Endocrinology & Metabolic Syndrome
Open Access
ISSN: 2161-1017
ISSN: 2161-1017
Research Article - (2015) Volume 4, Issue 3
The increased prevalence of overweight and obesity has been exponential in recent years and involves all age groups, including children and adolescents [1]. Obesity and insulin resistance determine metabolic disturbances that are deleterious to the vascular system and other tissues, accelerating the atherosclerotic process [2,3] and increasing the risk of other diseases such as high blood pressure (hypertension), dyslipidemia, diabetes type 2 non-alcoholic fatty liver disease, bone disease and even depression [1,4].
It has also been shown an association between insulin resistance and hyperinsulinemia with increased prevalence of thyroid nodules and enlargement of the thyroid gland [5], which would be related to the goitrogenic action of insulin and insulin-like growth (insulin-like growth factor I). Controlling obesity contributes greatly to reverse these processes by reducing insulin resistance and compensatory hyper-insulinemia.
Therefore, early detection is important for high-risk patients to intervene in a timely manner and avoid the introduction of such diseases, thus reducing future morbidity and mortality. In order to establish the prevalence of heterogeneous thyroid ultrasound and its association with hyper-insulinism we perform the following study in a population of children and adolescents with overweight and obesity.
A cross-sectional study was conducted in 50 children and adolescents aged 2 to 14 years referred to the Service of Endocrinology of the Hospital Provincial del Centenario for overweight or obesity, between March 2011 and May 2012.
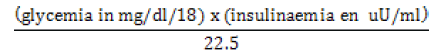
The following variables were analyzed: weight, height, Body Mass Index (BMI), acanthosis nigricans, fasting blood glucose, insulin, HOMA index, total cholesterol, HDL-cholesterol, triglycerides, liver transaminases (GTP-GOT), TSH, FT4, microsomal antibodies, thyroglobulin antibodies. Thyroid ultrasound was also requested, which were all made by the same observer [6-8]. The IR HOMA estimated insulin resistance by fasting glucose and insulin. For the calculation the following formula [9] was applied:
Overweight was defined as the presence of BMI ≥ 85 percentile for age and sex, and obesity BMI ≥percentile 97para sex and age [9]. Hyperinsulinism was defined as the presence of fasting insulin level ≥15 mIU/ ml [10]. Heterogeneous thyroid ultrasound was considered those who had solid nodules, pseudonódulos, cysts or anatomic abnormalities of the thyroid gland [5,6].
All patients were evaluated in clinical endocrinology deparment and anthropometric data obtained. To determine obesity according to BMI charts of the World Health Organization were used. BMI was calculated by the following formula: weight/height [2]. Laboratory tests were performed in the central laboratory of the Hospital. All patients were fasting. Of the parameters evaluated in this study we analyzed the relationship between hyper-insulinemia and heterogeneous thyroid ultrasound scans, to try to correlate the same relationship shown in the adult population.
Statistical analysis
The association between dependent and independent (predictor) variables were evaluated using univariate by χ2 test or Fisher exact test, as it corresponded. ORs and confidence intervals of 95% were calculated. Associations were considered significant at P<0.05. The calculations were performed with the program SPSS versión 22.
Descriptive results
Variables in Table 1 are analyzed and described (Table 1). Of all the children we studied the presence of acanthosis nigricans was found (as an indirect sign of hyper-insulinemia) in 26 of them (52%) (Figure 1). Insulin levels were assessed finding hyperinsulinism (≥15) in 31 children (62%) (Figure 2)
| Variable | N Validate | Average | Standard deviation | Median | Mínimum | Máximum | Quartile | ||
|---|---|---|---|---|---|---|---|---|---|
| 25 | 50 | 75 | |||||||
| Age | 50 | 9.8 | 3.0 | 10 | 2 | 14 | 8 | 10 | 12 |
| Wight | 50 | 54.6 | 17.0 | 55.5 | 21.0 | 95.2 | 40.3 | 55.5 | 67.1 |
| Height | 50 | 141.8 | 17.4 | 145.0 | 96.0 | 169 | 132.0 | 145.0 | 156.0 |
| IMC | 50 | 26.3 | 3.5 | 25.3 | 20.3 | 36.5 | 24.0 | 25.3 | 28.6 |
| Glycemia | 50 | 89.0 | 10.2 | 88.5 | 68.0 | 111 | 81.5 | 88.5 | 96.3 |
| Insulinemia | 50 | 23.3 | 16.8 | 19.0 | 6.0 | 82 | 12.7 | 19.0 | 25.2 |
| HOMA | 50 | 5.5 | 4.6 | 4.0 | 1.1 | 22 | 2.8 | 4.0 | 6.2 |
| TSH | 49 | 5.1 | 2.9 | 5.1 | 1.1 | 17.6 | 2.8 | 5.1 | 6.6 |
| T4 Free | 47 | 1.3 | 0.2 | 1.2 | 0.8 | 1.78 | 1.1 | 1.2 | 1.5 |
| Total cholesterol | 50 | 150.5 | 28.1 | 150.5 | 87.0 | 221 | 133.5 | 150.5 | 169.3 |
| HDL cholesterol | 45 | 46.6 | 21.5 | 43.0 | 15.0 | 132 | 32.5 | 43.0 | 52.5 |
| Triglycerides | 49 | 93.1 | 42.7 | 88.0 | 32.0 | 226 | 61.5 | 88.0 | 123.5 |
| TGO | 45 | 24.0 | 9.9 | 21.0 | 13.0 | 67 | 18.5 | 21.0 | 27.5 |
| TGP | 45 | 24.0 | 15.7 | 21.0 | 6.0 | 86 | 15.0 | 21.0 | 27.0 |
Table 1: List of the variables analyzed.
As part of the paper we study the percentage of children with positive thyroid antibodies: the microsomal antibodies tested (n 42) were positive in 4 children (Figure 3); and thyroglobulin (n 41) had the same positivity of just 2 (Figure 4); and we evaluate its relationship with the heterogeneity or ultrasound (Table 2).
| AMA | Thyroid ultrasound | Total | |
|---|---|---|---|
| Homogeneous | Heterogeneous | ||
| Negative | 33 | 5 | 38 |
| Positive | 1 | 3 | 4 |
| Total | 34 | 8 | 42 |
Note: Fisher exact test p=0.017 (sig). AMA: Antibody antimicrosomal.
Table 2: Relationship between antibody positive and heterogeneity of thyroid ultrasound.
As a result of a survey conducted in children and adolescents are overweight or obese (n 50) is evaluated as part of the existence of insulin resistance and its relationship with the presence of heterogeneous thyroid ultrasound [6-8]. 50 thyroid ultrasound, all made by the same observer (sonographer physician), and heterogeneity of the gland was found in 10 patients (20%) were performed (Figure 5).
Of all thyroid ultrasound (n 50) that were performed in this study, the presence of nodules was observed in 5 of them (10%). They can be divided according to US pattern in 2 cysts (40%), 2 solid nodules (40%) and one pseudo-node (20%) (Figures 6 and 7)
Variable insulin resistance (considering HOMA index) taking the following values are defined:
- No HOMA insulin resistance when the variable is <3 and insulin <15.
- Insulin resistance when the variable is Homa insulin ≥ 3 or ≥15.
36 children had insulin resistance (assessed by HOMA) positive (72%) (Figure 8).
Analytical analysis
You want to analyze the relationship between the variable “Thyroid Ultrasound” and other variables. For quantitative variables, and recalling that N=50, the Mann-Whitney U test is applied, it is a nonparametric test applied to two independent samples. The null hypothesis of is that two samples come from populations continuous identical and the alternative hypothesis assumes that the central tendency (median) of a population differs from the other (Table 3).
| Variable | p-associated | Signification |
|---|---|---|
| Insulinaemia | 0.003* | Significant |
| HOMA | 0.014* | Significant |
| TSH | 0.02* | Significant |
| T4 Free | 0.013* | Significant |
Table 3: Relationship between variables.
The other variables did not present statistical significance. Of the patients who had ultrasound pattern heterogeneous (n 10), defined it by the presence of thyroid nodules or anatomical changes in the gland, it showed that 90% of them had hyperinsulinism (n 9), Fisher exact test=p=0.037 (significant) (Table 4 and Figures 9 and 10). We studied the relationship between heterogeneous thyroid ultrasound and HOMA index. (Table 5 and Figure 11). 100% ultrasound showed heterogeneous ≥3 HOMA index.
| Hyperinsulinemia | Thyroid ultrasound | Total | |
|---|---|---|---|
| Homogeneous | Heterogeneous | ||
| Lower insulin 15 | 18 | 1 | 19 |
| Insulin greater tan/equal 15 | 22 | 9 | 31 |
| Total | 40 | 10 | 50 |
Table 4: Note: Fisher exact test p=0.037 (significant).
| Insulin resistance HOMA | Thyroid ultrasound | Total | |
|---|---|---|---|
| Homogeneous | Heterogeneous | ||
| Yes | 26 | 10 | 36 |
| No | 14 | 0 | 14 |
| Total | 40 | 10 | 50 |
Table 5: Note: Fisher exact test p=0.024 (significant).
When we evaluate the possible relationship between patients with thyroid nodules and those who had hyperinsulinism, we found that 80% (n 4) of patients who had thyroid nodules had as well hyperinsulinism; showing a positive relationship between the two variables (Figure 12).
As we described in the introduction the number of obese people increases with the passing of the years; this applies to both adult and pediatric population. Weight gain results in a series of metabolic processes that affects different organs and systems, as the heart, blood vessels, liver, lipid profile, pancreas, and thyroid commence; among others. Obesity brings with it a high percentage of patients with increased blood insulin levels (expressed as acanthosis nigricans on the back of the neck, armpit or groin). Hyper-insulinemia, among other things, predisposes to increased incidence of thyroid nodules in the adult population.
In this paper we wanted to assess whether there was a relationship between obesity and hyper-insulinism, with increased susceptibility to thyroid nodules in the pediatric population. The presence of thyroid nodules in children must be always studied because thyroid cancer is more frequent in this population. The frequency of this type of tumor in the pediatric population varies by age (Table 6). According to the degree of differentiation, the frequency of these can be seen in the table below (Table 7).
| Differentiated thyroid cancer in childrens | |
|---|---|
| Frequency | Age |
| 1/1.000.000 | <10 años |
| 1/200.000 | 10-14 años |
| 1/75.000 | >14 años |
Table 6: Frequency of differentiated thyroid cancer in children by age.
| Thyroid cancer in children Frequency according to their degree of differentiation |
|
|---|---|
| Degree of differentiation | % |
| Differentiated | 96 |
| Undifferentiated | 1 |
| Medullary | 3 |
Table 7: Shows the percentage frequency according to their degree of differentiation.
The first thing evaluated in this study was the number of children with obesity had heterogeneous ultra-sonographic pattern (the scans were all performed by the same operator, to avoid differences between different operators observation). This assessment found that 20% presented heterogeneous ultrasound pattern (in other words 1 in 5 obese children have ultrasound abnormalities in the thyroid gland); which it is a high percentage that leads us to think about the possibility of having to make thyroid ultrasound all children are overweight or obese.
Following this first data obtained, we tried to find the relationship between children who had heterogeneous ultrasound and the presence of serum hyper-insulinism. The analysis of both variables shown that 90% of those with heterogeneous ultrasound coursed with high blood insulin levels (9 of 10 patients) (Fisher’s exact test=p=0.037). Which is no minor detail so we suggested that all children are overweight or obese that occur with increased serum insulin levels should not stop hacérseles ultrasound thyroid, performed the same, if possible, with good ultrasound and sonographer with experience in this type of study.
Which we were also analyzed the frequency of nodules in this population and the characteristics thereof; and as shown in the results, in our patients we studied we found that 10% (n 5) 50 ultrasound screening showed nodules (one in 10 children with the characteristics studied showed nodules in the thyroid gland). The total of which 20% were pseudo nodules and the remaining 80% is divided equally between cystic and solid nodules (40% of cysts and nodules 40% solids).
This is interesting to think from prevention and early detection of the same in the child population under review, and the ability to prevent the occurrence of thyroid cancer. Finally we seek direct relationship that might exist between hyper-insulinemia and thyroid nodules found in the scans of our patients. We found that 80% of patients with thyroid nodules had elevated blood insulin levels. Hence the importance of conducting thyroid ultrasound in children also appears to present the characteristics that we have analyzed in our study.
Childhood obesity is increasing steadily with the clinical, physical and psychological consequences that this implies. We demonstrate in this study that there is a direct relationship between obesity and insulin levels. This brings a higher percentage of ultrasound abnormalities in the thyroid gland, with a consequent increase in susceptibility to the occurrence of thyroid nodules. We suggest thyroid ultrasound performed by trained professional to all children with obesity and hyper-insulinemia.