
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Case Report - (2022)Volume 13, Issue 6
A 22 year old primi diagnosed as Eisenmengers syndrome with severe pulmonary hypertension with bidirectional shunt and room air saturation of 78% was taken up for emergency caeserian section under thoracic segmental spinal anaesthesia with low volume isobaric 0.5% levobupivacaine and fentanyl. Patient was haemodynamically stable during the intraoperative and postoperative period and was discharged safely on the 10th postoperative day. Thoracic segmental spinal anaesthesia with isobaric levobupivacaine is a good alternative to epidural and general anaesthesia in patients with cardiac and respiratory diseases.
Thoracic segmental spinal; Isobaricbupivacaine; Eisenmengers syndrome; Pregnancy
Eisenmengers syndrome refers to any untreated congenital cardiac defect with intracardiac communication that leads to pulmonary hypertension, reversal of flow and cyanosis [1]. The previous left to right shunt is converted into a right to left shunt secondary to increase in the pulmonary artery pressure. Development of syndrome indicates the pulmonary hypertension is irreversible and the lesion is inoperable. Incidence in pregnancy is very rare about 3%. Pregnancy related physiological changes are poorly tolerated in Eisenmengers and early termination of pregnancy is advised. Continuation of pregnancy with Eisenmengers carries a very high maternal mortality rate of 40-70 percent. We present a case of 22 yr primigravida with Eisenmengers syndrome managed under segmental thoracic spinal anaesthesia.
A 22 year-old primigravida of 34-35 weeks, a known case of Eisenmengers syndrome with large bidirectional shunt and severe pulmonary hypertension was referred to our institution from a private hospital for caeserian section. She was diagnosed as a case of Eisenmengers syndrome in a private hospital three months back and was having her antenatal checkups there. She was put on tablet sildenafil citrate and tablets Frusemide by the cardiologist there, and was referred to our institution for emergency caeserian section at around 35 weeks of pregnancy [1].
Preoperatively on history elicitation, patient complaints of exertional dyspnea from 24 weeks of pregnancy but otherwise able to take care of her daily activities. On general examination she had central cyanosis, clubbing, her weight was 52 kg, height 152 cm, Pulse rate 98/min, BP-118/78 mmhg, room air saturation of 78%, with oxygen supplementation of 4 litres/min the saturation increased to 86%. On auscultation a pansystolicmurmur of grade 3/6 was heard in the left sternal border and normal vesicular breath sounds heard.
Cardiac evaluation was repeated in our institution and echo showed a large perimembranous ventricular septal defect, bidirectional shunt, adequate left ventricular function, severe pulmonary hypertension (RVSP-73 mmhg), RARVdilated, valves normal, no clot. Cardiologist suggested high cardiac risk for surgery and advised Infective Endocarditis prophylaxis before surgery (Figure 1).
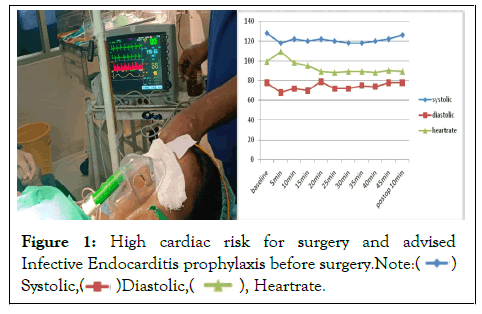
Figure 1: High cardiac risk for surgery and advised
Infective Endocarditis prophylaxis before surgery.

Investigations showed Hemoglobin of 16.1 g, coagulation profile was normal, electrolytes Na+-131, K+-3.5, renal function tests within normal limits. ABG was not done due to non-availability of the facility. Patient and attenders were explained about the high risk for surgery and anaesthesia and also explained about the plan of thoracic spinal anaesthesia and its complications.
Patient was shifted inside the operation theatre, was connected to multipara monitor, peripheral line was secured and started on ringer lactate. Right internal jugular vein was cannulated under aseptic precautions and meticulous attention was paid to avoid air bubbles in the lines. Phenylephrine infusion of 20 ug/min was kept ready. Her preoperative vitals showed Pulse Rate-99/min, Blood pressure-124/75 mmHg, CVP-14 cms and saturation of 78% in room air. She was kept on ventimask with 4 litres of oxygen and her saturation increased to 86%.
Patient was positioned in the sitting posture and under aseptic precautions T10-T11 space was identified and infiltrated with 2% lignocaine, then 26 g Quinkes needle was inserted by midline approach and after free flow of cerebrospinal fluid 1.2 ml of 0.5% isobaric Levobupivacaine with 20 ug Fentanyl was given. Patient was made to lie down in the supine posture and prophylactically a bolus dose of 20 ug phenylephrine given. Level of blockade was assessed by pinprick method and was confirmed at T6 to L1. Patient was able to move the ankles and slightly bend the knees (bromage score 3). Surgeon was allowed to proceed and patients pulse rate, blood pressure and saturation, were monitored and recorded every 5 minutes (Figure 2).
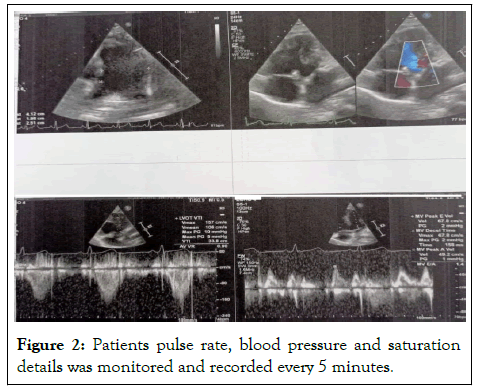
Figure 2: Patients pulse rate, blood pressure and saturation details was monitored and recorded every 5 minutes.
Patient was haemodynamically stable throughout the procedure except for occasional pruritis over the nose. On delivery of the fetal head injection oxytocin 10 units was given intramuscularly. Male baby was delivered with APGAR score 6/10, 7/10, weight 1.6 kg and was shifted to Neonatal intensive care unit. Surgery lasted for 45 min and totally 750 ml of crystalloids given, and urine output was 100 ml. postoperatively patient was able to bend her knee partially and she was able to move herself to stretcher with minimal help. Patient was shifted to postoperative intensive care unit and vitals were monitored continuously. She was haemodynamically stable and Paracetamol infusion was given three times a day for postoperative pain relief and advised to avoid opioids as it may cause respiratory depression, hypoxia and worsen the shunt. Post operatively patient maintained saturation of around 90% with 4 litres of oxygen. Patient was discharged to ward after 48 hrs of monitoring in the intensive care unit.
Pregnancy induced physiologic changes worsen the Eisenmengers syndrome and Anaesthesia management will be really challenging and we aim at maintaining the systemic vascular resistance, avoiding hypotension, hypoxia, hypercarbia and factors increasing the pulmonary vascular resistance. General anaesthesia was used for most of the cardiac diseases in pregnancy but we opted for segmental thoracic spinal anaesthesia as the patient was on full stomach and MPG 3 [2]. Many references show cases being successfully done under graded epidural, but in case of emergency caeserian section for fetal distress epidural is not ideal due to time consumption [3]. In segmental thoracic spinal we used a low volume of 0.5% isobaric levobupivacaine with 20 ug fentanyl. The advantage of isobaric drug is that its spread is not affected by the position of the patient and isobaric levobupivacaine is more cardiac stable than plain bupivacaine. By using isobaric levobupivacaine of 1.2 ml in the lower thoracic level the spread of the drug was 3-4 segments above and below the site of injection, and there will be lumbosacral sparing and the venous pooling in lower limbs leading to decrease in venous return and hypotension is avoided. Even in cardiac cases haemodynamic stability is well maintained.
Spine anatomy shows that the space between durameter and the spinal cord in the thoracic region is greater when compared to the space in the lumbar area. MRI shows a distance of 4.8-5.6 mm between the cord and the durameter at thoracic levels, so the risk of spinal cord injury is very rare if done by expert. Now with ultrasound guided thoracic spinal the risk of injury is almost nil [4,5].
Thoracic segmental spinal with low volume isobaric drug is an alternative to general anaesthesia especially in patients with respiratory or cardiac disease due to its remarkable hemodynamic stability, patient satisfaction and avoids polypharmacy and perioperative complications. To minimisecollateral effects, thoracic spinal anaesthesia may be given at a dose that is half that of the lumbar area. Similar to this, using hyperbaric solutions and adopting a mild Trendelen burg position helps the solutions permeate throughout the posterior canal (sensitive rootlets), resulting in shorter motor block durations and longer sensitive block durations. In comparison to general anaesthesia, the segmental thoracic spinal anaesthetic approach offers improved patient satisfaction, superior postoperative analgesia, and fewer problems in patients having breast cancer surgery.
We certify that we had obtained patient consent forms for their clinical information and images can be reported in this journal. The patients understand their names will not be published.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Yangste SN, K. Kalyanasundram ( 2022) Thoracic Segmental Spinal Anaesthesia with Isobaric Levobupivacaine for Caeserian Section in a Patient with Eisenmengers Syndrome. J Anesth Clin Res. 13:1065.
Received: 03-Jun-2022, Manuscript No. JACR-22-18541; Editor assigned: 06-Jun-2022, Pre QC No. JACR-22-18541 (PQ); Reviewed: 22-Jun-2022, QC No. JACR-22-18541; Revised: 28-Jun-2022, Manuscript No. JACR-22-18541 (R); Published: 05-Jul-2022 , DOI: 10.35248/2155-6148.22.13.1065
Copyright: © 2022 Yangste SN et al.This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.