Family Medicine & Medical Science Research
Open Access
ISSN: 2327-4972
ISSN: 2327-4972
Research Article - (2020)Volume 9, Issue 1
Introduction: Delayed in the use of contraceptives following childbirth pose women at risk of pregnancy, which can lead to unintended pregnancy and short birth intervals. There are little evidences on timetouse modern contraceptives following childbirth. Therefore, this study aimed to estimate the time to use modern contraceptive and associated factors among women in extended postpartum period in Gondar town, northwest Ethiopia.
Methods: Institutional based cross sectional study was conducted from November, 2017 to October, 2018 in eight health institutions among postpartum women who came for infant measles immunization in Gondar town, northwest Ethiopia. A systematic random sampling technique was used to select 427 study participants. Data were analyzed using SPSS version 20. Kaplan–Meier survival curve was used to describe the time-to-use contraceptive. A Cox proportional hazards model was used to determine factors associated with time-to-contraceptive use.
Results: A total of 421 women were participated in this study. The median time to use modern contraceptive among women during the extended postpartum period was 6 (IQR: 5, 7) months. History of abortion (AHR=0.44, 95% CI: 0.25, 0.79), sexual resumption (AHR=3.29, (95% CI: 1.35, 8.03), menses resumption (AHR=1.46, 95% CI: (1.11, 1.92), getting family planning counseling during antenatal care (AHR=1.34, 95% CI: 1.02, 1.78) and husband approval (AHR=1.89, 95% CI:1.21, 2.96) were factors associated with time to contraceptive use in the extended postpartum period.
Conclusion: The time to modern contraceptive use during the extended postpartum period was delayed. Sexual and reproductive characteristics of postpartum women and male involvement in family planning were statistically significant predictors for timely use of modern contraceptive use. It is good to initiate contraceptive use before the return of menses.
Time; Modern contraceptive; Use; Postpartum period; Ethiopia
AHR: Adjusted Hazard Ratio; ANC: Antenatal Care; CI: Confidence Interval; EDHS: Ethiopian Demographic and Health Survey; EPP: Extended Postpartum Period; EPPFP: Extended Postpartum Family Planning; FP: Family Planning; PPFP: Postpartum Family Planning; PI: Principal Investigator; SPSS: Statistical Package for Social Science; WHO: World Health Organization
Maternal health problems remain a major global concern since pregnancy and childbirth are the leading causes of morbidity and mortality [1,2]. Avoidable morbidity and mortality remains a great challenge in many developing countries which account for approximately 99% of the global maternal deaths [3]. In Ethiopian, maternal mortality ratio was 412 per 100,000 live births [4].
Sexual resumption seems to occur earlier than menses and postpartum contraceptive use [5]. However, pregnancy can occur even before menses resumes [6]. Recent evidence in Ethiopia showed that 78.3% of postpartum women resumed sexual intercourse with a median time of 6 weeks with delayed initiation of contraception [7]. Birth interval of less than two years after the preceding birth is considered as short inter-pregnancy interval [8]. As evidences revealed short inter-pregnancy interval was associated with higher risks of pregnancy related complications and maternal mortality [9,10].
Postpartum family planning (PPFP) is crucial for the initiation and use of contraceptives within the first 12 months following childbirth [11,12]. As evidences showed, the mean time to return of ovulation was 45 to 94 days after delivery [6,13].Women are recommended to use contraceptives within 6 weeks after delivery [14]. However, the use of different contraceptives in the postpartum period depending on whether the woman is lactating or not in the time since delivery [15]. Therefore, addressing women’s contraceptives need during the postnatal period can prevent unintended pregnancy and short birth intervals [16,17].
Many reports have been published on the proportion and factors associated with postpartum modern contraception. However, studies are limited on the time to use modern contraceptive and associated factors in the extended postpartum period. Therefore, the aim of this study was to estimate the time to use modern contraceptive and associated factors among women in extended postpartum period in Gondar town, northwest Ethiopia. This is important for designing appropriate family planning interventional strategies as well as address the evidence gap on the time postpartum women takes to start using modern contraceptives following childbirth.
Study design period and setting
Institutional based cross sectional study was conducted from November, 2017 to October, 2018. The study was conducted in eight public health institutions of Gondar town namely: Gondar University Comprehensive Specialized Hospital, Gondar health center, Maraki Health Center, Azezo Health Center, Azezo Tekele haymanot Health Post, Loza health post, Sabia health post and Lay Teda Health Post. The town is located in North Gondar Zone of the Amhara Regional State which is 750 Km far from Addis Ababa, capital city of Ethiopia, to northwest. According to Gondar city Health department office, Gondar town has a population of 78,546 women in the reproductive age group [18]. Gondar town has one comprehensive specialized hospital, eight governmental health centers and 14 rural health posts that are providing maternal and other health services to the community.
Source and study population
The source population was all reproductive age women in extended postpartum period in Gondar town, northwest Ethiopia, while all reproductive age women in extended postpartum period who were attending health facilities for measles vaccination for their infant during data collection period was the study population. Women who come out of the catchment area for infant vaccination and women who brought children for vaccinations are guardians or relatives were excluded from the study.
Sample size determination and sampling procedure
STATA version 14 was used to calculate the sample size for proportional hazard regression model by taking 80% power, 5% level of significance and standard deviation of 0.5. From previous study done in Uganda [19], the overall rate of contraceptive use (22.2%) and hazard ratio (1.83) were considered to calculate the sample size. Finally, the total sample size with 10% non-response rate was 427.
A systematic random sampling technique was used by considering the eight health institutions immunization clinics on average gave immunization service for children per day. The sampling interval was obtained by dividing the number of postpartum women per health facility which was allocated proportionally to the level of immunization service. The sampling interval was calculated to be two. The first study participant was selected by lottery method and the next study participants were chosen at regular intervals (every 2nd interval) and interviewed by data collectors.
Variables of the study
Time-to-contraceptive use was the dependent variable, which was measured in months, by the period from six weeks following a birth to the time when a woman used modern contraception.
The independent variables were included sociodemographic factors (age, religion, marital status, educational level, residence, occupation, husband education, wealth status, reproductive health factors (number of live children, birth interval, sex of child, mode of delivery, menstrual resumption, sexual resumption, fertility desire, breast feeding status, abortion history), health service related factors (antenatal care visits, postnatal care visit, place of delivery, family planning counseling during antenatal care, family planning counseling during postnatal care) and knowledge related factors (discussion on contraceptive use, husband approval, exposure to media, knowledge about contraceptives).
Data collection tools and procedures
The data was collected though interviewer administered technique by using a structured and pretested questionnaire which was developed in English by reviewing different literatures [19-24]. The questionnaire includes socio-demographic characteristics of women as well as other potential factors affecting time to modern contraceptive use. Eight trained diploma female midwifes as data collectors and two BSC nurses as supervisors were involved in the data collection process.
To keep the data quality training was given for data collectors and supervisors; local language was used during data collection and pre-tested the questionnaire. Furthermore, the collected data was checked for completeness, consistency, accuracy and clarity by the principal investigator on a daily basis.
Operational definition
Contraceptive status (yes): If women used modern contraceptive within the first 9 months of following child birth.
Contraceptive status (no): If women did not used modern contraceptive from six weeks following a birth to 9 months of following childbirth.
Data management and analysis
The data was entered into Epi-info version 7.2.2.2 and exported to SPSS version 20 Software for analysis. Descriptive statistics was employed to characterize the study population using frequencies and proportions. Kaplan-Meier survival curves were used to describe the time-to-contraceptive use. Bivariable and multivariable Cox proportional hazards model was used to assess the independent factors associated with time-to-contraceptive use. Variables with p-value ≤ 0.2 in the bivariable analysis were fitted in the multivariable analysis.
The final model was checked for satisfying the assumption of proportionality with time dependent Cox model and graphically by log-log hazard plot, and the proportional hazard assumption was not violated. Cox and Snell’s residual analysis was also used to check the model fitness. Adjusted Hazard ratio (AHR) with 95% confidence interval (CI) was calculated to estimate the strength of association between independent predictors and time to use of modern contraceptive. P value ≤ 0.05 was considered statistical significance.
Socio-demographic characteristics of study participants
A total of 421 mothers were responded completely for the study making response rate of 98.6%. Out of the total study participants 372 (88.4%) were urban dwellers. The age range of the respondents was 18-50 years. The mean age of the mothers was 28.20 (± 5.4 SD) years with more than half, 225 (53.4%), of them were in the age range of 25-34 years. The majority, 407 (96.7%), were married and 360 (85.5%) were orthodox followers in religion. Regarding to educational status, 162 (38.5%) of the study participants attended secondary school. About 179 (44%) respondents’ husband attended higher education (Table 1).
| Variables | Number | Percent |
|---|---|---|
| Age | ||
| 18-24 | 136 | 32.2 |
| 25-34 | 225 | 53.4 |
| ≥ 35 | 60 | 14.3 |
| Marital status | ||
| Married | 407 | 96.7 |
| Other (single, divorced and widowed) | 14 | 3.3 |
| Religion | ||
| Orthodox | 360 | 85.5 |
| Muslim | 55 | 13.1 |
| Protestant | 6 | 1.4 |
| Residence | ||
| Urban | 372 | 88.4 |
| Rural | 49 | 11.6 |
| Educational level | ||
| No formal education | 68 | 16.2 |
| Primary school | 67 | 15.9 |
| Secondary school | 162 | 38.5 |
| Higher education | 124 | 29.4 |
| Occupation | ||
| Housewife | 273 | 64.9 |
| Government employee | 49 | 11.6 |
| Private employee | 75 | 17.8 |
| Merchant | 14 | 3.3 |
| Others (Daily laborer, student, Tella sellers) | 10 | 2.4 |
| Husband’s education status (N=407) | ||
| No formal education | 53 | 13 |
| Primary school | 57 | 14 |
| Secondary school | 118 | 29 |
| Higher education | 179 | 44 |
| Husband’s occupation (N=407) | ||
| Farmer | 23 | 5.7 |
| Government employee | 151 | 37.1 |
| Private employee | 103 | 25.3 |
| Merchant | 83 | 20.4 |
| Daily laborer | 36 | 8.8 |
| Others(Driver, student, job seekers) | 11 | 2.7 |
| Wealth status | ||
| Lowest | 35 | 8.3 |
| Second | 134 | 31.8 |
| Middle | 70 | 16.6 |
| Fourth | 94 | 22.4 |
| Highest | 88 | 20.9 |
Table 1: Nelson-Alian cumulative hazard curve for the final model containing Cox-Snell residuals.
Reproductive characteristics of study participants
The average number of alive children per woman was 2.2. Among the study participants 33 (7.8%) and 89 (21.1%) were ever experienced abortion and caesarean section respectively. About of the respondents 123 (29.2%) have had more than three years gap between the previous and current birth. Majority, 395 (93.8%) of the current births were planned, and 193 (45.8%) want another child after 2 years and 181 (68.3%) of the mothers planned to have one to two more number of children. Almost all 412 (97.9%) of study participants had received ANC service at least once. About 399 (94.8%) of mothers gave birth to their current child in governmental and private health institutions. Three hundred twenty-two (94.4%) and 268 (65%) respondents had family planning counseling during postnatal period and ANC respectively. The majority, 406 (96.4%) of respondents were currently breastfeeding their infant. Of the study participants, 373 (88.6%) practiced exclusive breast feeding. About half, 214 (50.8%) of the respondents had resumed mensus and 387 (91.9%) of the study participants have already resumed sexual intercourse (Table 2).
| Variables | Number | Percent |
|---|---|---|
| Parity | ||
| 1 | 149 | 35.4 |
| 2-4 | 253 | 60.1 |
| ≥ 5 | 19 | 4.5 |
| Abortion | ||
| Yes | 388 | 92.2 |
| No | 33 | 7.8 |
| Alive children by now | ||
| 1 | 152 | 36.1 |
| 2-3 | 212 | 50.4 |
| ≥ 4 | 57 | 13.5 |
| Gap between the previous and current birth | ||
| It is my first child | 149 | 35.4 |
| <24 months | 85 | 20.2 |
| 24-36 months | 64 | 15.2 |
| >36 months | 123 | 29.2 |
| Ever had caesarean section | ||
| Yes | 89 | 21.1 |
| No | 332 | 78.9 |
| Mode of delivery for current child | ||
| Spontaneous vaginal delivery | 338 | 80.3 |
| Caesarean section | 83 | 19.7 |
| Sex of current child | ||
| Male | 226 | 53.7 |
| Female | 195 | 46.3 |
| Feeding option for the current child | ||
| Exclusive breast feeding | 373 | 88.6 |
| Mixed feeding | 48 | 11.4 |
| Breastfeed currently | ||
| Yes | 406 | 96.4 |
| No | 15 | 3.6 |
| Is the present birth was planned? | ||
| Yes | 395 | 93.8 |
| No | 26 | 6.2 |
| Sexual intercourse resumed after recent birth | ||
| Yes | 387 | 91.9 |
| No | 34 | 8.1 |
| Menstruation resumed after recent birth | ||
| Yes | 214 | 50.8 |
| No | 207 | 49.2 |
| Future reproductive plan | ||
| Want no more children | 94 | 22.3 |
| Want another child within 2 years | 11 | 2.6 |
| Want another child after 2 years | 193 | 45.8 |
| Undecided | 123 | 29.2 |
| Previous use of contraceptive | ||
| Yes | 405 | 96.2 |
| No | 16 | 3.8 |
| Number of planned children (N=265) | ||
| 1-2 | 181 | 68.3 |
| ≥ 3 | 84 | 31.7 |
| ANC follow up | ||
| Yes | 412 | 97.9 |
| No | 9 | 2.1 |
| Number of ANC visit | ||
| 1-3 visits | 56 | 13.6 |
| 4 and above | 356 | 86.4 |
| FP counseling during ANC (N = 412) | ||
| Yes | 268 | 65 |
| No | 144 | 35 |
| Place of delivery | ||
| Health facility | 399 | 94.8 |
| Home | 22 | 5.2 |
| Postnatal care | ||
| Yes | 341 | 81 |
| No | 80 | 19 |
| Number of PNC visit (N=341) | ||
| 1-2 visits | 249 | 73 |
| 3 and above | 92 | 27 |
| FP counseling during PNC (N = 341) | ||
| Yes | 322 | 94.4 |
| No | 19 | 5.6 |
Table 2: Reproductive health-related characteristics of mothers of extended postpartum period, Gondar city, northwest Ethiopia, 2019.
Time-to-contraceptive use
The prevalence of modern contraceptive use among women in the extended postpartum period was 281 (66.7%) with 95% CI (62.2, 71.0). The median time to use modern contraceptive among women during the extended postpartum period was 6 months (IQR: 5, 7) (Figure 1).
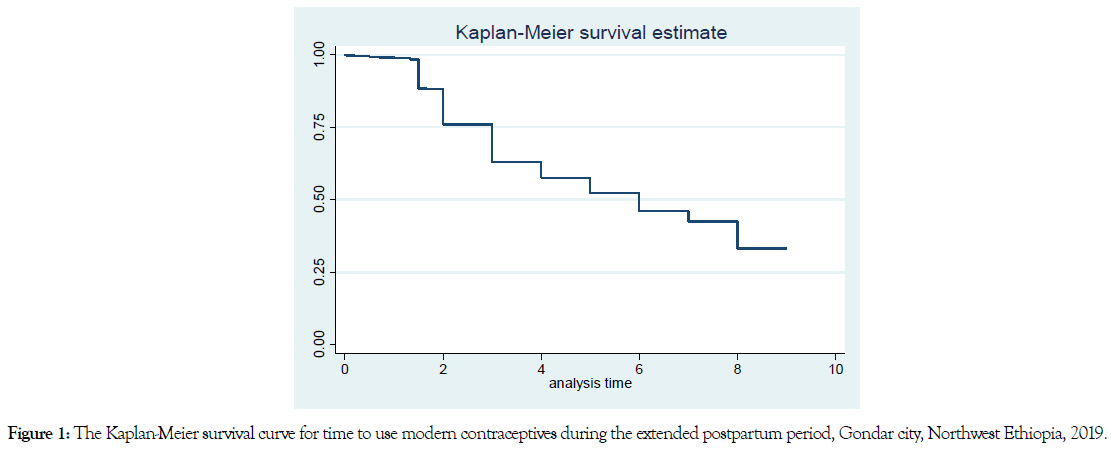
Figure 1. The Kaplan-Meier survival curve for time to use modern contraceptives during the extended postpartum period, Gondar city, Northwest Ethiopia, 2019.
Kaplan-Meier curves that show the survival estimates of modern contraceptive use for selected factors
The Kaplan Meier curve displayed below shows, the estimated difference in survival status of women based on selected variables (Abortion history, Mensus resumption, Husband approval on contraceptive use and Sexual resumption) (Figure 2).
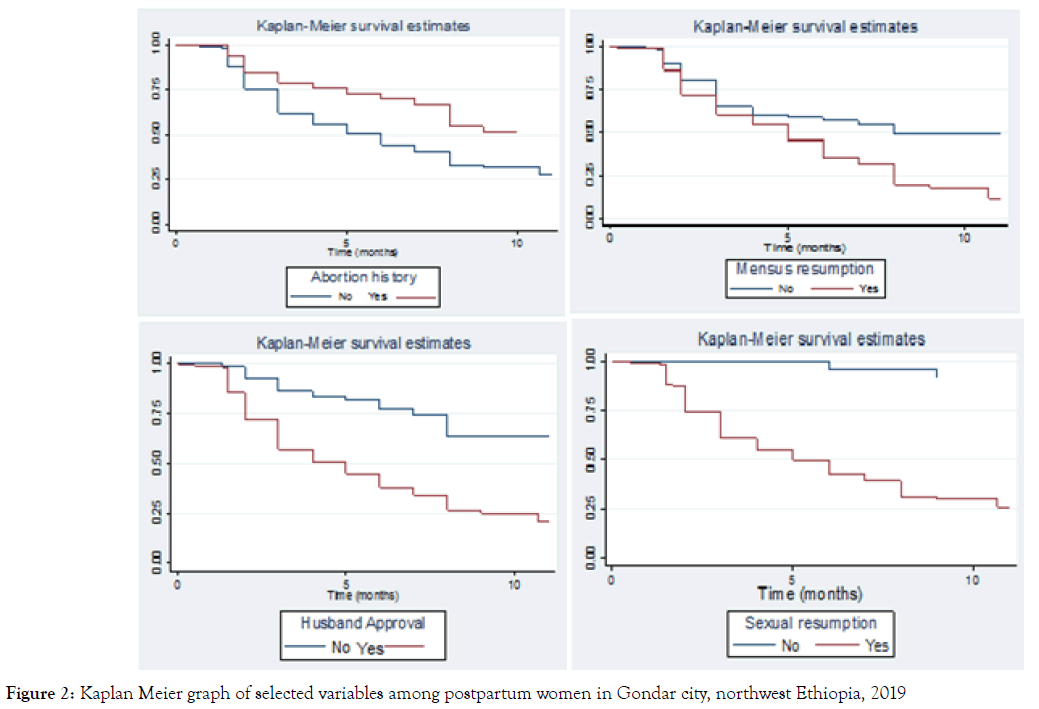
Figure 2. Kaplan Meier graph of selected variables among postpartum women in Gondar city, northwest Ethiopia, 2019
Factors affecting time-to-contraceptive use
In multivariable analysis abortion experience, sexual resumption, menses resumption, FP counseling during ANC and husband approval remained statistically significant with time to modern contraceptive practice during the extended postpartum period.
Postpartum women whose menses had returned were about 1.46 times more likely to start contraceptive use early in the extended postpartum period as compared to those who were amenorrheic (AHR= 1.46, 95% CI: 1.11, 1.92).
The likelihood of shorter time-to-use of modern contraceptives in the extended postpartum period was 3.29 times higher among postpartum woman who started sexual activity as compared with abstainers (AHR= 3.29, 95% CI: 1.35, 8.03). In women who had history of abortion, the time to use modern contraceptive was delayed by 56% as compared to those who had not have abortion experience (AHR= 0.44, 95% CI: 0.25, 0.79).
FP counseling during ANC was positively associated with time to modern contraceptive use after childbirth. Mothers who were received counseling service about family planning during last pregnancy were 1.34 times more likely to use modern contraceptive earlier than mothers who weren’t counseled (AHR= 1.34, 95% CI: 1.02, 1.78).
Husband approval of contraceptive use was also found to be one of the predictors of time to contraceptive use in the extended postpartum period. The rate of using modern contraceptive was 1.89 times shorter among woman whose husbands approved for contraceptives initiation than those whose husbands did not approve contraceptive use (AHR= 1.89, 95% CI:1.21, 2.96) (Table 3).
| Variables | Use of contraceptives | Hazard Ratio (95% CI) | ||
|---|---|---|---|---|
| Yes | No | Unadjusted (CHR) | Adjusted(AHR) | |
| Age | ||||
| 15-24 | 101 | 35 | 1.32(0.90, 1.90) | 1.32(0.53, 3.26) |
| 25-34 | 142 | 83 | 1.02(0.71, 1.46) | 1.26(0.55, 2.91) |
| ≥ 35 | 38 | 22 | 1 | 1 |
| Residence | ||||
| Urban | 255 | 117 | 1.58(1.06, 2.37) ** | 1.62(0.93, 2.82) |
| Rural | 26 | 23 | 1 | 1 |
| Educational level | ||||
| No formal education | 35 | 33 | 0.63 (0.42, 0.93) ** | 0.95 (0.39, 2.34) |
| Primary school | 42 | 25 | 0.84 (0.58, 1.23) | 0.88 (0.50, 1.55) |
| Secondary school | 116 | 46 | 1.03 (0.78, 1.37) | 0.99 (0.66, 1.52) |
| Higher education | 88 | 36 | 1 | 1 |
| Parity | ||||
| 1 | 107 | 42 | 1.60 (0.84, 3.06) | 1.06 (0.74, 1.53) |
| 2-4 | 164 | 89 | 1.33 (0.70, 2.52) | 0.35 (0.11, 1.15) |
| ≥ 5 | 10 | 9 | 1 | 1 |
| Alive children by now | ||||
| 1 | 110 | 42 | 1.48 (1.01, 2.18) ** | 3.09 (0.71, 13.40) |
| 2-3 | 138 | 74 | 1.23 (0.84, 1.80) | 0.97 (0.39, 2.44) |
| ≥ 4 | 33 | 24 | 1 | 1 |
| Abortion history | ||||
| Yes | 16 | 17 | 0.57 (0.34, 0.95) ** | 0.44 (0.25, 0.79) ** |
| No | 265 | 123 | 1 | 1 |
| Breastfeed currently | ||||
| Yes | 275 | 131 | 1.88 (0.84, 4.23) | 1.43 (0.56, 3.66) |
| No | 6 | 9 | 1 | 1 |
| Is the present birth was planned? | ||||
| Yes | 269 | 126 | 1.80 (1.01, 3.22) ** | 0.68 (0.46, 1.03) |
| No | 12 | 14 | 1 | 1 |
| Sexual activity resumed | ||||
| Yes | 275 | 112 | 6.14 (2.73, 13.8) ** | 3.29 (1.35, 8.03) ** |
| No | 6 | 28 | 1 | 1 |
| Menstruation resumed | ||||
| Yes | 176 | 38 | 1.94 (1.53, 2.48) ** | 1.46 (1.11, 1.92) ** |
| No | 105 | 102 | 1 | 1 |
| FP counseling during ANC | ||||
| Yes | 191 | 77 | 1.33 (1.04, 1.72) ** | 1.34 (1.02, 1.78) ** |
| No | 88 | 56 | 1 | 1 |
| Place of delivery | ||||
| Health facility | 269 | 130 | 1.50 (0.84, 2.67) | 0.75 (0.29, 1.91) |
| Home | 12 | 10 | 1 | 1 |
| FP counseling during PNC | ||||
| Yes | 228 | 94 | 1.99 (1.03, 3.89) ** | 1.50 (0.53, 4.23) |
| No | 9 | 10 | 1 | 1 |
| Knowledge on FP | ||||
| Yes | 178 | 74 | 0.80 (0.63, 1.02) | 1.01 (0.64, 1.56) |
| No | 103 | 66 | 1 | |
| Husband approval | ||||
| Yes | 257 | 84 | 3.03 (1.99, 4.62) ** | 1.89 (1.21, 2.96) ** |
| No | 24 | 42 | 1 | 1 |
| Discussion with husband on contraceptive | ||||
| Yes | 50 | 59 | 0.47 (0.35, 0.64) ** | 1.13 (0.59, 2.16) |
| No | 231 | 81 | 1 | 1 |
| Wealth Index | ||||
| Lowest | 24 | 11 | 1.25 (0.77, 2.03) | 1.97 (0.94, 3.48) |
| Second | 85 | 49 | 1.02 (0.73, 1.44) | 1.09 (0.75, 1.60) |
| Middle | 48 | 22 | 1.20 (0.78, 1.69) | 1.08 (0.71, 1.66) |
| Fourth | 67 | 27 | 1.31 (0.92, 1.87) | 1.13 (0.76, 1.68) |
| Highest | 55 | 33 | 1 | 1 |
Table 3: Bivariable and Multivariable Cox regression analysis for factors associated with time to use of modern contraceptives during the extended postpartum period, Gondar city, Northwest Ethiopia, 2019.
Goodness of fit of the final model
The fit of the model was evaluated by using the Cox-Snell residuals with fitting the model. Finally, the Nelson- Aalen cumulative hazard function plot was seen to compare the hazard function to the diagonal line (Figure 3).
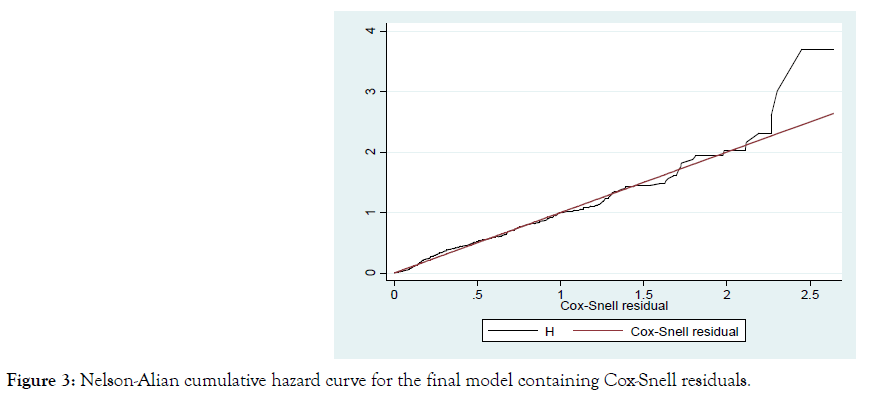
Figure 3. Nelson-Alian cumulative hazard curve for the final model containing Cox-Snell residuals.
This study was conducted to estimate the time to modern contraceptive use of women in the first year after delivery. The study revealed that the median time to use modern contraceptive among women during the extended postpartum period was 6 months (IQR: 5, 7). This finding is in line with study conducted in Kenya [5] which reported the median time to contraceptive use after childbirth was 7 months. This finding indicatedthata number of women is at a high risk of unwanted or unplanned pregnancies; because of late initiation of contraceptive use which is much delayed than WHO recommendation [14]. This study revealed a delay in the initiation of contraceptive use after childbirth in contrast with studies done in Gozamen district, northwest Ethiopia (3.2 months meantime to start contraceptive use) [22] and Kebribeyah town, eastern Ethiopia (2-3 months of mean time to start contraceptive use) [20]. This difference might be due to statistical analysis method variation, as these studies were calculated the mean as measure of average for time of contraceptive initiation after childbirth. However, this finding revealed shorter initiation of contraceptive use than the studies conducted in Zambia [25] and Uganda [19] which documented 8 and 19 months of median time to contraceptive respectively. The reason might be due to target population variation, as the studies in Zambia and Uganda were include women who had a birth within the five and two years respectively; that increased the median time to modern contraceptive use after childbirth. On the other hand, this study excluded women who gave birth 9 months and above prior to the study.
In this study, the prevalence of modern contraceptive among women in the extended postpartum period was found to be 66.7% with 95% CI (62.2, 71.0). This finding was higher than that of studies conducted among postpartum women in India (15%) [26], Nigeria (8.32%) [27], Uganda (28%) [28] and Dabat district, northwest (10.3%) [21]. The possible explanation for this variation may be due to difference in the study setting; this study was conducted among postpartum women who came to a health institution for infant immunization and such participants could have an opportunity to obtain health education. This finding is in line with a study conducted in Ganta-Afeshum district, Tigray, northern Ethiopia (68.1%) [29]. However, this finding is lower than the study carried out in Addis Ababa, Ethiopia (80.3%) [23]. This difference might be due to difference in study area; the study in Addis Ababa was done among urban residents, and such participants could have better access to information and health education than rural women.
This study showed that resuming sexual activity was positively associated with time to modern contraceptive use (AHR=3.29, (95% CI: 1.35, 8.03). This finding is consistent with other studies carried out in Kenya (5), Northern Ethiopia [30] and Gondar town [24]. The possible reason for this may be that women may perceive themselves to be at risk for unwanted or unintended pregnancy when they resume sexual activity following childbirth and that motivates them to start contraceptive use [13].
Women whose menses returned after childbirth were about 1.46 times more likely to start contraceptive use early in the postpartum period (AHR= 1.46, 95% CI: 1.11, 1.92). The reason for this may be that menses resumption may make women be aware of their fertility returning, which motivates them to start contraceptive use early. Moreover, different studies indicated that menses returning after birth was found to be stimulating factor affecting the use of modern contraceptives in the postpartum period, and the absence of menses as main factor for not using modern contraceptives during the extended postpartum period [13,24,31]. This finding is consistent with studies done in Addis Ababa [23], Gozamen district [22] and Gondar town, northwest Ethiopia [32].
The present study revealed a significant difference in time to contraceptive use among postpartum women based on their abortion history. Women who had history of abortion were 56% longer time to start modern contraception as compared to those who had not an abortion experience (AHR= 0.44, 95% CI: 0.25, 0.79). This might indicate that post abortion modern contraceptives access is poor. This is also likely because; majority 19 (51.4%) of respondents among postpartum women who had abortion experience had spontaneous abortion which mean they might have had fertility intention.
Mothers who were received counseling service about family planning during pregnancy had a shorter time-to-contraceptive use compared with their counterparts (AHR=1.34, 95% CI: 1.02, 1.78). This finding was supported by a study conducted in Kenya and Zambia [25]. The possible reasons for this may be that counseling during ANC would create an opportunity for women to have more exposure of information and awareness regarding birth spacing by the use of contraceptive after giving each birth [17].
This study showed that husband approval of contraception significantly affects the time to use of contraceptives following childbirth (AHR=1.89, 95% CI: 1.21, 2.96). This is in line with a study conducted in Zambia [25], Gozamen District [22], and Gondar town [24] northwest Ethiopia. The reason for this finding could be the fact that decisions made jointly with agreement of both couples will have better outcome regarding the use of postpartum contraceptives as compared with decision made by only one side since issue of family planning is not only the concern of one partner [4].
This study adds to the currently limited body of evidence of the time to modern contraceptive use after childbirth. However, it has some limitations: respondents might have recall bias on certain variables; health service providers’ related factors and communitylevel factors that were not measured.
This study indicated that modern contraceptive use following childbirth was delayed. Determinant factors that positively associated with time to use modern contraceptive use were sexual resumption, menses resumption, FP counseling during ANC and husband approval. Health education should be provided on fertility return behaviors, and initiation of contraception before the return of menses or sexual activity. It is better to provide counseling about family planning service for women during their ANC visit. Counseling of husbands about the early use of postpartum contraception should be provided. It is possible that researchers could identify health service providers’ related and community-level factors that can influence time to postpartum modern FP practice.
Ethical approval
Ethical clearance was obtained from the Institutional Review Board (IRB) of University of Gondar, College of Medicine and Health Sciences, Institute of Public Health. Formal letters of cooperation were written to the different health institutions in Gondar Town and Gondar Worde Health Offices. Head of each health facilities were also write letter of permission to the immunization focal person. The benefit of the study was explained to the respondents Participants were informed that they had the right to withdraw from the study at any time and also, informed verbal consent was received from the participants before interviewing them. The study participants were interviewed in separate room keeping their privacy and confidentiality of the information was maintained by excluding personal identifiers in the questionnaire.
The authors acknowledge the Institute of Public Health, College of Medicine and Health Sciences, University of Gondar. The authors would also like to thank all each health facility staffs, data collectors, supervisors and all mothers who participated in this study for their commitment in responding to the interviews.
Availability of data and material
The datasets used and analyzed during the current study are available from the corresponding author.
Authors' contributions
BDM wrote the proposal, participated in data collection, analysis, report writing and drafted the manuscript. AAG and AML made revisions on proposal, participated in data analysis and drafted the manuscript. All authors reviewed, revised and approved the manuscript for publication.
Competing interests
The authors declare that they have no competing interests.
Citation: Mekonnen BD, Gelagay AA, Lakew AM (2020) Time to Use Modern Contraceptives and Associated Factors among Women in Extended Postpartum Period in Gondar City, Northwest Ethiopia. Fam Med Med Sci Res 9: 243.
Received: 24-Jan-2020 Accepted: 10-Feb-2020 Published: 17-Feb-2020 , DOI: 10.35248/2327-4972.20.9.243
Copyright: © 2020 Mekonnen BD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.