Journal of Sleep Disorders & Therapy
Open Access
ISSN: 2167-0277
ISSN: 2167-0277
Case Report - (2020)Volume 9, Issue 4
Central sleep apnea (CSA) is a neurological breathing disorder resulting from intermittent disruptions in the neural drive to breath. CSA and obstructive sleep apnea (OSA), caused by partial or complete airway blockage, sometimes occur together. The remede System (Respicardia, Minnetonka, MN) is an implantable device that delivers transvenous phrenic nerve stimulation therapy (TPNS) to treat CSA. A patient who failed previous Positive Airway Pressure (PAP) therapies presented with severe CSA and OSA with a baseline Apnea Hypopnea Index (AHI) of 98.1 events/hour. The patient was implanted with a TPNS device and titrated to maximum effectiveness. His CSA improved, but still had persistent OSA. PAP therapy was added to supplement the TPNS. With TPNS off, PAP therapy treated obstructive events but not the central events. TPNS alone treated the central events but not the obstructive events. With both therapies on, CSA and OSA were controlled and breathing was normalized (AHI=3.8). ClinicalTrials.gov Identifier: NCT01816776.
Transvenous phrenic nerve stimulation; Central sleep apnea; Positive airway pressure; Obstructive sleep apnea
AHI: Apnea Hypopnea Index; APAP: Automatic Positive Airway Pressure; ASV: Adaptive Servo Ventilation; CAI: Central Apnea Index; CHF: Chronic Heart Failure; CPAP: Continuous Positive Airway Pressure; CSA: Central Sleep Apnea; EPAP: Expiratory Positive Airway Pressure; HFrEF: Heart Failure with reduced Ejection Fraction; HI: Hypopnea Index; Kg: Kilograms; LVEF: Left Ventricular Ejection Fraction; M: Meters; MAI: Mixed Apnea Index; OAI: Obstructive Apnea Index; PAP: Positive Airway Pressure; PAV: Positive Airway Ventilation; PSG: Polysomnogram; QOL: Quality of Life; T90: Time with oxygen saturation less than 90%; TPNS: Transvenous Phrenic Nerve Stimulation
Central sleep apnea (CSA), a rare condition in the overall population, is a neurological breathing disorder resulting from intermittent disruptions in the neural drive to breathe [1-3]. Analysis of data from the Sleep Heart Health study shows in patients with heart failure (HF), though OSA is common, up to 4% of patients have co-existent CSA [4]. Moreover, CSA is predominantly seen in patients with systolic HF and to a lesser degree with high altitude and opioid drug use [1,5,6]. CSA and obstructive sleep apnea (OSA), caused by partial or complete blockage of the airway, can occur together to varying degrees [7]. How to most effectively treat patients with both forms of sleepdisordered breathing remains uncertain. Concomitant therapy including implantable devices along with Positive Airway Pressure (PAP) therapy may be beneficial in selected patients. The remede System (Respicardia, Minnetonka, MN) is an implantable device that delivers transvenous phrenic nerve stimulation (TPNS) therapy to treat moderate to severe CSA in adult patients (Figure 1). This is the first reported case demonstrating the combination of TPNS and Automatic Positive Airway Pressure (APAP) to treat both CSA and OSA.
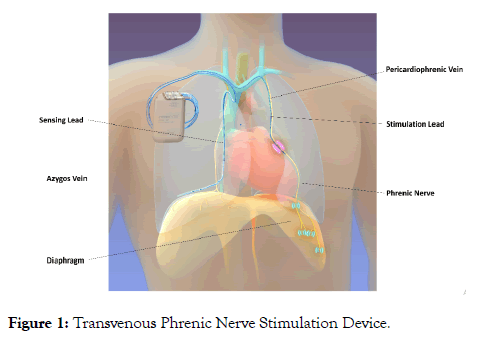
Figure 1: Transvenous Phrenic Nerve Stimulation Device.
A 59-year-old man with chronic systolic heart failure (CHF), NYHA class II, ischemic cardiomyopathy, left ventricular ejection fraction (LVEF) 43%, prior stroke, weight 105.7 kg, and body mass index (BMI) 35 kg/m2, presented with classic sleep apnea symptoms despite optimized and stable guideline-directed medical therapy for HF. A baseline sleep study revealed an apnea hypopnea index (AHI) of 98.1 events/hour, composed predominantly of central apnea events (61/hour), obstructive apnea events (13/hour) and hypopnea events (18/hour, 12 of which were considered obstructive in nature) (Table 1). The patient failed adaptive servo-ventilation (ASV) which was standard of care at the time for complex CSA and the residual AHI was 22 events/hour which could not be differentiated between central or obstructive. The ASV settings were the following: EPAP (Expiratory positive airway pressure) min=8, EPAP max=15, PS (pressure support) min=0, PS max=29 with auto backup rate. The patient was 100% compliant with ASV. However, the patient reported persistent sleepiness as evidenced by an ESS of 12 despite optimal treatment with ASV.
Table 1: Sleep Metrics (events/hour).
| Visit | TPNS/APAP Therapy Use | AHI | CAI | OAI | MAI | HI (Obstructive HI) |
|---|---|---|---|---|---|---|
| Baseline | None | 98 | 61 | 13 | 5 | 18 (12) |
| 6 Months | TPNS only | 74 | 1 | 28 | <1 | 44 (44) |
| 12 Months | TPNS only | 79 | 3 | 17 | <1 | 60 (59) |
| 18 Months | TPNS and APAP | 10 | 0 | 4 | 0 | 6 (6) |
| 24 Months | TPNS only | 47 | <1 | <1 | 0 | 46 (45) |
| 36 Months | TPNS and APAP | 0 | 0 | 0 | 0 | 0 (0) |
Note: Sleep metrics over time showing TPNS therapy alone treated central but not obstructive events whereas combination TPNS and APAP therapy successfully controlled both central and obstructive events. Obstructive HI is presented as a component of the displayed HI.
Abbreviations: TPNS: Transvenous Phrenic Nerve Stimulation; APAP: Automatic Positive Airway Pressure; AHI: Apnea Hypopnea Index; CAI: Central Apnea Index; OAI: Obstructive Apnea Index; MAI: Mixed Apnea Index; HI: Hypopnea Index
He underwent a transvenous phrenic nerve stimulator implant as an enrolled subject in the remede System pivotal trial and consented to publication of data [8]. The TPNS device was titrated to maximum effectiveness. Follow-up polysomnograms (PSG) were performed every 6 months.
The PSGs at 6 and 12 months showed that with TPNS therapy, the patient was experiencing ≤ 4 central apnea and hypopnea events per hour, but >70 obstructive apnea and hypopnea events per hour (Table 1). Despite the residual AHI, the Epworth Sleepiness Scale improved from 14 at baseline to 4 at 6 months and 6 at 12 months. The percent of sleep with oxygen saturation <90% (T90) decreased from a baseline of 86% to 66% at 6 months and 61% at 12 months, while the average oxygen saturation increased from 83% at baseline to 88% and 89% at 6 and 12 months, respectively. NYHA class improved to I at 6 months and the six-minute walk distance increased from 335 m at baseline to >420m at these visits. LVEF was 41% at 12 months. The patient reported feeling markedly improved on the Patient Global Assessment at 12 months and did not have any complaints about discomfort from stimulation or the implant procedure, so he wanted to continue TPNS therapy.
After the 12-month follow-up visit, APAP was added as a supplement to TPNS to treat the residual obstructive events. The APAP pressures were titrated during a routine PSG. Effectiveness of the two individual therapies was assessed using auto positive airway pressure therapy alone, transvenous phrenic nerve stimulation therapy alone, and with both therapies combined during the APAP titration PSG. It was observed that APAP therapy alone treated obstructive apnea and hypopnea events but not central events (Figure 2A). TPNS therapy alone treated central apnea and hypopnea events but not obstructive apnea and hypopnea events (Figure 2B). Combined TPNS and APAP therapy normalized breathing by controlling both CSA and OSA, resulting in an AHI of 3.8 events/hour during that portion of the night (Figure 2C). The final APAP pressures of 6 cm H2O-12 cm H2O were well tolerated. The patient preferred automatic positive airway pressure mode over Continuous Positive Airway Pressure (CPAP) and remained comfortable on that mode. The patient proceeded to use the combination therapy daily.
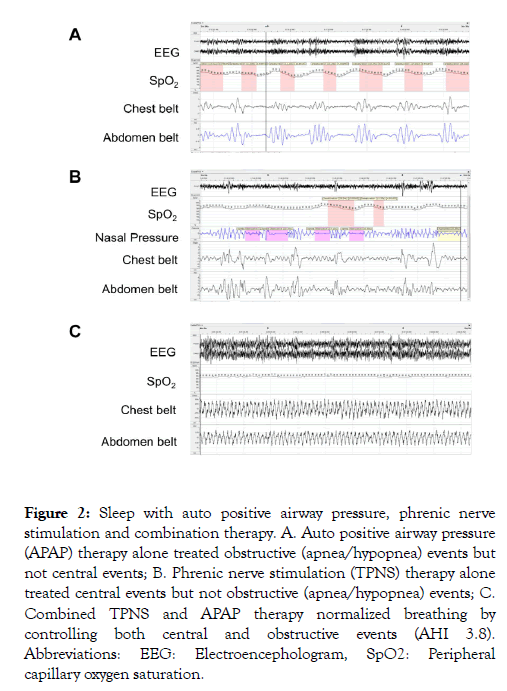
Figure 2: Sleep with auto positive airway pressure, phrenic nerve stimulation and combination therapy. A. Auto positive airway pressure (APAP) therapy alone treated obstructive (apnea/hypopnea) events but not central events; B. Phrenic nerve stimulation (TPNS) therapy alone treated central events but not obstructive (apnea/hypopnea) events; C. Combined TPNS and APAP therapy normalized breathing by controlling both central and obstructive events (AHI 3.8). Abbreviations: EEG: Electroencephologram, SpO2: Peripheral capillary oxygen saturation.
At the 18-month follow-up visit, TPNS and APAP combination therapy reduced the baseline AHI by 90% to 10 events/hour, including a reduction in all AHI components (Table 1). Oxygenation further improved (T90 was down to 2% and average oxygen saturation was up to 93%). The 24-month visit PSG was performed with TPNS therapy only; APAP was turned off in order to assess the single therapy result. Again, the presence of residual OSA was observed. Successful treatment of CSA was maintained with 0 central apnea events/hour. T90 was similar to the results at 6 and 12 months with TPNS only (62%) and average oxygenation went back down to 89%. The OSA was quite a bit lower at the 24-month PSG compared to prior PSGs with only TPNS, which could in part be explained by further weight loss (10.2 kg reduction since baseline). LVEF remained relatively stable at 38% and the patient was determined to be NYHA Class II at the visit. A home sleep apnea test was performed at 36 months using both therapies combined. Breathing was normalized with an AHI of 0 events/hour, T90 of 0% and average oxygenation 93% and NYHA remained Class II. The patient did not report discomfort or other related adverse events from the therapy throughout the trial and remains treated with both therapies and is sleeping well.
Both CSA and OSA can co-exist especially in patients with HF. It’s important to recognize that sleep-disordered breathing is a significant comorbidity and needs to be effectively treated in this patient population as repeated episodes of apnea, hypoxia, reoxygenation and arousals lead to sympathetic nervous system activation, oxidative stress and systemic inflammation which can worsen CHF [2]. Addressing HF symptoms with guidelinedirected medical therapy should be the first treatment step to manage the heart failure and assess it if resolves the sleep disordered breathing. If the sleep disordered breathing persists, treatment specific to the sleep disorder is the next step. Though CPAP is clearly the established standard treatment for OSA, treatment options for CSA are evolving. Adaptive Servo Ventilation (ASV) used to be a standard treatment for this group of patients as it has expiratory positive airway pressure (EPAP) to treat OSA and with the help of pressure support along with a back-up rate it can also successfully treat CSA. But evidence from the SERVE-HF trial demonstrated increased mortality in patients with HF with reduced ejection fraction (HFrEF) when ASV was used to treat central sleep apnea [9]. More recently, transvenous phrenic nerve stimulation was approved by FDA for the treatment of moderate to severe CSA in adult patients and was shown to significantly reduce the AHI, CAI, and arousals and improve quality of life (QOL) [10].
In the patient described in this case, TPNS effectively treated CSA but did not treat OSA. Auto positive airway pressure therapy alone treated OSA but did not treat CSA. Interestingly, in this patient the obstructive events increased at the 6- and 12- month PSGs compared to the patient's baseline PSG. It is possible the increase in obstructive events was due to events scored as central at baseline being both central and obstructive in nature (no effort and airway closed) appearing as obstructive (airway remains closed) when treating the central aspect of the event. Weight gain did not explain the increase in obstructive events as the patient’s BMI decreased from 35 kg/m2 to 33.5 at 12 months (weight decreased from 105.7 kg to 100.3 kg). Moreover, the residual AHI remained high at these timepoints, but the patient reported improvement in the ESS which could be due to the decrease in AHI from baseline, the elimination of the central events and shift toward obstructive events, with the majority being hypopneas instead of apneas, or improvement in oxygenation. Also, the increase in average oxygen saturation, the decrease in T90, the improvement in six-minute walk distance and improved NYHA classification likely reflect less sleepiness. However, we cannot exclude the possibility some of the ESS improvement was due to the placebo effect since the patient was randomized to the active therapy arm in the unblinded trial. Ultimately, the combination of phrenic nerve stimulation and auto positive airway pressure safely and successfully treated both CSA and OSA.
Sleep disordered breathing is common in patients with HF. Both OSA and CSA can present together, and treatment could be challenging. New treatment modalities, especially transvenous phrenic nerve stimulation with the remede System, is available now to treat CSA. Our case illustrates a possible role for combined PAP therapy and TPNS for this patient population to treat OSA and CSA, respectively.
JF, KJ, SM are employees of Respicardia Inc., the manufacturer of the TPNS device. The other authors have no conflicts of interest to report.
Citation: Beyerbach D, Fricke J, James K, McKane S, Kanagarajan K (2020) Transvenous Phrenic Nerve Stimulation and Automatic Positive Airway Pressure Therapy for Treating Central Sleep Apnea and Residual Obstructive Sleep Apnea. J Sleep Disord Ther 9:311. doi: 10.35248/2167-0277.20.9.311
Received: 20-May-2020 Accepted: 03-Jul-2020 Published: 10-Jul-2020 , DOI: 10.35248/2167-0277.20.9.311
Copyright: © 2020 Beyerbach D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.