
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Commentary - (2016) Volume 7, Issue 10
Ultrasound use for the placement of central venous catheters has become part of routine practice and is advocated by many governing bodies. The use of real time ultrasound has been shown to improve first pass success rate and reduce the risk of complications such as arterial trauma. Complications arising from inadvertent carotid dilation/cannulation include haemorrhage, pseudo aneurysm, AV fistula formation, arterial dissection, neurological injury including stroke and lethal airway obstruction secondary to haematoma formation. The use of ultrasound has reduced but not fully eliminated the risk of inadvertent arterial dilation/cannulation. This is often due to operator inexperience and/or the incorrect use of ultrasound. The consequences of inadvertent arterial dilation/cannulation to the patient can be life threatening and it is important that we do not become complacent when inserting central lines under ultrasound guidance or when supervising others using ultrasound. Additional checks such as pressure transducing the needle or performing blood gas analysis on the aspirate prior to dilation should not be forgotten when there is concern about needle placement.
Keywords: Inadvertent arterial cannulation, Inadvertent arterial dilation, Central venous access, Complications
Ultrasound use for the placement of central venous catheters has become part of routine practice, especially in the elective setting when the internal jugular or femoral sites are used.
The use of ultrasound is advocated by several governing bodies including the National Institute for Health and Care Excellence (NICE, UK) [1], The Association of Anaesthetists of Great Britain and Ireland (AAGBI) [2] and the American Society of Anesthesiologists (ASA) [3]. The use of real time ultrasound is associated with a higher first pass success rate and reduced risk of complications such as carotid puncture and venous trauma. The incidence of inadvertent arterial cannulation is quoted as between 0.1% and 0.5% [4].
Complications arising from inadvertent carotid puncture/dilation/ cannulation include [5,6]:
• Haemorrhage
• Pseudoaneurysm
• AV fistula formation
• Arterial dissection
• Neurological injury including stroke
• Lethal airway obstruction secondary to haematoma formation.
Carotid puncture with a needle is associated with considerably less risk of trauma and complications compared with when the artery is dilated and catheterised. It is therefore important that arterial cannulation is avoided or at least recognised at an early stage prior to dilatation.
The use of ultrasound has reduced but not fully eliminated the risk of inadvertent arterial dilation/cannulation. This is often due to operator inexperience with ultrasound, the incorrect use of ultrasound and/or lack of associated checks when there is concern with needle placement.
Many anaesthetists will have heard of or been involved with a case of inadvertent arterial injury when ultrasound has been used. After witnessing a patient experiencing impending airway obstruction as a result of haematoma formation from the inadvertent dilation of the carotid artery when ultrasound was being used, I felt it was important to reflect on whether we are becoming complacent when inserting central access devices due to the perceived ‘safety factor’ that ultrasound provides [7].
Are we optimizing patient’s coagulation prior to line insertion or are we tolerating a degree of abnormality that we wouldn’t have when using a landmark technique? Are we always selecting the most appropriate site for central access in the patient? Or are we as default using the internal jugular vein because this site is most commonly selected and the use of ultrasound in this location is more familiar?
Finally are we cutting corners with our ultrasound technique and/ or not using additional checks when there is concern about needle placement?
Correct use of ultrasound
The most commonly used sites for central access include the internal jugular vein, femoral vein and subclavian vein. Central access via the internal jugular vein may be associated with less mechanical trauma (i.e. pneumothorax) than when the subclavian vein is used and due to the position of the subclavian artery compression of the site in the event of arterial puncture/cannulation is not possible [8]. The femoral site is associated with a higher rate of thrombosis and bacterial colonisation than subclavian and jugular sites but has the advantage of being in a location away from the airway and easy to compress [3].
There is evidence that the use of ultrasound for internal jugular vein, femoral vein and subclavian vein access improves first pass success rate and reduces the risk of complications [3,4]. The ASA propose that ‘real time ultrasound should be used for guidance during venous access when either the internal jugular or femoral veins are selected for cannulation. The consultants and ASA members are equivocal regarding the use of real time ultrasound when the subclavian vein is selected [3].
Ultrasound is used for the identification of landmarks, witnessing the insertion of the needle into the vein (in plane/out of plane) and for confirmation that the guide wire is in the vein.
There are several components involved in the correct use of ultrasound for central access these include:
• Correct probe selection and ultrasound machine set up
o Frequency
o Probe shape and size
o Machine set up-depth, gain, and focus
• Ultrasound technique
o Identification of structures
o Dynamic ‘real time’ scanning vs. static scanning
o In plane vs. out of plane techniques
o Confirmation of guidewire location in vein
Probe selection and ultrasound machine set up
Frequency affects the penetration of the ultrasound waves. For superficial structures higher frequencies will ensure better axial resolution and give a clearer image. Lower frequencies enable deeper structures to be viewed but at the expense of poorer axial resolution and image quality. As most vascular structures are at a depth of 2-4 cm a high frequency ultrasound probe is required [9,10].
A probe that has a small footprint is preferable due to the limited space at some of the vascular sites, this aids probe contact with the skin and image stability.
The linear array probe is ideal due to its small footprint and high frequency setting (6-13 MHz). Curved array probes are available but are more suitable for deeper structures as they use lower frequencies (2-5 Mhz) and have a larger footprint. They should be avoided for superficial vascular sites due to the poorer images they produce [9,10].
When setting up the ultrasound machine it is important that you select the correct mode (B mode-2D image) and settings in order to optimise the image. There is often a ‘vascular structures’ setting which can be selected to reduce the amount of alterations needed. The depth should be adjusted so that the vascular structures are in the centre of the image. Too deep and the vein appears very small and too shallow means that the accompanying artery can be missing from the picture. The best focus is often in the centre of the image which means that buy selecting the correct depth it can improve the view of the vascular structures. Many machines also have the function to adjust the focus and focal position manually. Finally gain affects image brightness and can be increased or decreased to optimise the image.
Ultrasound technique
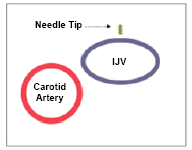
It is advisable to scan a short distance up and down the vein to see if there is a location where the artery and vein do not overlie but rather lie lateral to one another. This will help reduce the risk of arterial puncture.
Arteries are pulsatile and not easily compressible whereas veins are often readily compressible and non-pulsatile. The head down position for internal jugular vein sites will increase the size of the vessel. If there is any uncertainty a valsava manouvre will increase the size of the interal jugular vein. Colour Doppler mode can be used to identify the direction of blood flow and help distinguish arteries from veins. The acronym BART is commonly used-Blue Away, Red Towards [10].
The use of ‘static’ ultrasound for the identification of landmarks is not advocated. Dynamic or ‘real time’ ultrasound scanning where the probe is used to visualise the needle entering the vein is recommended [2,3].
A in plane (longitudional) or out of plane (transverse) technique can be used. Both methods have advantages and disadvantages (Table 1).
| In Plane (longitudional) | Out of Plane (transverse) | |
|---|---|---|
| Overview | 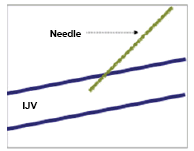 Needle is placed inline and parallel to transducer. |
 Needle placed perpendicular to transducer. |
| Advantages | The whole needle can be visualised entering the vessel as long as the probe, vessel and needle are correctly aligned. | More familiar technique and easier to initially learn. Both artery and vein can be visualised at all times. |
| Diadvantages | Beam, needle and vessel all need to be in parallel, which can be difficult for a novice. Artery may not always be visible when vein in view depending on its location in relation to the vein. |
Needle tip can sometimes be difficult to locate and can be misidentified as needle shaft. |
Table 1: In plane and out plane technique.
For either method it is important that the tip of the needle is correctly identified and visualised throughout. Misidentifying the needle shaft as the tip, can lead to the actual tip being in a posterior placed artery.
When confirming the position of the guide wire the wire should be visualised along the length of the vein, for internal jugular locations scanning should occur from the insertion point distally to the supraclavicular fossa. A single cross section scan close to the insertion point can confirm wire position in the vein but miss its eventual entry into the artery [11].
In addition to the correct use of ultrasound, additional checks can also be used to help avoid misplacement of the needle and reduce the risk of complications:
Pre procedure
Ensuring the operator is skilled in the use of ultrasound or appropriately supervised.
Optimising the patient prior to line insertion eg correct abnormal coagulation, head down position for internal jugular vein access.
During the procedure
Recognising high pressure or pulsatile flow from the needle prior to guidewire insertion. This may not be obvious in hypotensive critically ill patients.
Performing blood gas analysis on the initial aspirate prior to dilatation.
The needle pressure can be checked with the use of a manometer or pressure transducer prior to guide wire insertion if there is a concern about needle location. This can be associated with other complications including needle displacement, blood loss, loss of sterility and venous air embolism [3,5].
Post procedure
Transduce the central venous catheter to ensure a venous trace is obtained.
Perform blood gas analysis.
Check catheter tip position with a chest radiograph at the earliest opportunity. It is important to note that it will not always be possible to identify arterial placement due to the close proximity of the arteries and veins.
If carotid dilation and/or cannulation do occur the catheter can either be removed immediately and compression applied or the catheter left in place and expert advice from a Vascular Surgeon or Interventional Radiologist obtained.
There are risks associated with either option; with removal there is a risk of haemorrhage and haematoma formation especially in patients with coagulation abnormalities, however there is a recognised risk of neurological injury and stroke with prolonged catheter insertion [6]. The ASA advises that ‘when unintended cannulation of an arterial vessel with a dilator or large-bore catheter occurs, the dilator or catheter should be left in place and a general surgeon, a vascular surgeon, or an interventional radiologist should be immediately consulted regarding surgical or nonsurgical catheter removal for adults’ [3].
If the subclavian artery has been cannulated then it would be advisable that the catheter be left in place due to the inability to compress the vessel and specialist advice sought.
The consequences of inadvertent arterial dilation/cannulation to the patient can be life threatening and it is important that we do not become complacent when inserting central lines under ultrasound guidance or when supervising others using ultrasound.
Ultrasound has reduced the occurrence of complications but not eliminated the risk completely. It is vital that the practitioner inserting the line has the appropriate knowledge and skills in using ultrasound, or is adequately supervised. Additional checks such as pressure transducing the needle or performing blood gas analysis on the aspirate prior to dilation should not be forgotten when there is concern about needle placement.