
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2020)Volume 11, Issue 4
Background and aim of the study: To what extent focused transthoracic echocardiography when done preoperatively to patients admitted for elective surgery and suspected to be at risk of cardiac disease specially the geriatric population can affect perioperative anesthetic management of these patients.
Methods: This study was done at Qena university hospitals and 100 patients were included, >60 years of age who were subjected to preoperative transthoracic echocardiography (TTE) to evaluate hemodynamic state, left and right ventricular functions, systolic and diastolic volumes and pressures, valves diameters and competency, pericardial effusion and pulmonary artery pressure.
Results: Our results showed changes in clinical diagnosis in the form of reporting 26% of patients with impaired ejection fraction of left ventricle, 18% valve lesions, and diastolic dysfunction in 40% of patients. Accordingly 4% of patients were canceled and the anesthetic management was changed in 20% of patients.
Conclusions: preoperative focused TTE can help decision making in perioperative management of old age patients suspected to be at risk of post operative cardiac complications.
Transthoracic echocardiography; Postoperative cardiac complications; Elective surgeries
The anesthetic management of patients scheduled for operative procedures depends on the pre-operative data of the patient regarding the age, weight, sex and type of surgery. The preoperative investigations either laboratory or radiological were done to determine the plan of anesthesia and strategy of postoperative pain control [1]. For some reasons or other, complete investigation of the patient may be insufficient for accurate evaluation of co-morbid conditions such as cardiovascular diseases which commonly represent the most common postoperative complications. The detection of comorbid condition is common in day-case surgeries for which there should be rapid and effective intervention in collaboration with cardiologist or other specialty according to the condition of the patient [2].The presence of pre-operative anesthesia clinic can help in evaluation and preparation of the patient to avoid sequels of undiscovered coexisting cardiac disease [3].
Moreover clinical examination may not be sufficient to evaluate the patient specially if the patient is not able to co-operate with the examining physician such as if there is broken leg or forearm or obese patient or pediatric patients, so many signs may be missed during clinical examination which if discovered can change the anesthesia plan of the patient [4].Transthoracic echocardiography (TTE) is a relatively new tool of investigation that non-invasively can assess the state of the heart and great vessels. During clinical examination, the detection of a murmur can be further evaluated by the TTE to determine the pathology of the valve responsible for that murmur and to confirm whether the dyspnea suffered by the patient is of cardiac of pulmonary cause [5-7].
TTE can also evaluate left ventricular function, left ventricular hypertrophy and pulmonary blood pressure. Although it does not replace other investigatory tools of assessment of the cardiovascular system, it seems more accurate and informative than clinical assessment alone specially if we know that it is easily performed and that junior anesthesiologist can be trained to do it in short time [8].The aim of this study was to determine the value of pre-operative TTE examination of patients scheduled for surgery in anesthetic plan and post-operative pain relief.
This prospective cohort study was done at Qena university hospitals in the time period from October 2017 to December 2018 on 100 patients above 60 years of age with risk of postoperative cardiac complications scheduled for elective surgical operations. The study protocol was approved by the ethical committee of Qena faculty of medicine and registered at www.clinicaltrials.gov at no.:” NCT04114474. Written informed consent was taken from every patient included in the study. Eligibility for participating in the study was assessed before assignment by the attending physician in the anesthesia clinic. Patients above 60 years of age ASA I and ASA II were included in the study and patients with history of cardiac disease, history of previous postoperative cardiac complications and symptoms or signs of cardiac diseases were excluded from the study. All patients were first assessed in the anesthesia clinic of Qena university hospital by clinical examination and routine investigations regarding detailed history taking including: age, sex, work, previous operations, smoking, diabetes, past history and family history, Clinical Examination of the chest and heart was done and all patients were investigated for complete blood picture, prothrombin concentration/time, INR and ECG.
According to the each type of surgery, the responsible anesthesiologist was asked to write his anesthetic management protocol of the patient in special sheet then TTE (Vivid I echocardiography machine General Electric Healthcare, Milwaukee, WI, USA®) with a 3S-RS (1.5-3.6 MHz) transthoracic probe) was done by professional anesthesiologist following the HEART protocol (Hemodynamic Echocardiography Assessment in Real Time). According to the clinical findings of TTE patients may be either free or have one or more of the following hemodynamic states:
- Left ventricular systolic and diastolic failure,
- Right ventricular failure,
- Valve stenosis or regurgitation of at least moderate severity,
- A pericardial effusion greater than 0.5 cm; or
- Pulmonary hypertension (estimated pulmonary artery systolic pressure >60 mmHg). Non-hemodynamically findings on clinical or TTE examinations such as: mild valvular stenosis, regurgitation, or normal haemodynamic state were not significant.
According to the data found by TTE examination, the anesthesia plan was re- discussed with the responsible anesthesiologist to be compared with the one put in the anesthesia clinic before TTE was performed to record any change in that plan of anesthesia. All modifications of anesthetic management as well as any intra-operative hemodynamic changes were recorded for further analysis. Our primary end point was the detection of different pathology not diagnosed preoperatively and the change of anesthetic management after TTE was done which may necessitate:cardiology consultation, surgery consultation to modify the surgical technique planned to be done, preparation for intensive care bed, fluid management modification.Secondary end points were any post-operative cardiac and non cardiac complications. We performed this study on a hundred patients to facilitate statistical calculation of the results obtained.
In this study there was a significant role of pre-operative focused transthoracic echocardiography in the anesthetic management of patients with risk of post-operative cardiac complications. Summary of flow of patients throughout the study is illustrated in Figure 1. Focused TTE was performed the patient’s bedside before surgery, the focused TTE examinations resulted in change in clinical diagnosis according to Table 1. This finding resulted in a changed patient management in 28 out of 100 patients. The change in management was more frequent (22%) in the group ASA 2; yet even in ASA 1 patients, management was changed in (6%). The change was according to Table 2.
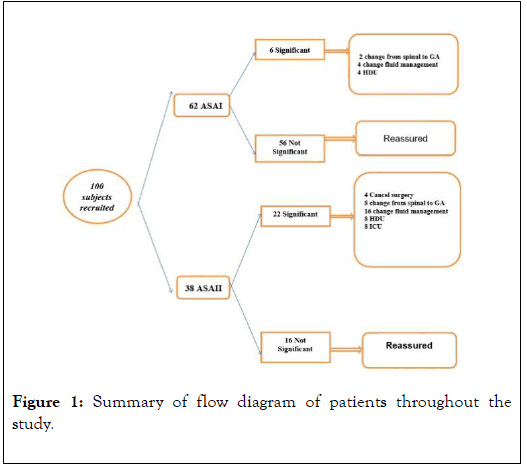
Figure 1. Summary of flow diagram of patients throughout the study.
| Number | Percent % | Valid Percent % | Cumulative Percent % | |
|---|---|---|---|---|
| Normal | 82 | 82 | 82 | 82 |
| mild MS | 4 | 4 | 4 | 86 |
| moderate MS | 4 | 4 | 4 | 90 |
| severe MS | 2 | 2 | 2 | 92 |
| mild AS | 2 | 2 | 2 | 94 |
| moderate AS | 2 | 2 | 2 | 96 |
| severe AS | 2 | 2 | 2 | 98 |
| moderate AR | 2 | 2 | 2 | 100 |
| Total | 100 | 100 | 100 | - |
Table 1: Valve lesions.
| TTE finding | Number |
|---|---|
| impaired EF <55% | 26% |
| Hypokinesia | 24% |
| Valve lesions | 18% |
| Diastolic dysfunction | 40% |
Table 2: Change in clinical diagnosis.
1. Ejection fraction: Of the 100 patients enrolled in the study, 26 patients were with impaired EF >55%
2. Ventricular wall motion: Of the 100 patients enrolled in the study, 24 patients were with hypokinesia
3. Valve lesions: Of the 100 patients enrolled in the study, 18 patients were with valve lesions. mild MS 4%, moderate MS 4%, severe MS 2%, mild AS 2%, moderate AS 2%, severe AS 2% and moderate AR 2%.
4. Diastolic dysfunction: Of the 100 patients enrolled in the study, 40 patients were with DD, 32 of them DDI, 4 of them DDII and 4 of them DDIII
Type of surgery: Surgical specialties included orthopaedic (30), abdominal surgery (20), gynaecological (24), vascular (10) and plastic (16) (Figure 2).
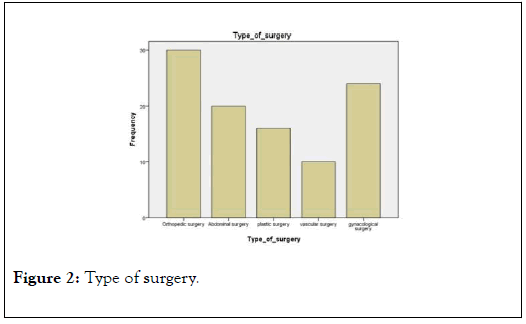
Figure 2. Type of surgery.
Of the 100 patients enrolled in the study, 80 patients were transferred to Standard ward, 12 patients to High dependency unit (intermediate care) and 8 patients need to transferred to Intensive care unit (ICU) (Figure 3).
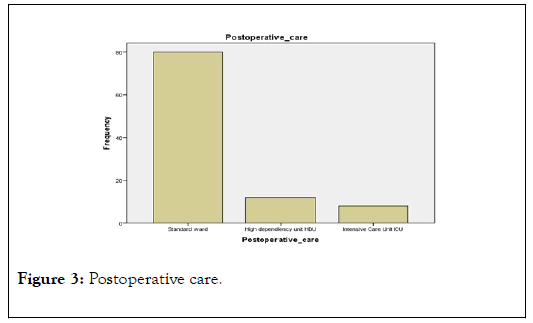
Figure 3. Postoperative care.
100 patients enrolled in the study, 80 patients were transferred to Standard ward, 12 patients to High dependency unit (intermediate care) and 8 patients need to transferred to Intensive care unit (ICU) (Table 3).
| The change in management | Number |
|---|---|
| cancel surgery &refer to cardiology | 4% |
| change fluid manegment | 20% |
| change anaesthetic technique | 10% |
| Postoperative care | 12% tansferred to HDU 8% tansferred to ICU |
Table 3: Change in anesthetic management.
1. Cancel surgery & refer to cardiology: Of the 100 patients enrolled in the study, 4 patients were referred to cardiology department due to severe valve lesion.
2. Change fluid management: Of the 100 patients enrolled in the study, 20 patients were subjected to change fluid management due to hypokinesia or valve lesion.
3. Change anaesthetic technique: Of the 100 patients enrolled in the study, 10 patients were subjected to change anaesthetic technique (e.g from GA to spinal anaesthesia)
4. Postoperative care: Of the 100 patients enrolled in the study, 80 patients were transferred to Standard ward, 12 patients to High dependency unit (intermediate care) and 8 patients need to transferred to Intensive care unit (ICU).
This was a prospective randomized clinical study to determine whether focused TTE changes the anesthetic management of patients with risk of post-operative cardiac complications leading to best possible patient’s outcome.
Pre-operative non-invasive testing aims to provide information on three cardiac risk markers: LV dysfunction, myocardial ischemia and heart valve abnormalities, all of which are major determinants of adverse post-operative outcome. LV function is assessed at rest and various imaging methods are available. For detection of myocardial ischemia, exercise ECG and non-invasive imaging techniques may be used [9]. The reason why in this study we used TTE because that a previous study concluded that, senior cardiologists fail to detect 10-20% of murmurs, and no physical examination finding has been identified that has both a high sensitivity and a high specificity for the diagnosis of severe aortic stenosis in asymptomatic subjects [10]. Also echocardiography is the only practical investigation available for confirmation of the diagnosis of right ventricular failure, and is accurate for the evaluation of pulmonary hypertension [11]. The echocardiographic findings allowed the anaesthetist to triage patients into low- and high-risk categories, thereby helping them to devise what they felt to be an appropriate management plan before surgery.
When a clinically important haemodynamic or valvular abnormality was detected on TTE, the effect was to alert the anaesthetist to increased cardiac risk. On the other hand, a clinically unimportant finding or normal TTE had the effect of reassuring the anesthetist, leading to a reduced requirement for further investigation, invasive peri-operative monitoring and increased dependency postoperative care [12].
In our study there was a significant role of pre-operative focused transthoracic echocardiography in the anesthetic management of patients with risk of post-operative cardiac complications. In agreement with our study many studies have shown the impact of focused echocardiography on clinical diagnosis and changes in patient management. Canty and Royse show the impact of focused echocardiography on clinical diagnosis. The change in diagnosis due to detection of clinically significant cardiac pathology was reported about 51% [13].
In another study (Canty et al.2012), The change in diagnosis due to detection of clinically significant cardiac pathology was reported about 67% and in (Cowie 2011) study changes in patient management were 82% [14,15].The diagnostic impact appeared greater in studies where focused echocardiography was performed in patients with a recognized indication for focused echocardiography (a change in diagnosis was made in between 51% and 67% of cases) [16] and the impact on management also appeared greater in the studies where focused echocardiography was performed for a recognized indication (between 54% and 82%)
Confirming our study one study (Botker et al. 2014) where focused echocardiography was used as a routine screening tool in which a diagnosis was only changed in 17% of patients and changes in anesthesia was only in 12% and disclosed in a group of patients above age of 60 years and/or in ASA class ≥ 3 [17].We have shown that focused TTE, performed preoperative by an anesthetist, resulted in a change of management in a high proportion of patients, including in asymptomatic patients.
Transthoracic echocardiography is a common performed preoperative investigation, but the agreement of the exact indications for echocardiography is lacking, and its effect on perioperative decision making has not been previously reported. It may be requested by anaesthetists to identify lesions such as aortic stenosis, pulmonary hypertension, left ventricular hypertrophy, left ventricular dysfunction and mitral regurgitation, in at-risk patients [18-20].
Conventional practice is to refer patients to an outpatient cardiology echocardiography clinic if TTE is required. This may lead to an undesirable delay before surgery. However, if the anesthetists can perform the investigation themselves immediately, delays due to availability and waiting times may be eliminated [21].
The echocardiographic findings allowed the anesthetists to categorize patients into low- and high-risk categories, thereby helping them to choose an appropriate management plan before surgery [22].
When a clinically important hemodynamic or valvular abnormality was detected on TTE, the effect was to alert the anesthetist to increased cardiac risk. On the other hand, a clinically unimportant finding or normal TTE had the effect of reassuring the anesthetist, leading to a reduced requirement for further investigation, invasive peri-operative monitoring and increased dependency postoperative care [23-25].
Limitations of this study include the observational nature of the design; a suitable anesthetic department echocardiography service would need to include a reasonable number of anesthetists suitably trained in focused TTE. There is also the potential for a wide range of anesthetic management decisions to be applied for the same TTE findings. A TTE at rest primarily evaluates functional and anatomical abnormalities, is a poor Discriminator for active coronary artery disease and is not a substitute for pre-operative stress testing. In addition, a normal TTE study does not rule out all possible cardiac pathology and these limitations must be considered when putting together any management plan using TTE data.
Preoperative focused TTE can help decision making in perioperative management of old age patients suspected to be at risk of post operative cardiac complications.
The authors have no sources of funding to declare for this manuscript.
The authors declare no conflicts of interest.
The study was registered at www.clinicaltrials.gov at no. :”NCT04114474”. At 10/15/2019.
Citation: Elatif AFA, Mohamed HS, Ahmed MS, Elzohry AAM (2020) The Role of Pre-Operative Focused Transthoracic Echocardiography in Anesthetic Management of Old Age Patients with Potential Risk of Post-Operative Cardiac Complications. Journal of Anesthesia and Clinical Research 11:946. DOI: 10.35248/2155-6148.20.11.946
Received: 10-Apr-2020 Accepted: 20-Apr-2020 Published: 27-Apr-2020 , DOI: 10.35248/2155-6148.20.11.946
Copyright: © 2020 Elatif AFA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.