
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2021)Volume 12, Issue 7
Background and aim: During pregnancy, edema and obesity obscure the anatomical landmark and because of this epidural space identification become difficult by conventional methods. Loose connective tissue also causes false loss of resistance and responsible for failed block and complications. This study was planned for USG (ultrasonography) guided puncture point detection and epidural space depth assessment and its correlation with actual needle insertion depth in obstetric patients.
Methods: Sixty four patients of ASA I and II for elective caesarean sections were included in this study. Lumbar space was identified by USG in which ligamentum-flavum with dura mater complex was taken as key structure for assessment of Ultrasound Depth (UD). This was followed by epidural needle insertion at the same marked point and measurement of epidural space Needle Depth (ND) taken. Concordance correlation coefficient and Bland Altman test were used to compare UD and ND.
Results: Mean ND and UD were respectively 3.63 ± 043 cm and 3.61 ± 0.17 and these distances were not significantly different (P>0.0001). Bland Altman analysis showed mean of difference between UD and ND to be insignificant (0.02). Significant concordance correlation r=0.96 (95% CI-0.94-0.9, p>0.0001) was observed between ND and UD.
Conclusion: In obstetric population pre puncture ultrasound scanning of lumbar spine helps in approximate assessment of epidural space depth and its correlate precisely with actual needle depth.
Ultrasonography; Obstetric epidural; Ligamentum; Flavum-duramater complex
Epidural anaesthesia procedure becomes difficult in pregnancy because of soft tissue edema and abnormal axis of spine which obscure the anatomical landmarks [1]. Hormonally altered molecular composition of tissue causes deeper and narrowed epidural space channel, consequently palpation often lead to inappropriate selection of intervertebral space [1]. The safety zone between ligamentum flavum and inadvertent dural puncture becomes smaller. The inter-spinous ligament become softer and inhomogeneous which imitate an untimely loss of resistance and mal-placement of epidural catheter [2]. Several attempts to relate the epidural space depth with patient related parameters such as weight and height have been proved ineffective for clinical use [3,4]. Epidural space distance measurement can be obtained by lateral radiography of lumbar spine or by computerized axial tomography but both are inappropriate diagnostic tools in pregnancy because of hazardous radiation exposure to fetus. USG is a newer diagnostic tool which is free of radiation and simple to use in pregnancy.
The first study of ultrasonic measurement of the epidural space was done in 1980. They found a strong relationship between ultrasonic images of the epidural space depth and the epidural needle puncture depth [5,6]. Further studies found ultrasonography to be useful in puncture point detection for neuraxial block in obese parturients [7]. In sonographic view ligamentum-flavum was identified as key structure in determining approximate epidural space depth [8]. USG found to reduces epidural catheter insertion failure rates and placement attempts [9]. USG scanning of spine in transverse plane accurately estimates the epidural space depth and give information regarding landmark in midline in parturient patients [10-16]. Hypothesis of this study was the approximate assessment of epidural space depth and its correlation with actual needle depth in parturients undergoing caesarean section. Precision of epidural space depth by the ultrasound and assessment of its correlation with actual needle depth
This was a prospective correlational study which was conducted on sixty five parturients of ASA I and II posted for elective caesarean section. Patient with any contraindication to neuraxial block were excluded from study. The patient was made to sit with neck flexion, arms resting on the side and feet resting on a stool. After the positioning, inspection and palpation of the back was performed. Quality of anatomical landmarks were noted as ‘good’ when landmarks identified on inspection, ‘fair’ when they were identified only on palpation and ‘poor when they were difficult to identify on deep palpation. Tuffier`s line was used as a landmark for interspace marking. Portable ultrasound system equipped with a 2-5 MHz curved array probe (kontron medical, Type; SONEO EN, SN; 040165) was used for USG scanning in unsterile manner. In the midline transverse plane spinous process was identified as hyper- echoic signal continuing as long triangular hypo-echoic shadow [1,3]. Intervertebral space visualized as acoustic shadow containing articular process, transverse process, posterior complex, intrathecal space and anterior complex. Ligamentum flavum together with duramater called as posterior complex which was taken as reference key structure [3,16]. The best image was frozen and with the aid of a built-in caliper, the Ultrasound Depth [UD] i.e., the depth to reach the epidural space from the skin to the inner surface of the ligamentum flavum–duramater complex (posterior complex) was measured. For the marking of insertion point transducer was kept steady and perpendicular lines were drawn on the midpoint of all aspects of probe and the intersection of these lines were taken as insertion point [9]. Inclination angle of USG probe in relation to skin was noted visually for needle trajectory. USG image was considered ‘good’, if key structure (ligamentum flavum–duramater complex) was sharp with clear demarcation, ‘fair’ if it was not sharp but had some demarcation and ’poor’ if it was visible with blurred margin [9-11].
Epidural procedure was done by the same anaesthesiologist [resident trainee with eight month experience under guidance of radiologist and senior anaesthesiologist] in the same position under all aseptic precautions. The puncture point marked by USG was infiltrated with 2 ml of 2% lignocaine followed by 18-gauge Tuohy epidural needle [B. Braun Melsungen AG, Germany with 10 mm markings on total 80 mm length] insertion at the predetermined insertion point and angulations obtained by USG. The epidural space confirmation was done by a loss of resistance to air technique then multi-orifice closed tip epidural catheter was inserted 5 cm into the epidural space. Before withdrawing the needle, needle shaft was marked at the point of skin insertion and this distance from the tip of the needle to the marking point on the needle shaft was measured as Needle Depth (ND). A test dose of 2 ml of 2% lignocaine with adrenaline was given through the epidural catheter to rule out intravenous or intrathecal placement of the catheter after negative aspiration for cerebro-spinal fluid or blood. The number of needle reinsertion and redirection were recorded. We gave subarachnoid block for caesarean section in a different space using hyperbaric 0.5% bupivacaine with Luer lock 25 gauge quincke needle. Epidural catheter was used for intraoperative analgesia supplementation if required and for post- operative analgesia for twenty four hours.
The sample size was calculated on concordance correlation coefficient 0.88 between ultrasound depth and needle depth, with standard deviation of 0.05, 80% power and 5% alpha error. He number of minimum patient required for this study were forty eight, we evaluated sixty five patients to compensate for possible protocol violations during the study period. Descriptive statistics were calculated by using mean, standard deviation and range (maximum to minimum) for continuous data and percentages for discrete variables. The Bland Altman test was used to assess the magnitude of difference between ultrasound depth and needle insertion depth and mean of differences between two measurements. Pearson correlation coefficient was calculated along with statistical significance for determining linear relationship between ultrasound depth and needle depth. The value of P<0.05 was considered as statistically significant.
We prospectively collected the data after examining sixty five parturient patients of ASA grade I and II posted for elective caesarean section (Table 1).
| Mean | Variance | SD | Minimum | Maximum | |
|---|---|---|---|---|---|
| Age (years) | 26.2 | 19.725 | 4.4413 | 20 | 37 |
| Weight (kilogram) | 59.708 | 75.4601 | 8.6868 | 43 | 80 |
| Height (centimeter) | 152.046 | 36.7635 | 6.0633 | 136 | 170 |
| BMI (kilogram/meter2) | 26.05 | 16.3342 | 4.0416 | 19.89 | 40.54 |
Table 1: Demographic profile of elective caesarean section.
Mean of ND was found to be 3.63 cm ± 0.43 cm, minimum depth was 2.9 cm and maximum depth was 5 cm. Mean UD was 3.61 cm ± 0.17 cm, minimum UD was 2.9 cm and maximum was 4.8 cm. Pearson correlation coefficient between UD and ND was 0.96 showing strong positive linear correlation. 95% confidence interval was between 0.94 to 0.97 and its P value was 0.0001. Concordance correlation coefficient between UD & ND was found to be 0.963 (95% Confidence interval-0.94 to 0.97) with an accuracy 0.998 and precision 0.965.The slope was 0.921 and the intercept at 0.270 (Figure 1). Bland–Altman analysis in Figure 2 shows that the mean of the difference between UD and ND was statistically insignificant as most of data were under the 95% limit of agreement for the differences. The lower limit of 95% agreement was -0.21 cm and the upper limit was 0.24 cm (Figures 2-4).
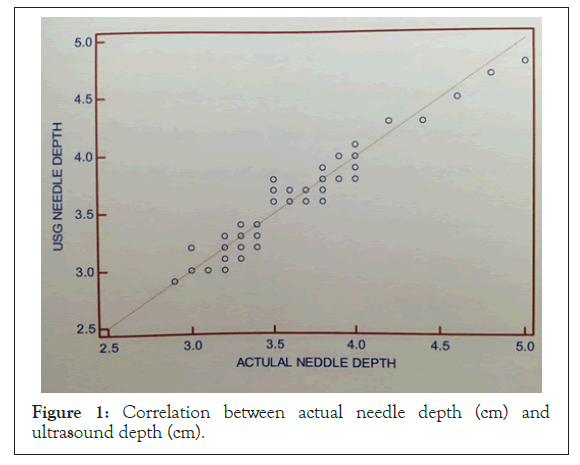
Figure 1: Correlation between actual needle depth (cm) and ultrasound depth (cm).
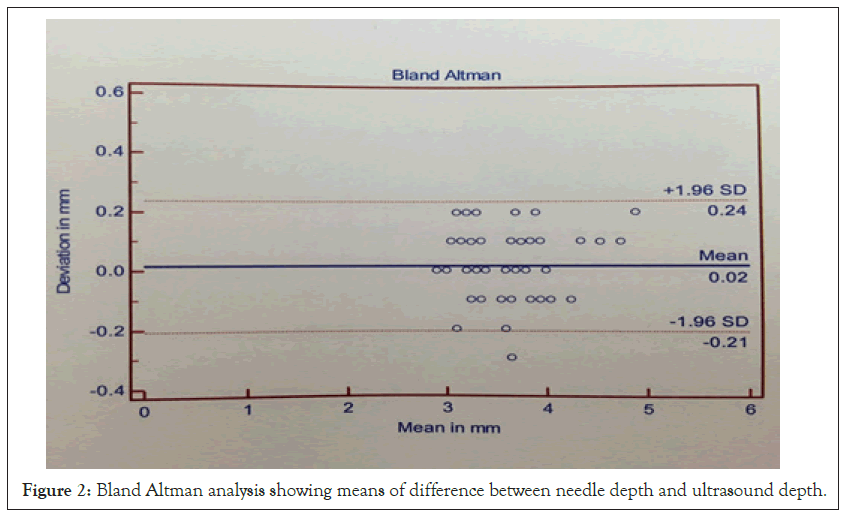
Figure 2: Bland Altman analysis showing means of difference between needle depth and ultrasound depth.
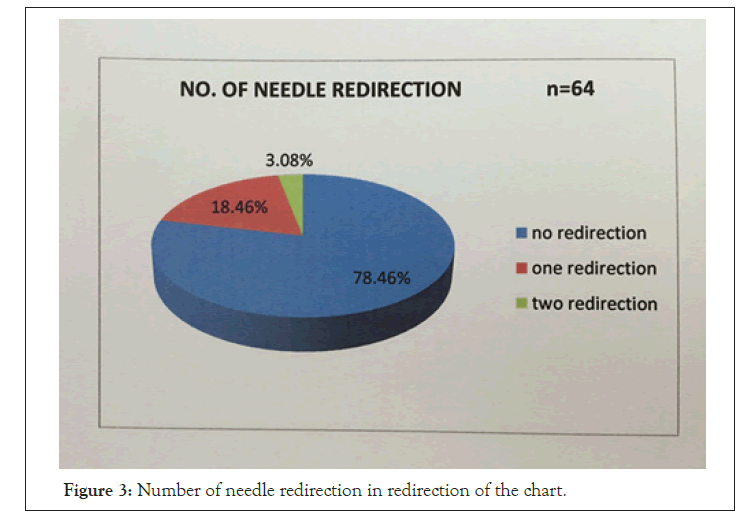
Figure 3: Number of needle redirection in redirection of the chart.
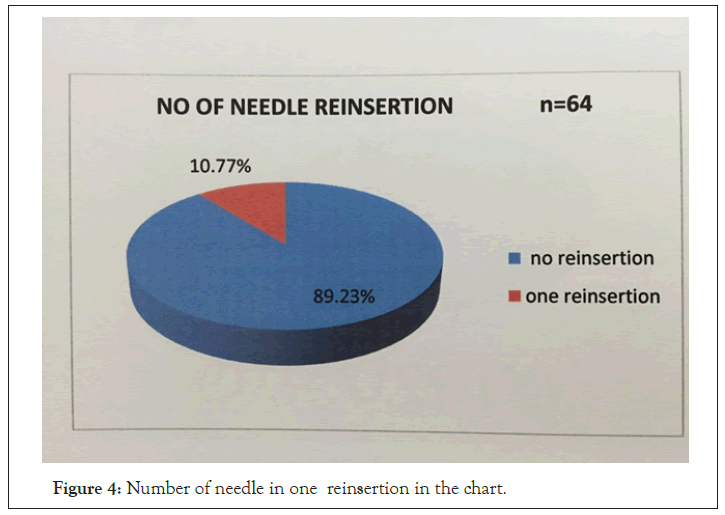
Figure 4: Number of needle in one reinsertion in the chart.
Conventional epidural needle insertion technique lacks of accuracy in pregnant patients because of physiological changes obscure the anatomical landmarks. In literature, failure rate of epidural anaesthesia in pregnancy is between 6%-25%. Now a day USG evolved as a useful tool in pregnancy for pre-puncture lumbar spine scanning as it is devoid of radiation exposure to fetus [14].
Previously the USG scanning of epidural space has been done in transverse plane, midline longitudinal or para-median plane by various authors [1-11]. We studied our population in the midline transverse plane as it is good for mid line procedure using signal from ligamentum-flavum and duramater complex as a key structure [8-12].
In our population, we found that ultrasound depth and needle depth, highly correlated with each other as shown by Concordance correlation coefficient value [r2= 0.963] and Pearson correlation coefficient (r=0.96). This finding was comparable with the previously done work [r2=0.79-0.92] [1-4]. It was stated from previously done study that UD was slightly shorter than ND that because of pressure caused by USG transducer on skin surface [9,10]. Mean of Absolute difference between UD & ND came to be 0.02 mm by Bland-Altman analysis, which was statistically insignificant, same was found in previously done studies [1-3]. In contrast Balki et al. found this difference to be statistically significant in obese parturient with value of 0.3 ± 0.5 cm but clinically insignificant [9,10]. Pre puncture determination of the insertion point and needle trajectory reduces the need of needle reposition compared with the conventional palpation method. We found puncture site in first attempt without reinsertion in 89.23% patients. Grau T also found higher success rate with the use of USG [9-15]. Maximum of two times redirection were required in two patients who were of higher BMI, similar results were also shown in other study of obese parturient population in which needle redirection was required in 33% and reinsertion was required in 24% patients with multiple attempts in epidural catheter placement [11].
In most of our studied population USG scanning quality and anatomical landmark quality were of fair quality because most of patients were of mild to moderate BMI (27-30 kg/m2 to 30- 35 kg/ m2) and his study showed significant correlation between USG scanning quality and anatomical landmark with Pearson correlation coefficient value of 0.745. Studies in the patient of higher BMI showed ultrasound depiction of key structure was markedly reduced because of attenuation of ultrasound beam by fat [11].
We did not encounter any vascular puncture, paresthesia or catheter migration during epidural catheter insertion. There were no unilateral or failed block although two cases had dural puncture but none of them developed post dural puncture headache in follow up. All the epidural catheters were followed up for post-operative analgesia for twenty four hours and they found to be functioned well with good patient satisfaction as found in previously done sono guided studies also [3-11]. This study concludes that USG is a non-invasive and safe tool without radiation for pre puncture lumbar spine scanning in obstetric population. It helps in puncture point detection and approximate epidural space depth assessment. Ultrasound should be used in all obstetric patients before elective caesarean section or labor epidural for successful epidural catheter insertion, better patient satisfaction and lesser complication. However this does not preclude the need for the loss of resistance technique but provide a guide to approximate detection of needle depth of the epidural spaces.
Angle of needle insertion to skin was not precisely measured which might be contributed to differences in both UD and ND and change in needle trajectory and also a source of bias in this study. Real time ultrasonography imaging is needed for accurate prediction of needle insertion, needle trajectory and to avoid differences in UD and ND. In future, we will need real time imaging for accurate projection of ultrasound depth and to decrease the difference between ultrasound depth and needle depth.
Pre-puncture ultrasound scanning of lumbar spine in obstetric population helps in approximate assessment of epidural space depth and it’s precisely correlate with needle depth.
There was no conflict of interests in this study.
Citation: Kanwat J (2021) To Study the Correlation between Estimated Ultrasound Depth and Actual Needle Depth of Epidural Space in Transverse Plane in Parturients Undergoing Cesarean Section. J Anesth Clin Res. 12:1009.
Received: 24-Jun-2021 Accepted: 09-Jul-2021 Published: 16-Jul-2021 , DOI: 10.35248/2155-6148.21.12.1009
Copyright: © 2021 Kanwat J. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.