constitute the most common source of pain and they are involved in nearly every pain syndrome, including radiculopathies [10]. Simons et al. defined an MTrP as “a hyperirritable spot, usually within a taut band of skeletal muscle or in the muscle fascia which is painful on compression and can give rise to characteristic referred pain, motor dysfunction, and autonomic phenomena” [9]. This referred pain rarely coincides with dermatologic or neuronal distributions but follows a consistent pattern. Consideration of muscle referred pain patterns assists clinicians in determining which muscles harbour clinically relevant MTrPs. Identifying the pain distribution is one of the most critical elements in identifying and treating myofascial pain. These patterns are illustrated thoroughly in Simons et al. Myofascial Pain and Dysfunction. They highlighted that compensatory scoliosis, i.e., functional scoliosis disposes to trigger points (TrPs): “A lower limb length inequality can cause a tilted pelvis in standing. This usually results in compensatory scoliosis that is maintained by sustained muscular effort, which is a potent perpetuating factor for TrPs in those muscles. Correcting the inequality is often essential for lasting inactivation of TrPs in muscles that are overloaded by the length discrepancy. Occasionally, these perpetuating factors are so important that their elimination permits spontaneous inactivation of the TrPs” [9].
The above authors used shoe lifts for the correction without considering the reversible nature of LLD. MTrPs are tender, prevent full lengthening of the muscle, and may also weaken the muscle. The presence of a local twitch response (LTR), referred pain, or reproduction of the person’s symptomatic pain increases the certainty and specificity of the diagnosis of myofascial pain syndrome (MPS) [11]. A survey of members of the American Pain Society showed general agreement that MTrPs and MPS exist as distinct clinical entities. However, MPS continues to be one of the most commonly missed diagnoses [10]. The focus of this study aimed at evaluating the relationship between MTrPs and functional scoliosis within a given cohort. A strong correlation between the two came forth. However, the question how treatment of functional scoliosis and MTrPs affected the accompanying pain remained outside of the scope of the present study. Our preliminary findings clearly show the need for further research.
In this observational retrospective study, we analyzed 100 consecutive first-visit patients having reversible pelvic asymmetry. They visited a private doctor’s office (a specialist in physiatry) for the first time between November 2018 and June 2019 due to diverse complaints of pain or discomfort.
The total number of patients included in the study, 111, was determined so that that the number of participants having a reversible pelvic obliquity, amounted up to 100. The procedures for diagnostic and treatment of pelvic obliquity were performed as outlined in introduction section.
The patients’ medical records were retrieved for data analysis. The diagnostic and treatment procedures described in the introduction have been incorporated into routine physiatric practice of the author over the past several years as well as the use of dry needling for treating trigger points. No additional examinations or interventions related explicitly to the study were performed. Consequently, an approval from an ethical board was not required.
MTrPs were identified by local palpation of the muscles guided by referred pain patterns according to Simons et al. [9]. The MTrPs suspected of causing referred pain were treated with dry needling. The dry needling technique consists of inserting the needle into the TrP until a first local twitch response (LTR) or radiating pain is obtained. The needle is then moved up and down, without rotation, to obtain further LTRs. Hong showed that when TrP needle penetration produced LTRs, it was much more likely to result in subsequent pain relief than needle penetration that did not elicit LTRs [11]. Only the MTrPs eliciting an LTR and/or pain radiating toward the area of complaint were registered as active MTrPs. Iliopsoas muscle tightness was assessed through comparing passive extension of the hip joint with patient lying prone.
A reversible (small r) pelvic asymmetry was found in 100 out of 111 patients (90%). Patient age ranged from 7 to 83 years, mean age being 48 years. Of the 100 patients 43 were men. Sixty-two patients had an anteriorly rotated ilium; 52 on the left side and ten on the right. Thirty-eight patients had an upslip: 32 on the left and six on the right. Both asymmetries were ass- -ociated with a higher ilium on the affected side. The mean height difference between the iliac crests measured using a PALM ® tool before the aligning manoeuvres was 18.5 mm (range, 10-24 mm). The mean difference in the height of the scapular angles was 11 mm (range, 0-17 mm).
Simultaneous sacral torsion, which was first noticeable after adjusting the ilia, was observed in 98 patients. The mean difference in the scapular elevation was 9.5 mm (range, 6-18 mm). Scapular elevation caused by iliac asymmetry was predominantly found on the same side as the elevation caused by sacral torsion. However, in 31 cases, the scapular elevation caused by the sacral torsion was on the side opposite to that of the initial scapular elevation. After the adjustment of the ilium, the scapular elevation changed sides. This finding explains the initial zero difference in the scapular level in the current cohort, as the two opposing types of scoliosis, one caused by iliac asymmetry and the other by sacral torsion, initially neutralized each other. The main functional features of the three pelvic asymmetries causing functional scoliosis can be summarized in that the iliac upslip shortens the ipsilateral leg, the anterior rotation lengthens the ipsilateral leg, and sacral torsion does not affect leg length.
The self-correcting muscle energy manoeuvres resulted in restoring symmetry in all three forms of pelvic obliquities, which led to aligning of the functional scoliosis. In all cases, the iliac crests, scapulae, and shoulders were even after the aligning manoeuvres. The LLD was equalized without requiring shoe lifts. The change from obliqueness to symmetry and vice versa is an on/off phenomenon without any transitional stages (Figure 6).
Trigger points
Eighty-four patients presented with identifiable MTrPs. TrPs in 36 different muscles were identifies and treated with dry needling. The greatest number of TrPs treated in one patient was six. The ten most common muscles with identified TrPs were the gluteus medius (29 patients) (Figure 6), gluteus minimus (20), quadratus lumborum (19), tensor fascia lata (13), infraspinatus (9), adductor longus (8), pectoralis minor (6), vastus medialis (5), latissimus dorsi (5), and soleus (5).
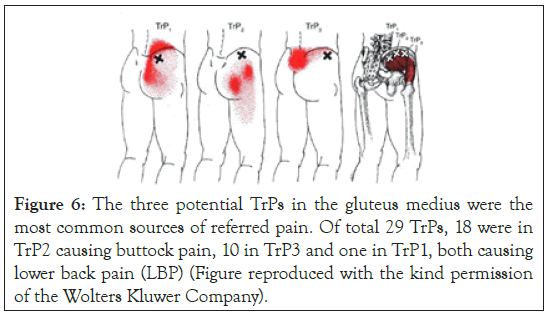
Figure 6: The three potential TrPs in the gluteus medius were the most common sources of referred pain. Of total 29 TrPs, 18 were in TrP2 causing buttock pain, 10 in TrP3 and one in TrP1, both causing lower back pain (LBP) (Figure reproduced with the kind permission of the Wolters Kluwer Company).
Of all the TrPs treated, 52 were localized in the upper and 170 in the lower body. Among the 77 patients presenting with LBP, 65 (84%) had unilateral tightness (tension) of the psoas muscle (84%); all were right sided except for one. Among the 23 patients not presenting with LBP, only 7 (30%) had unilateral psoas tightness. The TrPs in psoas itself cannot be reached with a needle because of its location. In these patients, an active isolated stretching procedure for psoas muscle tightness was taught instead of dry needling (Figure 7).
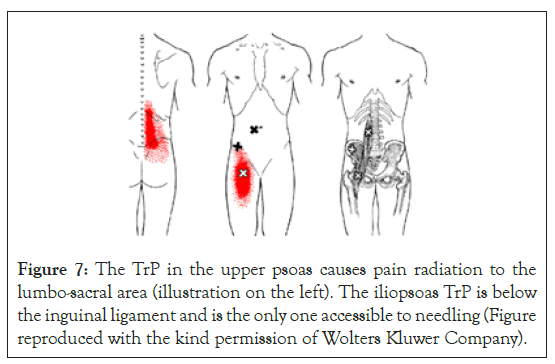
Figure 7: The TrP in the upper psoas causes pain radiation to the lumbo-sacral area (illustration on the left). The iliopsoas TrP is below the inguinal ligament and is the only one accessible to needling (Figure reproduced with the kind permission of Wolters Kluwer Company).
In our patients, pain was regularly associated with existing TrPs. Our finding of the gluteus medius TrPs being most often connected with LBP and buttock pain is parallel with the results obtained by Kameda et al. [12]. They treated 81 LBP patients having TrPs with and/or leg pain using injections or soft tissue release. In their findings the muscle most involved was the gluteus medius. They identified a TrP in the gluteus medius in 40 (49%) patients.
Iliopsoas dysfunction is often portrayed as a contributing factor to LBP, Bachrach et al. [13] defined psoas insufficiency as a major cause of LBP; his findings were analogous with ours: sacroiliac dysfunction with an anteriorly rotated ilium, LLD, mostly rightsided psoas shortening, and MPS. As the cornerstone of treatment, he presents the correction of sacroiliac and other dysfunctions supported by self-management program. Petroutsos [14] further detailed the biomechanics of psoas insufficiency in causing LBP and introduced the term “psoatic lumbar rotoscholiosis.” Both these studies stated that sacroiliac dysfunction was the result of psoas insufficiency; however, we rather hold the view that sacroiliac dysfunction associated with pelvic obliquity is the primary cause of psoas problems.
In our study, the ipsilaterally restricted hip extension due to iliopsoas tightness correlated strongly with the presence of LBP. Ingber [15] observed how palpable tenderness and weakness of the iliopsoas muscle and loss of pain-free hip extension can be correlated with LBP. He treated these patients with dry needling of the iliopsoas TrPs followed by self-administered, post-isometric relaxation exercises. He noted improvement in extension after iliopsoas TrP dry needling with LBP alleviation and concluded that iliopsoas muscular contracture is the likely cause of LBP in patients with a unilateral tight iliopsoas muscle.
According to the available systematic reviews, dry needling should be the first-choice treatment to reduce MTrP pain in the short term [16]. The advantages of dry needling are increasingly documented and include an immediate reduction in local, referred, and widespread pain, restoration of range of motion and muscle activation patterns. A Cochrane review concluded that “dry needling appears to be a useful adjunct to other therapies for chronic low back pain” [17].
Simons et al. [9] emphasize the role of functional scoliosis as a factor disposing to TrPs. “The functional scoliosis due to the short leg and tilted pelvis requires continuous compensatory muscular activity in the upright position, which overloads the paraspinal muscle and can make a critical contribution to musculoskeletal pain. To ensure lasting relief from the myofascial pain it is important to correct the leg length discrepancy which alone may be sufficient to relieve the pain of muscular origin.”
This paper does not include a follow-up of the patients. However, based on personal observation over the past 10 years, the combining TrP dry needling with the restoring of spinal symmetry can contribute to long lasting improvement of myofascial pain. The relapses of pain symptoms were mostly associated with recurring pelvic asymmetry activating the trigger points anew. In all our papers, LLD has been found to be reversible and caused by pelvic obliquity.
The method described in this manuscript permits the treatment of functional scoliosis without shoe lifts or aligning procedures by physical therapists. Further research is needed to confirm our results. The generalization of the study results might be limited by the fact that this was a retrospective study among patients treated by a single physician who also performed all the assessments.
Citation: Timgren J (2020) The Role of Myofascial Trigger Points in the Treatment of Reversible Functional Scoliosis. Int J Phys Med Rehabil. 8:571. DOI: 10.35248/2161-0983.20.8.571
Received: 04-Sep-2020 Accepted: 18-Sep-2020 Published: 25-Sep-2020 , DOI: 10.35248/2329-9096.21.8.571
Copyright: © 2020 Timgren J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.