Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2023)Volume 8, Issue 6
Allergies in children are a serious health issue that impact a large segment of the global pediatric population. This case study explains into the specifics of a clinical visit with a male patient, age five, who had a complicated allergy profile. Allergen-specific IgE antibodies may confirm allergic sensitization and the medical history of the patients, clinical manifestations, diagnostic methodology, successful immunotherapy, therapeutic measures, and long-term management plans are all covered in the report. This case report will highlight the challenges in identifying and treating allergies in children and highlighting the significance of a multidisciplinary approach to the best possible patient treatment.
Pediatric allergy; Skin prick testing; Subcutaneous allergen immunotherapy; Food allergy
Pediatric allergies encompass a spectrum of immune-mediated hypersensitivity reactions to various environmental allergens. Allergic sensitization usually initiates in a mild form in early childhood, although it can arise at any age. Environmental allergens induce allergen-specific IgE; their presence is often transient and mostly resolves spontaneously. The prevalence of allergies in children has been steadily rising, identifying and necessitating thorough the understanding of the diagnostic and therapeutic purpose associated with this condition. This case report explores the challenges and considerations involved in managing pediatric allergies, using a detailed examination of a 5- year-old male patient with a diverse allergy profile can be studied [1].
A 5-year-old male, referred to as Patient X, presented to the pediatric allergy clinic with a history of recurrent episodes of sneezing, nasal congestion and pruritus. The symptoms were initially noted around the age of 2 and despite intermittent symptomatic relief with over-the-counter antihistamines, the frequency and severity of symptoms had escalated over the past year.
Medical history
Patient X was born at full term via normal vaginal delivery and had an unremarkable neonatal course. His family history revealed atopy, with both parents reporting allergic rhinitis and a maternal aunt diagnosed with asthma [2]. There was no history of exposure to environmental tobacco smoke, pets, or indoor allergens in the patient's home is seen in (Figure 1).
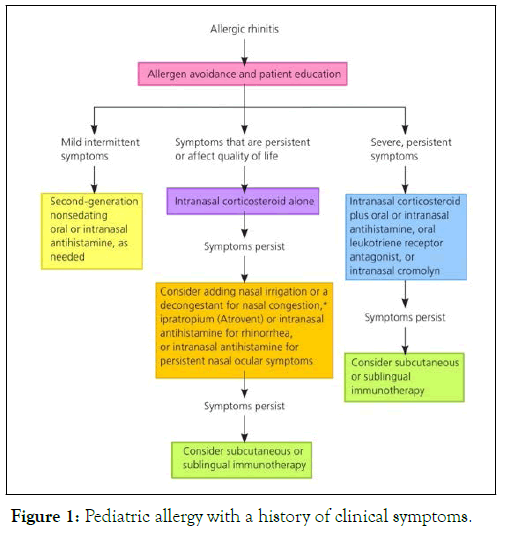
Figure 1: Pediatric allergy with a history of clinical symptoms.
Clinical manifestations
Patient X's primary complaints included sneezing, nasal congestion and pruritus. Secondary symptoms such as watery eyes and occasional coughing were also reported. Symptoms were more pronounced during the spring and fall seasons but persisted to a lesser extent throughout the year. Physical examination revealed bilateral nasal mucosal erythema, mild conjunctival injection and occasional dark circles under the eyes [3-5].
Diagnostic approach
Given the chronicity and escalating nature of symptoms, a systematic diagnostic approach was undertaken. Skin Prick Testing (SPT) was performed to assess sensitivity to common allergens, including pollens, molds, dust mites, and animal dander. Patient X exhibited strong positive reactions to grass pollens, dust mites, and cat dander.
Additionally, serum-specific IgE testing confirmed elevated levels of IgE antibodies against the identified allergens. Pulmonary Function Tests (PFTs) were within normal limits, ruling out concurrent asthma. The diagnosis of allergic rhinitis, with a focus on grass pollen, dust mites and cat dander, was established.
Therapeutic interventions
The management plan for Patient X involved a multifaceted approach, addressing both acute symptomatic relief and longterm control. Intranasal corticosteroids, such as fluticasone, were prescribed for their anti-inflammatory effects on nasal mucosa. Second-generation antihistamines, including cetirizine, were recommended for symptomatic relief, with emphasis on their non-sedating nature [6-8].
Allergen avoidance measures were discussed, including the use of allergen-proof bedding, regular cleaning and minimizing exposure to cats. Immunotherapy, specifically Subcutaneous Allergen Immunotherapy (SCIT), was proposed to modify the natural course of the disease by desensitizing the patient to specific allergens.
Long term management strategies
Patient X's long-term management plan focused on sustained allergen avoidance, regular follow-up evaluations and continuous optimization of pharmacotherapy. The initiation of SCIT was discussed with the parents, addressing potential benefits, risks and the importance of consistent adherence to the treatment regimen [9,10].
Patient education played a pivotal role in empowering the parents with the knowledge and skills required for effective allergen control. Follow-up appointments were scheduled at regular intervals to monitor treatment response, adjust medications and address any emerging concerns.
This case report underscores the complexity of pediatric allergies and the importance of a comprehensive diagnostic and therapeutic approach. The integration of SPT, specific IgE testing and clinical evaluation aids in the accurate identification of allergens triggering symptoms. The emphasis on allergen avoidance measures, pharmacotherapy and immunotherapy aligns with current guidelines for managing allergic rhinitis in pediatric patients.
The incorporation of a multidisciplinary team, including allergists, pediatricians and immunologists, is crucial for providing holistic care to pediatric allergy patients. Additionally, the involvement of parents in the management process is essential, as successful allergen control often relies on a collaborative effort between healthcare providers and caregivers. Pediatric allergies represent a challenging and increasingly prevalent health concern. This case report provides a comprehensive overview of the diagnostic and therapeutic aspects of managing pediatric allergic rhinitis. By examining the case of Patient X, we have highlighted the importance of a systematic approach, involving detailed history-taking, diagnostic testing and a personalized management plan.
As the prevalence of pediatric allergies continues to rise, ongoing research and clinical experience will contribute to refining our understanding of this complex condition. Through a concerted effort from healthcare providers, educators and families, the goal of optimizing outcomes and improving the quality of life for children with allergies can be achieved. Pediatric allergy can be divided into IgE mediated or non- Immunoglobulin E (IgE) mediated allergy: Immediate-type food allergy (IgE mediated), delayed-type food allergy (non IgE mediated) symptoms are caused by IgE antibodies and usually occur within 30 minutes (but certainly within 2 hours) of eating the food.
The standard therapy for Channel Service Unit (CSU) includes second-generation antihistamines, but if symptoms persist despite optimal treatment at maximal dosage, omalizumab should be initiated. Omalizumab is a humanized monoclonal IgG1 antibody that binds to free IgEs and downregulates the expression of FceRI (High-Affinity IgE Receptor), preventing the attachment to high-affinity receptors on mast and dendritic cells. This mechanism avoids cell activation and lowers the release of inflammatory mediators, with the final purpose of alleviating the allergic response. Omalizumab is currently approved for the treatment of CSU in pediatric patients aged 12 years and above. It is administered subcutaneously every month, with the option to increase the dosage if an inadequate response is observed. This monoclonal antibodies most common side effects are local reactions at the injection site and mild headaches. After six months of administration, if symptoms persist, other immunomodulatory drugs, such as oral cyclosporine, can be evaluated. Other biologics explored for treatment-refractory CSU include ligelizumab, dupilumab and benralizumab. Biological therapies, therefore, have emerged as valuable treatment options for pediatric patients with chronic urticaria, particularly for those who do not have a proper response to antihistamine therapy.
Food Allergy (FA) is a potentially life-threatening response driven by the immune system triggered by definite food allergens that affect a significant part of the pediatric population. FA is distinguished into immunoglobulin IgE-mediated, non- IgE-mediated, or mixed types depending on the underlying immune processes. IgE-mediated FA is frequently triggered by certain food such as milk, egg, peanut, wheat, soy and shellfish. As of now, the removal of the allergenic food is the elective approach for managing FA, but allergen-specific Oral Immunotherapy (OIT) has reported increasing effectiveness in inducing immune tolerance to the culprit food. In this context, omalizumab has been proven to increase the tolerance threshold for allergenic foods and is being tested in combination with oral immunotherapy.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Thomas G, Gomez J, Seagull S (2023) The Therapeutic Interventions in Treating Pediatric Allergy in Children and its Clinical Manifestations. Clin Pediatr. 08:254.
Received: 27-Oct-2023, Manuscript No. CPOA-23-29223; Editor assigned: 30-Oct-2023, Pre QC No. CPOA-23-29223 (PQ); Reviewed: 13-Nov-2023, QC No. CPOA-23-29223; Revised: 20-Nov-2023, Manuscript No. CPOA-23-29223 (R); Published: 27-Nov-2023 , DOI: 10.35248/2572-0775.23.08.254
Copyright: © 2023 Thomas G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.