Journal of Osteoporosis and Physical Activity
Open Access
ISSN: 2329-9509
ISSN: 2329-9509
Case Report - (2021)Volume 9, Issue 8
Transient migratory osteoporosis is a metabolic condition which among pediatric population it’s limited only to case reports. Acute onset arthralgia in large weight-bearing joints is the main presentation. Due to its low prevalence and self-limited course there is no certain treatment for this disease. Here in this paper we are going to report a case of TMO in pediatric population whit a rapid and dramatic response to treatment with Bisphosphonates.
Osteoporosis; Transient osteoporosis; Migratory pain
Transient Migratory Osteoporosis (TMO), also known as regional migratory osteoporosis, is a less prevalent condition considered as a part of bone marrow edema syndrome [1]. This condition is usually self-limiting and, in most cases, involves lower limb joints, especially hips and knees [2,3]. It typically affects males in their middle age. The etiology of this medical condition is not clear as it is not associated with any other diseases [4,5]. Diagnosis is made by exclusion of other disease and history of migratory arthralgia especially in weight bearing joints in addition to epiphyseal local osteoporosis that often is appreciated more in MRI rather than x-ray [6].
The incidence of TMO in the pediatric and adolescent population is very low and our knowledge is limited to case reports [7,8]. This paper is a report of TMO in a young girl presented with chronic knee pain and history of migratory pain in other joints as well which was eliminated spontaneously after a period of analgesic use [9].
A healthy twelve-year-old girl complaining of five-month leftknee pain without history of trauma was presented to our tertiary pediatric center. The onset of the pain was acute, aggravated with weight-bearing and alleviated by taking a rest and using analgesics. Assessment of the patient's medical history indicated a history of self-limiting hip joint pain in the past 5 years followed by right knee pain 1 year later. The pain had similar features, and in episodes of the pain, the pain was so severe that analgesics were needed every day [10].
All previous medical examinations and treatment of the patient were performed in the primary healthcare centers. The patient with a diagnosis of migratory reactive arthritis was treated with Non-steroidal anti-inflammatory drugs (NSAIDs). Despite the given recommendations, the patient refused to be visited by a rheumatologist or an orthopedist for further evaluation. Current imaging results and physical examinations are normal and unremarkable, and the patient had no complaints about the joints involved in previous episodes [11].
The history was unremarkable unless in case of weight loss during the last five years. There is no family history of rheumatologic, metabolic, or endocrine diseases. Furthermore, physical examination revealed localized bone tenderness in the proximal portion of the right leg. There are no restrictions on knee and hip joint movement and the gait was normal. Swelling, erythema, or warmth was not detected in the joints [12].
A plain radiography of the knee and leg revealed mild osteopenia in the tibial epiphysis without any fracture or joint destruction. We ran a triphasic whole-body bone scan and increased uptake in left proximal tibial metaphysis was detected. Non-contrast MRI study with T1 and T2 weighted imaging revealed bone marrow edema in epiphysis which extends toward the metaphysis of proximal tibia without any bone or soft tissue destruction (Figure 1).
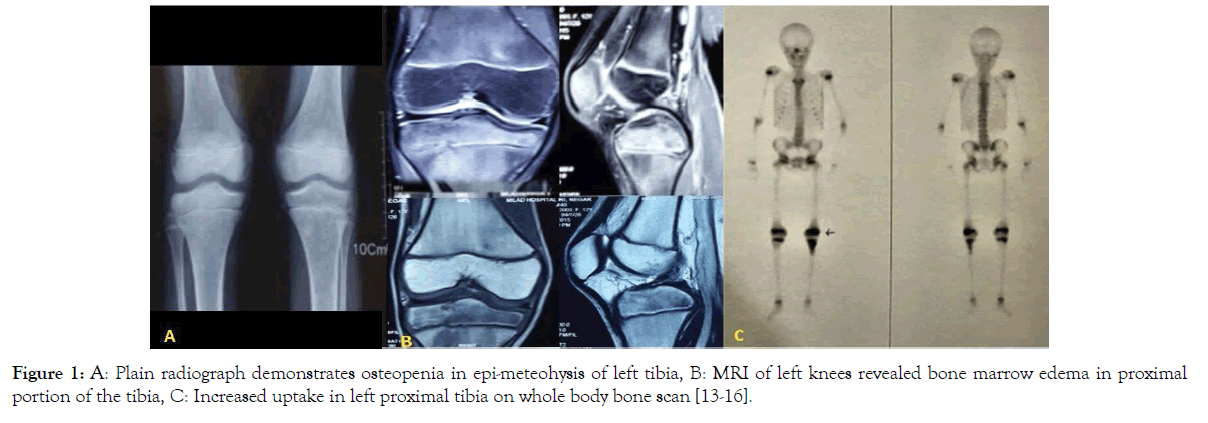
Figure 1. A: Plain radiograph demonstrates osteopenia in epi-meteohysis of left tibia, B: MRI of left knees revealed bone marrow edema in proximal portion of the tibia, C: Increased uptake in left proximal tibia on whole body bone scan [13-16].
Bone Mineral Densitometry (BMD) surprisingly revealed severs osteoporosis (z-score -3). Full blood count, endocrine studies including thyroid function test and PTH level, urine analysis, and inflammatory as well as rheumatologic markers were unremarkable, whereas, calcium, phosphorus, vitamin D, and magnesium were within the normal range (Table 1).
| Laboratory data | Result | Normal value | Laboratory data | Result | Normal value |
|---|---|---|---|---|---|
| Calcium | 9.3 mg /dl | 8.6-10.3 | Na | 138 meq/L | 135-145 |
| Phosphorus | 4.9 mg /dl | 3-5.7 | K | 3.7 meq/L | 3.5-5.2 |
| Albumin | 4.6 gr/dl | 3.5-5.2 | WBC | 5200 | 4000-10000 |
| Magnesium | 22 mg /dl | 1.5-2.6 | Platelet | 214000 | 150000-400000 |
| 25(OH) Vitamin D3 | 32 ng/ml | >30 | Haemoglobin | 12.8 | 12-14 |
| Alkaline phosphatase | 403 U/L | 180-1200 | ESR | 14 mm/h | 0-10 |
| PTH | 20 pg/ml | 9-94 | CRP | 0.7 mg/L | <6 |
| TSH (ECL) | 1.9 miu/ml | 0.4-4 | AST | 14 U/L | <31 |
| T4 (ECL) | 26 ug/dl | 10-60 | ALT | 17 U/L | <31 |
| 24 h Urine Potassium | 30 meq/24h | 25-125 | Serum Ion | 99 micg/dl | 60-170 |
| 24 h Urine Creatinine | 317 mg/24h | 600-1800 | TIBC | 325 micg/dl | 250-450 |
| 24 h Urine Calcium | 48 mg/24h | 100-300 | Cr | 0.7 mg/dl | 0.4-1.2 |
| 24 h Urine volume | 1000 ml | BUN | 13 mg/dl | 10-30 |
Table 1: Laboratory data.
According to the history of migratory arthralgia in multiple joints, physical examination, and more importantly imaging, and laboratory findings, and by excluding other conditions, the diagnosis of TMO could be considered [13-15]. A multidisciplinary team of specialists including orthopedic surgeon, rheumatologist, endocrinologist, radiologist, and neurologist were involved in the diagnosis process. Finally, by exclusion other diagnosis, TMO was considering more probable. Accordingly, Pamidronate was administered intravenously for the patient for three days with a dose of 1.5 mg/kg/day (in this patient, 30 mg/day), and immediately after the first dose of IV Pamidronate, pain was controlled and significantly diminished. The treatment continued by weekly oral bisphosphates (30 mg/week) for six months. At 20 months, the follow-up examination of the patient demonstrated that she was pain-free and gained weight about 10kg. In the follow-up bone mineral densitometry, Z-Score was increased significantly which was in the normal range and was indicative of the positive response to treatment. The plain radiographic study demonstrated that osteopenia has completely disappeared and follow-up MRI revealed normal appearance without any bone marrow edema (Figure 2).
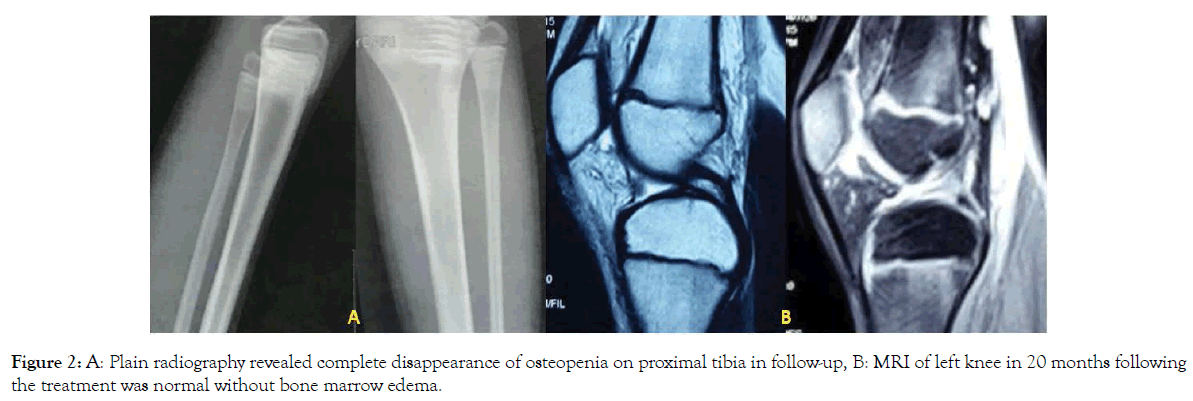
Figure 2. A: Plain radiography revealed complete disappearance of osteopenia on proximal tibia in follow-up, B: MRI of left knee in 20 months following the treatment was normal without bone marrow edema.
TMO is a rare self-limiting condition with unknown pathogenesis which usually involves the weight-bearing joints in a migratory patter. Although TMO in adults has been frequently reported in literature, based on our knowledge, in pediatric population, it is limited to 2 case reports of 2 patients at age of 12 and 15.
Diagnosis is based on a specific history of self-limiting migratory arthralgia, imaging findings including local osteoporosis and bone marrow edema, and excluding other possible conditions. In fact, no known diagnostic criteria for this rare disease have been introduced. Differential diagnosis for this disease such as septic or reactive arthritis, osteomyelitis, fractures, tumors and infiltrative conditions, metabolic and structural disorders like osteogenesis imperfecta should be excluded before making the diagnosis of TMO (Table 2).
| Category | Subgroup | Features |
|---|---|---|
| Traumatic | Occult fracture | History of trauma |
| Cortical disruption | ||
| Presence of hematoma and soft tissue injury | ||
| Bone bruise | History of trauma | |
| Osteochondral injury | History of trauma and locking events | |
| Presence of loose body in joint | ||
| Disruption of cartilage surface | ||
| Osteogenesis Imperfecta | History of multiple fractures with minimal trauma | |
| Blue sclera | ||
| Radiographic evidence of old and healed fracture with bony deformities | ||
| Infectious/Reactive | Osteomyelitis | Fever and chill with presence of swelling, effusion, erythema, and warmth in the joint |
| Septic arthritis | Elevated inflammatory markers (WBC count, ESR, CRP) | |
| Reactive arthritis | Restricted ROM | |
| CRMO | Positive culture in blood or synovial fluid | |
| Inflammatory | Enthesitis | Multiple synchronous joint involvement |
| Rheumatologic arthropathies (AS, RA, Psoriasis) | Morning stiffness | |
| Arthritis (swelling and effusion) | ||
| Elevated inflammatory or rheumatologic factors | ||
| Multisystem manifestations | ||
| Infiltrative | Leukaemia | Weakness, weight loss, fever |
| Elevated WBC count | ||
| Positive bone marrow examination | ||
| Ischemic | Avascular necrosis | Corticosteroid use |
| Destruction of cartilage | ||
| Subchondral fracture and collapse | ||
| CRPS | History of trauma and immobilization | |
| Shiny skin | ||
| Diffuse osteopenia | ||
| subperiosteal bone resorption | ||
| preservation of joint spaces | ||
| Sickle cell anemia | Anemia | |
| History of sickling episodes | ||
| Radiographic features like AVN |
Table 2: Summarized differential diagnose and their features.
In almost all reports of TMO in adult population, the disease is usually described with acute or subacute onset arthralgia in a self-limited course. In pediatric population reports are limited to three cases in two articles. Joshi et.al reported regional migratory osteoporosis in a 15 years old child with Gaucher disease. The child was totally asymptomatic and bone marrow edema was detected on routine evaluation of the long bones with MRI. Bone marrow edema was limited to the proximal tibial epiphysis. Santori et al. reported cases of TMO in 12 years old child in 1985 and to date to our knowledge it is the youngest case of TMO [8]. They reported a 13 years old boy with asymptomatic bone marrow edema in the spine and a 12 years old girl with pain and bone edema in the proximal tibia. Both had familial history of transient bone marrow edema and in both cases edema and pain disappeared spontaneously after several months. Current study reports an unusual case of a patient with migratory arthralgia for about 4 to 5 years without any improvement.
In the early stages, imaging studies may be normal. MRI is considered as the modality of choice in diagnosis of TMO. The findings include increased signal on T2 weighted images and lowsignal intensity on T1 images, which are characteristics of edema. As the radiographic imaging can be normal in the first weeks, bone scan seems to be more sensitive in the early stages of disease.
As the disease has a natural self-limited history, management is based on conservative treatment and follow-up examination. The effectiveness of bisphosphonates in treating painful benign bony pathologies is established, so they are considered effective and safe in treating TMO. Our case showed immediate and significant response just after receiving the first dose of IV Pamidronate as reported in other case reports. Ringe et al. used IV Ibandronate in 12 cases of painful transient local osteoporosis and after 1 to 3 months most of them were pain free. In addition to increase in bone density [16]. They reported that in patients with refractory pain to analgesics, Ibandronate let to complete pain relief. Additionally, the persistence of treatment with oral bisphosphonate resulted in normal bone densitometry in the long-term follow-up. Also, it is unclear if Pamidronate is effective in the course of disease or not and what is the best time for starting it. One of the limitations of this report is that relationship between TMO and weight loss is not clear and it’s not mentioned in other reports. As the prevalence is very low in the pediatric population, further research seems to be needed on etiology and course of the disease, as treatment policy.
Citation: Nabian MH, Zargarbashi RH, Rabie H (2020) Transient Migratory Osteoporosis: A Case Report in Pediatric Population. J Osteopor Phys Act. 9:265.
Received: 17-Jul-2021 Accepted: 10-Aug-2021 Published: 17-Aug-2021 , DOI: 10.35248/2329-9509.21.9.265
Copyright: © 2021 Nabian MH, et al. This is an open access article distributed under the term of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.