
Journal of Perioperative Medicine
Open Access
ISSN: 2684-1290

ISSN: 2684-1290
Research - (2024)Volume 7, Issue 4
Background: Endotracheal intubation is a critical skill for anaesthesia providers and any healthcare provider responsible for airway management. Despite the clinical significance, this skill continues to be a challenging procedure for beginner Student Registered Nurse Anesthetists (SRNAs) to master. Current training manner fail to account for the dynamic changes experienced in live patients. The purpose of this project is to evaluate whether Augmented Reality (AR) airway applications reduce the time to endotracheal intubation in new learners.
Methods: Research methods include searching databases, such as PubMed, Web of Science (WoS) and Cumulated Index to Nursing and Allied Health Literature (CINAHL) and narrowing results with keywords, inclusion and exclusion criteria. The study design used in this research project can be classified as an evidence- based intervention or quality improvement initiative. The population of this study included first-year Student Registered Nurse Anesthetists (SRNAs) of Emory University. The researchers analyzed time to intubation before and after Augmented Reality (AR) interactive education on the Airway Ex application.
Results: The median time Pre-AR and Post-AR were 14.22 seconds and 13.55 seconds, respectively. Wilcoxon Signed Ranked test with a two-tailed significance value of 0.394 indicates that these results are not statistically significant. The surveys demonstrated improved confidence in Direct Laryngoscopy (DL) skills post AR, better understanding of patient airway anatomy, enhanced learning experience and most participants reported ease of use of AR as an education modality.
Conclusion: This study highlights the potential of utilizing AR in the training of beginner SRNAs. There is a need for additional research with a larger sample size to establish statistical significance and further evaluate this novel training modality.
Direct laryngoscopy; Endotracheal intubation; Intubation time; Apneic time; Anesthesia training; Augmented reality
In today’s society, Augmented Reality (AR) has emerged as an innovative tool to facilitate entertainment, education, and communication by immersing people in new experiences in a safe way [1]. When utilized in education and training programs, AR encourages learners to acquire competency by repeatedly practicing complex skills in a safe and non-punitive environment. Furthermore, AR is resource friendly and precludes the need for a patient, cadaver, or other disposable supplies [1]. As a result, AR provides a secure environment for education that allows individual students to gain confidence while learning new skills.
Background and significance
State of knowledge: Traditional learning modalities for endotracheal intubation include working with manikins and cadavers, both of which present limitations in their representation of reality as well as concerns regarding access and cost. AR displays a dynamic and realistic model for students to learn and practice tracheal intubation. Although manikin practice can be helpful for students and providers to sharpen their technical skills, it does not allow for the interactive and visually accurate training provided by AR simulation [2]. By improving intubation skills with AR, the SRNA will perform intubation more efficiently when in the operating room, thereby reducing the patient’s apneic time and associated complications. Prolonged apneic time can lead to patient hypoxia, which, if uncorrected, can lead to lethal cardiac arrhythmias, cerebral ischemia, respiratory arrest, and death. Minimizing apneic time is especially important in patients with limited oxygen reserve, such as obese, pregnant, paediatric or hypermetabolic patients [3]. These patients are at an increased risk for rapid desaturation once apnea is induced. To increase oxygen reserve in these high-risk patient populations, anaesthesia providers utilize preoxygenation, passive oxygenation and proper “sniffing” positioning to reduce the incidence of intubation induced hypoxia. However, ultimately, the intubation technique and mastery remains the most significant factor in reducing the hypoxic time for patients. Competence in tracheal intubation cannot be understated. By quickly securing the airway, the anesthesia provider can oxygenate the patient and prevent an adverse outcome. First-year SRNAs often struggle with tracheal intubation; therefore, AR should be employed as a novel teaching modality to enhance understanding, improve intubation skills and reduce time to intubation in the clinical setting.
Epidemiology
Many Certified Registered Nurse Anesthetist (CRNA) programs lack the financial and physical resources to provide a cadaver or high-fidelity simulation lab for their students. As a result, they rely on traditional learning methods, such as plastic manikins, to teach first-years SRNAs the complex skill of intubation. AR addresses this limitation by providing an interactive, anatomically accurate, widely accessible, and cost-effective alternative to traditional teaching modalities that enhances the understanding and skill level of the learner. The ability to download the AR airway app on any smartphone device improves access to high- quality learning experiences for students who lack access to non- traditional learning methods and struggle in the clinical setting. Many digital AR airway applications are available for download at little to no cost. For example, the Airway Ex-application is entirely free of charge. Many nurse anesthesia programs require their students to possess technological devices, such as a smartphone or laptop, prior to beginning the program; thus, it is assumed the students have access to these devices. In addition to improving affordability, the AR airway app addresses diversity, equity and inclusion by offering diverse simulation scenarios featuring patients of various ages, genders, ethnicities and other demographic variations. In this way, AR promotes inclusion while increasing the student’s exposure and confidence in caring for diverse populations in the clinical setting.
Significance: Tracheal intubation is a fundamental skill for airway experts and anesthesia providers to master to ensure adequate ventilation and thus oxygenation of patients. Placing an endotracheal tube is a complex procedure that requires delicate, quick and precise movements. Perfecting this skill reduces the apneic time for the patient, as well as subsequent tissue damage from multiple intubation attempts and hemodynamic compromise that may ensure if apneic time is prolonged. Therefore, it is important to limit the time to intubation to improve patient outcomes [4]. Teaching endotracheal intubation may be challenging due to individual differences in airway anatomy and the inability of the teacher to share the same view point with learners [4]. Augmented reality presents a solution to this challenge by granting a shared view of the glottis opening during tracheal intubation, leading to enhanced learning and skill development in airway management. Many traditional educational programs utilize plastic manikins within a simulation lab to assist beginner students in learning the skill of intubation. Research has proven this to be effective [4]. However, the addition of AR amplifies the learning experience by allowing the teacher to share the same view as the student, further improving the instructor’s ability to coach the student on their intubation technique [4]. Additionally, the student will gain an advanced understanding and familiarity with an anatomically accurate view of the glottis opening and surrounding structures that a plastic manikin cannot provide. As aforementioned, these benefits provide students with a more effective learning modality for the skill of tracheal intubation, thereby improving first-time intubation success rates and reducing time to intubation for new SRNAs in the hospital setting.
Theoretical framework
During the 1950s, statistician and researcher lead efforts to improve business with statistical thinking and quality improvement methods, originally applied in the automotive industry [5]. Deming’s theory can be adapted and applied to the field of healthcare to accelerate quality improvement initiatives [6]. Deming’s system-focused theory consists of four key elements: Appreciation for a system, knowledge about variation, theory of knowledge and knowledge of psychology [4]. Improving intubation skills among 1st year SRNAs to reduce the apneic time for the patient is a quality improvement initiative focused on system and process improvement, thereby aligning with the pillars of Deming’s theoretical model, specifically the theory of knowledge. The theory of knowledge promotes learning as individuals and as an organization to improve system operations and subsequent quality outcomes. Deming’s theory exerts that significant and sustainable quality improvement can be achieved through leadership, training, understanding of system dynamics and variation and application of tools such as the Plan-Do-Study- Act (PDSA) cycle [6,7]. Rather than punishing an individual for a poor outcome, Deming’s theory examines the process and environment in which the person operates to identify a system based solution to the root cause. The field of anesthesia is dynamic, with considerable variation influenced by patient factors, anesthetic options and provider training or preference. By improving the training of first-year SRNAs with an airway app using Augmented Reality (AR), the students engage in a high- quality, dynamic learning environment to improve intubation skills and patient outcomes, secondary to reduced apneic time. An airway app utilizing AR accounts for the variation experienced during human endotracheal intubation and prepares students to better manage the airway when variations exist, such as with patient anatomy (i.e., enlarged tonsils, anterior larynx), then traditional learning methods (manikins, models). To substantiate his Theory of Knowledge, Deming designed the Plan-Do- Study-Act (PDSA) cycle to guide individuals and organizations in planning, implementing and evaluating a system or process change. Improving the safety and quality of healthcare begins with the education and training of new healthcare professionals. This exploration for quality improvement is best executed when using a strong theory and theoretical framework to guide change. The Plan-Do-Study-Act (PDSA) model (Figure 1), is a cyclic theoretical framework that has driven advancement in many different modalities of healthcare improvement by structuring the development and scientific analysis of complex ideas [8,9]. As the acronym suggests, PDSA consists of four distinct stages. The plan stage involves identifying a primary intervention aimed at improving outcomes, identifying objectives, forming a hypothesis and detailing steps to carry out the cycle. The do stage involves the conduction of the study and data collection. During this stage that execution of the plan occurs, in addition to documentation of outcomes (results, complications, unexpected observations). Next, the study stage involves a thorough examination of results, data analysis and interpretation of the results. Finally, the Acceptance and Commitment Therapy (ACT) stage determines what changes can be implemented based on the findings or if another modified PDSA cycle should be instituted. The PDSA model provides important information in guiding an organization to develop meaningful and sustainable change by outlining each step of the change process, such as abandoning or adopting a new method [9].
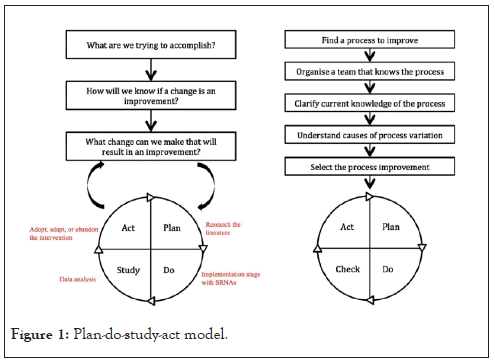
Figure 1: Plan-do-study-act model.
Framework application
The purpose of this project is to investigate the efficacy of an airway app utilizing Augmented Reality (AR) in reducing time to intubation with Direct Laryngoscopy (DL), thereby improving airway management skills and subsequent intubation success among first-year SRNAs. The PDSA model is a foundational framework based upon Deming’s Theory that can be employed to provide structure and clarity when conducting this study and implementing the new AR education modality [6]. The Planning stage of the PDSA cycle will correlate with the planning of our project. Specifically, we will conduct research related to our project so that goals and predictions regarding outcomes can be created as supported by the literature. To narrow our objective, we will specify who, what, where and why to implement this project. Additionally, it is during this stage that methods for data collection will be clarified, including the availability of tools and resources (i.e., intubating equipment, manikins, airway app) at Emory University, where the study will take place. The doing stage of the PDSA cycle aligns with the implementation phase of our project. Students will be active participants while engaging with the AR airway app and intubating the manikins. The researchers will document observations and record intubation times both before and after the SRNA uses the AR airway app. The collected data will then be analysed, which aligns with the study stage of the PDSA cycle. This data analysis will reveal whether the use of the AR airway app caused a statistically significant reduction in time to intubation among the study participants. The outcomes will then be compared to the mentioned predictions and a summary of results, including key learning points, will be designed. Finally, during the act stage, the researchers will utilize the study results to guide the next steps. To conclude this project’s PDSA cycle, the new learning modality (AR airway app) will either be adopted, adapted or abandoned. If the results demonstrate statistically significant improvements in intubation time, the intervention can be adopted without further changes and incorporated into the official university teaching curriculum. If the study is modified, such as expanding to a larger sample population, another PDSA cycle should be completed prior to implementing the intervention [9]. In summary, Deming’s theory of knowledge appreciates that information and experience work synergistically to create sustainable change in the education and training of first- year SRNAs. Both the theory and model suggest that the most effective solution to a problem or quality improvement initiative is the product of constantly asking questions and re-evaluating outcomes. The PDSA cycle guides project creation through a series of predictions and observations that can be modified within the model and throughout the study process [9]. As a result, the PDSA cycle model guides the process to improve education and intubation skills for new learners.
Among new anesthesia providers, achieving competency in endotracheal intubation via direct laryngoscopy is necessary for the delivery of safe and efficient anesthesia care. Due to the reduced cost and ease of accessibility, many traditional educational programs utilize plastic or latex manikins within a simulation lab to assist students in learning the skill of intubation. Although manikin practice allows students to develop their technical skills, it fails to accurately represent reality for the anesthesia trainee. In contrast, AR displays a dynamic and realistic model for students to learn and practice endotracheal intubation. This method is interactive, engaging and anatomically accurate [2]. By using AR to improve intubation education, the trainees will be equipped to perform intubations more efficiently in the healthcare setting, thus reducing the patient’s apneic time and associated complications. Extended apneic time can lead to patient hypoxia, which, if uncorrected, can potentiate lethal cardiac arrhythmias, cerebral ischemia, or even death [2]. AR should be integrated into the clinical training of first-year SRNAs as a novel teaching modality to enhance understanding, improve intubation skills, and reduce time to intubation in the clinical setting. The purpose of this study is to examine the efficacy of augmented reality in reducing time to intubation via direct laryngoscopy in new SRNAs.
Search methods
The databases searched include PubMed, Web of Science (WoS), and Cumulated Index to Nursing and Allied Health Literature (CINAHL). The keywords for the search included direct laryngoscopy, endotracheal intubation, intubation time, apneic time, anesthesia training, and augmented reality. Inclusion criteria included health science students in training, learning the skill of endotracheal intubation and utilization of direct laryngoscopy. Exclusion criteria included articles published before the year 2000 and non-English language. During the literature search, results were narrowed down by utilizing specific keywords, trying different combinations of keywords, and limiting the inclusion and exclusion criteria.
Results review
For the purpose of this literature review, a total of 10 articles were reviewed and sorted into three categories based on the most apparent themes identified in the literature, including technical skill improvement, non-technical skill improvement and technological variation. Articles related to technical skill improvement assess whether AR improves the efficiency and success of intubation, as evidenced by intubation time, whereas articles related to non-technical skill improvement assess whether AR enhances understanding and personal development for new learners. Finally, articles related to the theme of technological variation evaluate whether the quality of the AR equipment supports or inhibits the learning experience. The highest quality data included in this Literature Review, according to the Grading of Recommendation Assessment Development and Evaluation (GRADE) system, consists of randomized controlled trials by Qian, et al., Alismail, et al. and Natal, et al. [10-12].
Technical skills
Endotracheal intubation is a technical skill that requires repeated practice to gain proficiency. Yet, AR has emerged as a novel teaching modality to accelerate proficiency in this skill. Qian, et al. conducted a randomized controlled trial to evaluate endotracheal intubation proficiency among novice anesthesia providers utilizing AR-assisted video laryngoscopy [10]. During the study, AR-assisted video laryngoscopy glasses were worn by the trainee, whereby a magnified image of the patient’s airway was projected directly into the trainee’s visual field. This allowed the instructor to visualize the trainee’s technique and view and offer real-time feedback, without interruption of the trainee’s intubation. In the study, 45 healthcare providers with no prior intubation experience were randomly divided into three groups: Direct laryngoscopy, indirect video laryngoscopy and AR-assisted video laryngoscopy. Outcome measures included successful endotracheal intubation (<30 seconds), unsuccessful intubation due to time (30-60 seconds), unsuccessful intubation due to time (>60 seconds), and unsuccessful due to oesophageal intubation. The results revealed that the AR group exhibited a greater percentage of successful intubations compared to the DL group (70% vs. 32%). In addition, the AR group had zero incidence of oesophageal intubation, whereas the DL group intubated the oesophagus on 26% of attempts. The median time to intubate in the AR group was 20 seconds, compared to 35 seconds in the DL group. Such results conclude that in a simulation environment, intubation success among novice trainees was greatly improved utilizing AR-assisted laryngoscopy. A similar conclusion was derived from Hamza-Lup, et al. [13]. A randomized controlled study by Alismail, et al. evaluated the effectiveness of using AR glasses to perform intubation in the simulation setting [11]. During the study, 32 trainees from various healthcare backgrounds were randomly assigned to one of two groups: An AR group and a non-AR group. Participants from both groups were required to watch an educational video following a 17-point New England Journal of Medicine (NEJM)- based intubation checklist. The AR group was provided additional training and instruction on how to use the AR glasses. Following the education session, the AR group proceeded to intubate a mannequin using the AR glasses while the non-AR group performed a traditional intubation. Both groups were required to follow the aforementioned NEJM intubation checklist. AR group had direct visualization of the NEJM checklist within the AR glasses throughout the procedure, whereas the non-AR group participants were required to audibly deliver each step they could recall from the checklist during the procedure. In both groups, adherence to the NEJM checklist was assessed and the time to endotracheal intubation and ventilation was recorded. The results revealed that the AR group took longer median time to ventilate than the non-AR group (280 seconds vs. 205 seconds). This prolonged time to intubation may be explained by the AR group having to read and follow real-time instructions projected onto the glasses. In addition, the AR group demonstrated a greater adherence to the NEJM checklist than the non-AR group (100% vs. 82.4%). These results suggest that AR technology is effective in teaching the steps of endotracheal intubation in a simulation setting, but more research is needed to determine the clinical usefulness in patient care settings. A major limitation of this study is that the variable of user experience was not factored into the group randomization. As a result, the AR group had less human intubation experience than the non-AR group (46% vs. 60%), which may account for the prolonged time to ventilate in the AR group. During the post-procedure survey, participants with intubation experience remarked that the AR system “slowed them down,” as they already knew the next step to perform in the intubation sequence. Such survey responses support the idea of using AR in novice, rather than experienced, trainees. Additionally, Qian, et al. conducted a study to evaluate the benefits of using AR-assisted laryngoscopy on a head-mounted device to improve endotracheal intubation training and maintain a direct line-of-sight view for the trainee [10]. The study found that there was a lack of opportunities for medical trainees to intubate the neonate population in the clinical setting, resulting in less proficient providers at the bedside. Tracheal intubation is a difficult skill to learn and teach to new learners. The most common reason for a failed intubation is the inability to visualize the vocal cords during laryngoscopy and this can be improved by using better techniques and having more experience. One way to learn this is by using AR-assisted laryngoscopy, especially in populations of providers with limited opportunities for endotracheal intubations. A study was performed by Lenovo Research and the Duke, Neonatal Intensive Care Unit (NICU) and the subjects selected were 45 NICU nurses with no hands-on experience with intubation. The goal of the study was to evaluate the technology as an educational tool for new providers. The nurses were randomly assigned to three groups. The first group intubated an infant manikin using the standard intubation technique of direct laryngoscopy. The second group intubated an infant manikin using video laryngoscopy that projected onto the capture PC laptop at the bedside. The third group intubated an infant manikin using AR-assisted video laryngoscopy and glasses with the supplemented video stream to supplement their view [11]. Each participant was graded based on successful endotracheal tube placement, placement within the 30-second time frame, unsuccessful due to time or greater than 60 seconds or unsuccessful due to oesophageal intubation. The pilot study by Qian, et al. found that the time to complete one intubation was improved in both the video laryngoscopy and AR-assisted video laryngoscopy groups by an average of 10 seconds [10]. This was attributed to an improved identification of the airway as the direct laryngoscopy group acquired airway visualization in an average of 18 seconds while AR and video laryngoscopy acquired the airway visualization in 5.01 seconds and 4.65 seconds respectively. In conclusion, this study found that both AR-assisted video laryngoscopy and indirect video laryngoscopy improved intubation proficiency. Each participant answered an anonymous survey on a 5-point Likert-scale and found that AR smart glasses improved glottis view, improved shared view with the expert instructor, and improved the training of beginner airway providers [13]. This demonstrates that the AR- assisted laryngoscopy can be an effective tool in teaching endotracheal intubation. A systematic review and meta-analysis was performed by Kononowicz, et al. to evaluate the effectiveness of virtual patient simulations compared to traditional education in various health professions [3]. A total of 51 randomized controlled trials involving 4696 participants were included in the meta- analysis and results revealed that virtual patient simulations more effectively improved skills, including clinical reasoning, procedural skills and a mix of procedural and team skills, than traditional learning [3].Non-technical skills
Anesthesia training requires both technical and non-technical skills. In addition to improving the technical skill of intubation, AR also enhances non-technical skills that contribute to a successful intubation such as decision-making, communication, confidence and adaptability. Fully immersing in an AR-based clinical environment teaches the student effective decision- making during uncommon crises. For example, the clinical status of virtual patients will improve or deteriorate in real time as a direct result of the student’s actions [14]. This allows the student to reflect and learn from their clinical decisions via positive or negative feedback from the manikin. In addition to enhancing decision-making skills, AR improves communication skills between the learner and the instructor by allowing constant coaching and dialogue about the patient’s condition, which becomes visible to both parties in AR. A study conducted by Davis, et al. Highlights the communication benefit of utilizing AR technology during intubation training [13]. Specifically, Davis, et al. evaluated the use of telehealth glasses and AR during endotracheal intubation to help learners and faculty share the same view point [14,15]. During this qualitative descriptive design study, 14 nurse practitioner students wore telehealth glasses and individually intubated a manikin while a faculty member shared the student’s view on a laptop synced with the glasses. This allowed for real-time verbal instructions to guide the students while performing endotracheal intubation. The study participants were asked open-ended feasibility and acceptability questions about their experience using the telehealth glasses focusing on advantages, disadvantages and recommendations. Advantages included improved visualization, innovation and immediate feedback, whereas disadvantages included uncomfortable glasses, hindered learning and technical issues. Eight of the fourteen participants argued that the glasses enhanced their learning experience and improved communication with the faculty member [14]. Finally, AR improves the student’s confidence with intubation, as they are able to perform numerous intubations over a small period of time. This repeated exposure to intubation in the virtual environment accelerates proficiency in this skill and confidence with airway management. AR improves confidence and preparation for students in a safe way that avoids potential harm to patients in the hospital. Adequate preparation and positioning of patients is essential for a successful intubation. A study by Munzer, et al. found that AR allowed students to visualize changes in airway patency with alterations in patient positioning [2]. In this way, students learned the appropriate techniques for intubation such as placing the patient in a sniffing position. Similarly, exposure to AR scenarios with varying levels of difficulty increases the student’s ability to adapt to changing circumstances, which translates to better patient care in the clinical setting [14].Technological variation
In an article by Rolland, et al. a training tool utilizing AR was developed to assist medical personnel, including medical students, residents, and nurse anesthetists, in learning the skill of endotracheal intubation [15]. The authors of this article argue that the most common cause of intubation failure is the inability to visualize the vocal cords, which is a problem that may be mitigated with the incorporation of AR in training. The AR system developed by Rolland et al. includes a Head- Mounted Projective Display (HMPD) with an associated PC to simulate and visualize internal airway anatomy, such as the trachea, mandible, larynx and vocal cords [15]. Although the purpose of this study is to develop, rather than test, an AR tool for improving endotracheal intubation, quantitative outcomes measurable by the tool include morbidity and mortality of patients requiring intubation, time to intubation, length of hospital stay, success rate of intubation, intubation attempts before success, and number of traumatic intubations. Although further research and implementation is warranted, Rolland, et al. present a strong argument for the utilization of AR in teaching endotracheal intubation among new trainees [15]. This skill can often be difficult to master and complicated by difficult airway anatomy and low respiratory reserve in the neonate. The proposed framework was capable of recording the motions of direct laryngoscopy of the manikin and the laryngoscope with the ability to produce a 3D visualization of the head-mounted display and extract data related to the kinematic multi-variate time series. The recorded motions were then evaluated and there was real-time visualization of the airway for situational awareness during the trial. This AR training used motion tracking, task trainer, visualization module, and motion processing to assess performance evaluation. This was communicated back to the trainee through interpretable visualization, augmented feedback, and see-through visualization of the airway in real-time. The study included 193 trials and 45 subjects and included attending neonatologists and paediatric residents to preserve diversity within the study. The study focused on the 20 quantitative outcomes of the tool more than individual trainee success rate. The accuracy of the dilated Convolutional Neural Networks (CNN) attention, the framework used, was found to be 84.6% accurate compared to 75.2%-79.5% accuracy of other methods. Therefore, the study found that the AR framework granted real-time feedback and augmented visualization, subsequently improving trainee awareness during intubation and accelerating acquisition of intubation skills [16].
Practice implications
For patient safety purposes, it is essential for all anesthesia providers to be able to correctly place an endotracheal tube. Proper endotracheal intubation prevents damage to tissue, limits the apneic and hypoxic time in patients, prevents prolonged intubation time and eliminates intubation failure [17]. By improving intubation skills and reducing the mentioned complications, anesthesia-related morbidity and mortality, hospital length of stay and total cost of healthcare are drastically reduced [17,18]. Therefore, it is advantageous to both the patient and healthcare organization to employ clinicians competent in the skill of endotracheal intubation. AR can assist new providers in achieving competency in this critical skill. In the simulation environment, students are currently exposed to plastic and latex manikins, which help them understand the step-wise sequence of intubation. However, a manikin presents a static environment and cannot accurately reproduce the dynamic airway challenges that may occur during intubation, such as unusual patient anatomies, oral secretions, blood, vomitus and other challenges unique to patients [18]. In addition to providing a more realistic experience for the student, AR allows for a better understanding of different patient populations and their anatomies, while simultaneously providing real-time feedback from faculty. The ability to download the AR airway app on any smartphone device improves access to high-quality learning experiences for students who lack access to non-traditional learning methods, such as those 21 residing in rural communities. The accessibility and virtual presence of AR can “leverage the advantage of dismantling geographic boundaries and connecting expertise to remote areas” [1]. While engaging in AR with the student, faculty members are able to sharpen their airway management skills and practice applying solutions while simultaneously teaching students. As a result, AR creates a better understanding for the students and more prepared clinicians in the hospital setting. Improving education for clinicians with AR training will result in safer care for patients, improved patient outcomes, decreased length of stay, reduced cost to the hospital and patient, and improved patient satisfaction.
Study design
Clinical question and project aim: This research project will answer the question of whether utilizing an airway app with augmented reality correlates to faster direct laryngoscopy intubation times compared to traditional learning modalities (i.e., manikins) in first-year SRNAs. This project aims to investigate the efficacy of an airway app with augmented reality in reducing time to intubation using direct laryngoscopy, thereby improving overall intubation and airway management skills.
Methods
The purpose of this project is to investigate the efficacy of an airway app utilizing Augmented Reality (AR) in reducing time to intubation with direct laryngoscopy, thereby improving airway management skills and subsequent intubation success among first-year SRNAs. The design approach for this doctoral project is best classified as an evidence-based intervention or quality improvement initiative. Ultimately, the goal of the project is to employ a novel education technique to improve intubation time, which improves patient outcomes and reduces the perioperative complications associated with prolonged apneic time. The primary data collected for this project is time to intubation, defined as the time required to insert the endotracheal tube through the vocal cords. This data will be collected using manikins at the enhanced Nurse Licensure Compact (NLC) and verification by researchers. Once the endotracheal tube is placed through the vocal cords, the student will verbalize to the researchers who will verify via direct laryngoscopy. To maintain continuity, the room will be set up the same way for each student and the same manikin will be utilized. The start time will begin when the student verbalizes readiness and the end time will conclude when the endotracheal tube is placed through the vocal cords and the student verbalizes successful intubation. The participants will first place an endotracheal tube using direct laryngoscopy, and the time will be recorded. The SRNA will then interact with the AR-assisted application, Airway Ex, on the iPad to enhance their understanding of the intubation process. After engaging with the application, the participants will place a second endotracheal tube, using direct laryngoscopy, in the manikin, and the time will be recorded. Comparing these two times will help assess the benefits of using AR in the training of the SRNA. Students will also have the opportunity to take a pre and post survey answering questions related to confidence, direct laryngoscopy skills, and understanding of airway anatomy [10]. The purpose of this survey is to assess if augmented reality engagement can improve confidence in SRNAs. Each student will randomly be provided a four-digit number that will serve as their identifier throughout the project. The student’s intubation times, as well as pre- and post-implementation survey results, will be recorded under their random identifier. This process will ensure the SRNA remains anonymous, and that the data remains unbiased. All data will be collected under the student identifier and stored on Microsoft Excel. This data will be collected and organized by the two researchers, Caroline Skelton and Mary Rachel Gutierrez, in a systematic way after each student has finished. By following a systematic approach to data collection, the opportunity for error is drastically reduced. The outcome measure of time to intubation reflects a dependent variable of the study and exhibits an interval level of measurement because time values are pre- established, constant and measurable. This outcome measure will be tested for reliability prior to project implementation. To test the reliability, the researchers will intubate the manikin ten times to verify the sensor accurately and consistently captures endotracheal intubation [17]. The validity of the measure is enhanced by the participant intubating the same manikin with the same equipment both before and after the intervention (Airway Ex). Although individual differences may exist between participant intubation techniques, the data collected remains valid due to the outcome measurement of individual time to intubation. The data will be collected, analysed and stored on Microsoft Excel to ensure it is protected and accessible only to the researchers involved. The most essential data analysis performed will be for statistical significance (p-value<0.05), which quantifies whether the results (time to intubation) were a product of the intervention (AR-based airway application).
Project management
Resources required for successful project implementation include an available simulation space, an intubating manikin with a built- in feedback system (i.e., force and motion sensors) to determine intubation success, multiple laryngoscope blades, an AR-based airway application (Airway Ex), technology to interact with the application (iPad), pre- and post-implementation surveys and a method of communicating with participants (i.e., text, email). The mentioned resources are already available for use by students (included in tuition dues); therefore, no additional costs will be incurred by the primary researchers. As a result, the creation of a formal budget is not necessary for this doctoral project. The primary researchers will utilize their personal technology devices (iPad) for communication and project implementation. In the setting of this project, key stakeholders include the SRNAs participants, faculty members of the nurse anesthesia program at Emory University and staff members at the enhanced Nurse Licensure Compact (eNLC) simulation space. Pending the results of the study, the Director and Assistant Director of the Nurse Anesthesia Program at Emory University, Dr. Kelly Wiltse-Nicely and Dr. Erica Moore, respectively, will be key stakeholders in incorporating the intervention (AR-assisted airway application) into the official SRNAs curriculum. Site support during project implementation will include the two researchers, Caroline Skelton and Mary Rachel Gutierrez, an eNLC staff member, and at least one Emory Doctor of Nursing Practice (DNP) Certified Registered Nurse Anesthetists (CRNA) simulation instructor or faculty member available to assist with equipment set-up or in the case of an unexpected malfunction.
The primary data collected for this project is time to intubation, defined as the time required to insert the endotracheal tube through the vocal cords before and after AR education, involving 15 study participants. Additionally, we employed descriptive statistical techniques to assess the pre- and post-AR surveys, which gauged the students’ experiences and confidence levels. For the time to intubation, the pre- and post-AR time in our study was non-parametric and the histograms followed a bell curve demonstrating normal distribution of the data (Figure 2). The median time pre-AR was 14.22 seconds and post-AR was 13.55 seconds, as presented in Table 1. Wilcoxon Signed Ranked Test with a two-tailed asymptotic sigma value of 0.394 indicated that these results are not statistically significant. Although there was an improvement in the time to intubation, it was not of statistical significance. For a more in-depth analysis, we generated a scatter plot (Figure 3), to assess the variations in time to intubation pre- and post-AR education among individual students. In general, most students demonstrated an improvement in their intubation times, but there were some outliers who did not show any significant improvement following AR education.
| N | Valid | Pre-AR | Post-AR |
|---|---|---|---|
| Missing | 15 | 15 | |
| 0 | 0 | ||
| Mean | 14.2573 | 13.8913 | |
| Median | 14.22 | 13.55 | |
| Std. Deviation | 3.12007 | 5.17832 | |
| Range | 10.37 | 18.14 | |
| Minimum | 9.49 | 6.23 | |
| Maximum | 19.86 | 24.37 | |
Table 1: Time to intubation pre- and post-Augmented Reality (AR).
Figure 2: Time to intubation pre-augmented reality education.
Note: A) Pre AR time; Mean=14.28; Std. Dev=3.12; N=15; B) Post AR time; Mean=13.89; Std. Dev=5.178; N=15.
Figure 3: Scatter plot pre- vs post- augmented reality education and direct
laryngoscopy time. 
Histogram of intubation times to assess for normalcy in our study group. Mild asymmetric distribution and small sample size (n=15) led to the selection of a non-parametric Wilcoxon test to assess statistical significance. This data displays an analysis of the intubation times before and after the AR education.
Blue signifies pre-AR intubation times and red signifies post- AR intubation times for each student. The X-axis represents each student so this chart evaluates time differences for individual students before and after AR education. When evaluating the survey results, we utilized descriptive analysis to examine the 5- point Likert scale survey. The results have been analysed and are presented in the frequency table (Table 2). For the first question, only 6.7% strongly agreed with their confidence in DL skills Pre-AR, compared to 40% after AR education. Regarding the understanding of airway anatomy during DL, 20% strongly agreed before AR education, which increased to 33% after AR education. When comparing traditional training methods to AR training, 80% of students either agreed or strongly agreed that traditional training adequately taught them about DL, while 86.7% agreed or strongly agreed that AR education enhanced their understanding of DL. Finally, 73.3% of students either agreed or strongly agreed that the AR and Airway Ex app was easy to learn and navigate [19].
| Pre-AR Survey | |||||
|---|---|---|---|---|---|
| I feel confident in my direct laryngoscopy skill | |||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 1 | 6.7 | 6.7 | 6.7 |
| 2.00 | 11 | 73.3 | 73.3 | 80.0 | |
| 3.00 | 2 | 13.3 | 13.3 | 93.3 | |
| 4.00 | 1 | 6.7 | 6.7 | 100.0 | |
| Total | 15 | 100.0 | 100.0 | ||
| I have a strong understanding of patient airway anatomy during direct laryngoscopy |
|||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 3 | 20.0 | 20.0 | 20.0 |
| 2.00 | 11 | 73.3 | 73.3 | 93.3 | |
| 3.00 | 1 | 6.7 | 6.7 | 100.0 | |
| Total | 15 | 100.0 | 100.0 | ||
| I feel that the current training modalities offered by Emory to teach direct laryngoscopy are outstanding | |||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 4 | 26.7 | 26.7 | 26.7 |
| 2.00 | 8 | 53.3 | 53.3 | 80.0 | |
| 3.00 | 1 | 6.7 | 6.7 | 86.7 | |
| 4.00 | 2 | 13.3 | 13.3 | 100.0 | |
| Total | 15 | 100.0 | 100.0 | ||
| Note: 1- strongly agree, 2- agree, 3- neutral, 4- disagree, 5- strongly disagree | |||||
| Post-AR Survey | |||||
| After engaging with the AR-based airway app, I feel more confident in my direct laryngoscopy skill |
|||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 6 | 40.0 | 40.0 | 40.0 |
| 2.00 | 6 | 40.0 | 40.0 | 80.0 | |
| 3.00 | 3 | 20.0 | 20.0 | 100.0 | |
| Total | 15 | 100.0 | 100.0 | ||
| After engaging with the AR-based airway app, I have a strong understanding of patient airway anatomy during direct laryngoscopy |
|||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 5 | 33.3 | 33.3 | 33.3 |
| 2.00 | 7 | 46.7 | 46.7 | 80.0 | |
| 3.00 | 3 | 20.0 | 20.0 | 100.0 | |
| Total | 7 | 100.0 | 100.0 | ||
| I feel that the AR-based airway app improved my understanding of direct laryngoscopy compared to traditional methods | |||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 3 | 20.0 | 20.0 | 20.0 |
| 2.00 | 10 | 66.7 | 66.7 | 86.7 | |
| 3.00 | 2 | 13.3 | 13.3 | 100.0 | |
| Total | 15 | 100.0 | 100.0 | ||
| The AR-based airway app was easy to learn and navigate |
|||||
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | 1.00 | 3 | 20.0 | 20.0 | 20.0 |
| 2.00 | 8 | 53.3 | 53.3 | 73.3 | |
| 3.00 | 4 | 26.7 | 26.7 | 100.0 | |
| Total | 15 | 100.0 | 100.0 | ||
Table 2: Frequency table for 5-point likert scale survey.
Limitations and future research suggestions
Numerous gaps in the literature were identified while conducting this study. At present, there is a major lack of prospectively randomized controlled trials in this area of research. Much of the current literature focuses on AR system development, rather than implementation. Furthermore, in studies that do evaluate AR implementation, there is an extensive range of AR systems and software that is utilized for training. This lack of consistency in AR systems used makes it difficult to directly compare studies and outcomes. For example, study investigators integrate AR using glasses, whereas some studies utilize a head-mounted projection device. Although these devices share a similar purpose, the technological nuances have the potential to affect outcomes. A proposed solution to this difference is to standardize the AR system used for endotracheal intubation [19]. In order to accomplish this standardization, further research, particularly larger prospective studies, must be conducted to determine the most accurate and effective software for the purpose of intubation. An additional gap identified in the literature is the lack of research on digital applications, such as an AR-based airway application (i.e., Airway Ex), to improve intubation skills among new trainees. In a world consumed by technology, integrating AR into a digital application for training purposes increases accessibility, ease of use and consistency in AR software. Many of the studies investigated in this study utilize some variation of AR head gear, which presents greater challenges related to cost and accessibility when compared to a digital application or even traditional learning modalities (plastic manikin).
Tracheal intubation is a fundamental skill that airway experts must master in order to ensure adequate ventilation of patients. Traditional education modalities may be inaccessible or inadequate in preparing novice students for DL with reduced time to intubation. The AR-based Airway Ex-application demonstrated an improvement in the time to intubation, albeit not statistically significant, likely attributable to the limited sample size. Secondary data revealed that the AR-based airway application improved the SRNAs confidence with intubation, understanding of patient airway anatomy, and overall understanding of the DL procedure. It is recommended to conduct additional research with a larger sample size to comprehensively assess the effectiveness of this teaching modality. Nonetheless, integration of an AR-based airway application into the formal training of SRNAs is a practical, cost-effective and highly accessible method of supplementing traditional learning modalities to improve intubation competency. This study emphasizes the future potential of AR technology to enhance traditional learning and improve intubation proficiency.
In the context of this project, the intervention of AR-assisted direct laryngoscopy does not directly impact human subjects, but instead plastic manikins. However, the participants of this project will be regarded with honesty, trust and respect by the researchers. The names and demographic profiles of the participants will remain anonymous, to protect against bias and potential conflicts of interest. Compliance with all regulatory and ethical obligations will be accomplished as deemed necessary by the Emory Institutional Review Board (EIRBs).
Not applicable.
All data generated or analysed during this study are included in this published article.
The authors declare that they have no competing interests.
Not applicable.
CS and RG developed, implemented and evaluated the project. Both authors read and approved the final manuscript.
Dr. Cathy Smiley-Naughton, DNP, CRNA; Dr. Katie Cole, DNP, CRNA; Dr. Russell Branch, DNP, CRNA; Dr. Shawana Moore, DNP, Advanced Practice Registered Nurse (APRN).
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Gutierrez MR, Skelton C, Smiley-Naughton C (2024) Time to Intubate Utilizing Traditional Learning vs. Airway App with Augmented Reality. J Perioper Med.7:229.
Received: 10-May-2024, Manuscript No. JPME-24-31307; Editor assigned: 13-May-2024, Pre QC No. JPME-24-31307 (PQ); Reviewed: 27-May-2024, QC No. JPME-24-31307; Revised: 03-Jun-2024, Manuscript No. JPME-24-31307 (R); Published: 10-Jun-2024 , DOI: 10.35841/2684-1290.24.7.229
Copyright: © 2024 Gutierrez MR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.