Journal of Clinical & Experimental Dermatology Research
Open Access
ISSN: 2155-9554
ISSN: 2155-9554
Case Report - (2022)Volume 13, Issue 5
Carbuncle is an infection of the hair follicle(s) that extends into the surrounding skin and deep underlying subcutaneous tissue. We reported a case of giant carbuncle in the nape complicated by Diabetic Ketoacidosis (DKA) and sepsis. A 72-year-old male patient, who had a history of diabetes for more than 30 years and suffered from systemic sepsis due to a giant carbuncle in the nape for 2 weeks and complicated DKA, was admitted to our hospital on December 9th, 2020. The patient significantly improved after active management with blood sugar control, antishock therapy, systemic anti-infection, local excision of infected foci, and autologous meshed split-thickness skin grafts to repair the wound. The patient recovered and discharged after 40 days. For carbuncles, we believe that the most important therapy is to drain pus sufficiently or excise lesions, which is the first step in saving a patient’s life before systematic treatment.
Carbuncle; Diabetic ketoacidosis; Infection; Skin grafts
A carbuncle is a skin infection that often involves a group of hair follicles, it typically presents as an erythematous, tender, inflamed, fluctuant nodule with multiple draining sinus tracts or pustules on the surface. Depending on the depth of invasion, necrotizing soft tissue infections can cause extensive local tissue destruction, tissue necrosis, systemic toxicity, and even death [1,2].When middle-aged and elderly diabetic patients have a poor control of blood glucose for a long time, they are often prone to complicate with dorsal carbuncle or nape carbuncle [2,3]. If the infected lesion is not treated in-time, sepsis and septic shock may be caused. Serious infections can lead to diabetes complications, causing a vicious circle and threatening the lives of patients [4,5]. Wound repair after removal of a giant carbuncle is also a question worth exploring [6,7]. Here, we reported a case of giant carbuncle in the nape complicated by Diabetic Ketoacidosis (DKA) and sepsis, and conducted a literature review of treatments for carbuncles (Table 1).
| Authors | Age/Sex | Site | Symptoms | Treatments | Outcomes |
|---|---|---|---|---|---|
| Venkatesan et al. [1] | 65/M | Back | Fever Painful Swelling |
Surgical debridement Strict diabetes control Amoxicillin and clavulanic acid |
Good |
| Iyer et al. [6] | 35-75/22M,8F | Back/10 Scapula/6 Gluteal region/6 Thigh/4 Nape of neck/4 |
Carbuncles | Excision of carbuncle with primary split-thickness skin grafting | 66·66% patients achieved wound closure |
| Akram et al. [7] | 67/M | Postier trunk | Painful Swollen Mass with purulent discharging |
Local topical antibiotic ointment Wide local excision of the carbuncle Application of the VAC Split thickness skin graft |
Wound healed |
| Hirabayashi et al. [8] | 66/M | Neck Lower extremities Gluteal region |
Painful Swelling Fever |
Surgical drainage Ampicillin–sulbactam |
Good |
| Ahmad et al. [9] | 63/M | Right temporofacial region | Swelling | Daily dressings Good sugar control |
Long time Scar |
| Gheisari et al. [13] |
51/M | Nape of the neck | Severe neck pain Massive swelling Huge carbuncle Necrotizing fasciitis |
Wide incision Several sessions of debridement Piperacillin/tazobactam and vancomycin |
A shallow ulcer without any complication |
| Wang et al. [14] | 1-81/33M,28F | Neck | Abscess Necrotizing fasciitis |
Surgical incision and drainage Ultrasound-guided fine needle aspiration and catheter drainage |
Effective |
| Chou et al. [15] | 74/F | Forehead | Painful Erythematous nodule Headache Widespread subgaleal abscess |
Incision Drainage Operative debridement Antibiotics |
Headache resolved |
| Hee et al. [18] | 71/M 46/F 47/F |
Back Left scapula Back |
painful carbuncle | Saucerization of the carbuncle was performed dressed daily or every 2 to 3-days |
No readmissions |
| Zhang et al. [19] | 50/M | Back | Fever A painful carbuncle Swelling |
Incision Drainage 5-aminolevulinic acid (ALA) photodynamic therapy |
Healed without scaring, pigmentation, and recurrence |
| Sedik et al. [20] | 56/M | Nape of the neck | Painful Swelling Fever Headache |
Excision of the necrotic skin Aggressive debridement IV amoxicillin and clavulanic acid VAC system was applied Regular daily dressing was done |
Almost healed wound |
| Ng et al. [21] | 52/M 64/F 46/M |
Facial | Painful Swelling Pus discharge |
Intravenous antibiotics Glycemic control Incision Irrigated with gentamycin solution |
Wound healed with minimal scarring |
| Ngui et al. [22] | 52/M 33/M 26/M |
Chin Face Lips |
Extensive carbuncles | Intravenous antibiotics Drainage Minimal incision Conservative wound debridement |
Superior cosmetic outcomes |
Table 1: Summary of included studies.
A 72-year-old male patient was admitted to our hospital on December 9th, 2020, due to swelling and pain in the nape with pus for 2 weeks, as well as unconsciousness for one day. The lesion had been gradually expanded. The patient has a history of diabetes for over 30 years, as well as a history of hypertension and atrial fibrillation. Vital signs on admission were as follows: Body temperature, 38.4°C; Heart Rate (HR), 160 beats/min; respiratory rate, 20 cycles/min; and Blood Pressure (BP), 101/65 mmHg (1 mmHg=0.133 kPa). Physical examination revealed that the patient was in a semi-conscious, confused state and his answers were not relevant to the questions asked. Extensive redness and swelling of the skin could be observed on the nape reaching the occiput and lower back, and extending to both sides of the neck. There were multiple spots on the surface of the skin and yellow pus secretions flowing out (Figure 1A). An emergency blood test revealed the following results: White Blood Cell (WBC) count, 24.33 × 109/L; proportion of neutrophils, 92.3%; C-Reactive Protein (CRP), 171.52 mg/L; Plateletcrit (PCT), 1.27 ng/ml; Platelet (PLT) count, 278 × 109/L; Prothrombin Time (PT), 16.1 s; Activated Partial Thromboplastin Time (APTT), 38.3 s; Red Blood Cell (RBC) count, 4.14×1012/L; Hemoglobin (Hgb), 128 g/L; Glucose (GLU), 43.5 mmol/L; Albumin (ALB), 31 g/L; Serum Creatinine (SCr), 157 umol/L; Uric Acid (UA), 882 umol/L; B-type Natriuretic Peptide (BNP), 110.76 pg/mL; urine GLU, 56 mmol/L; and urine Ketone (KET), 1.5 mmol/L. Final diagnosis indicated the following results: (1) A giant carbuncle, (2) Sepsis,(3) Acute renal insufficiency, (4) Type 2 diabetes (DKA), (5) Hypertension and (6) Arrhythmia (atrial fibrillation).
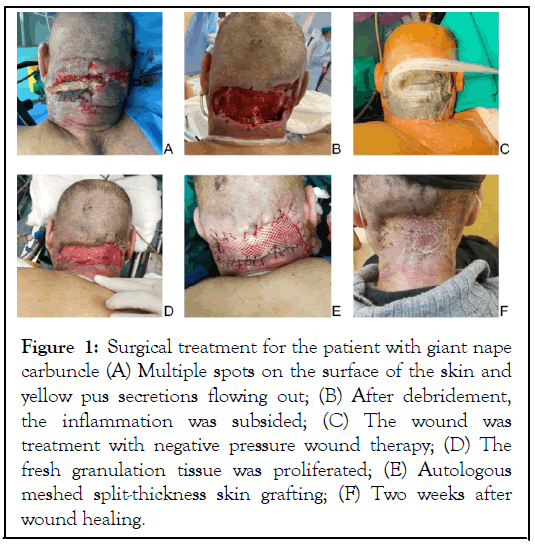
Figure 1: Surgical treatment for the patient with giant nape carbuncle (A) Multiple spots on the surface of the skin and yellow pus secretions flowing out; (B) After debridement, the inflammation was subsided; (C) The wound was treatment with negative pressure wound therapy; (D) The fresh granulation tissue was proliferated; (E) Autologous meshed split-thickness skin grafting; (F) Two weeks after wound healing.
The patient was obese with a short neck; he was in a state of lethargy and unconsciousness when he was admitted to our hospital. We took a series of rescue measures to save his life including: (1) Tracheal intubation and Noninvasive Mechanical Ventilation (NIV). Considering his weak ability to drain sputum spontaneously and the possibility of long-term bedridden pneumonia, percutaneous bedside tracheostomy was performed on December 18th, 2020, and we continued NIV. Furthermore, we delivered prone ventilation with the patient lying in the prone position by changing his posture regularly with rotating bed, and turning him over to a prone position twice a day, for 1 h each time. (2) We used 48 ml of 0.9% sodium chloride solution and rapid-acting insulin to lower his blood glucose level within a week, and this level was maintained at 7-12 mmol/L. (3) Infusion of plasma and saline for fluid resuscitation and antishock therapy, administration of norepinephrine to maintain a mean arterial pressure of 65 mmHg, injection of amiodarone to treat arrhythmia, and urinary alkalinization to protect renal function. (4) A systemic anti-infection treatment. (5) Debridement (thoroughly cleaning the wound and removing all infected and nonviable (necrotic or dead) tissue. At the same time, specimens of necrotic tissue and secretions were collected for bacterial culture and drug-susceptibility testing. Some lesions were cut and sent for pathological examination. The result of the bacterial culture was reported as staphylococcus aureus, and the antibiotic was changed according to the result of drugsusceptibility testing [8]. The pathological result indicated an acute suppurative inflammation. Iodoform gauze dressings were given and the frequency of dressing changes was 3 times/day [9].
When the vital signs were stabilized, abscess resection was performed in the prone position under general anesthesia on December 14th, 2020. During surgery, we found that the abscess had invaded the deep muscles, fascia, and even a part of the bone tissue. It had invaded both sides of the sternocleidomastoid muscle up to the periphery of the carotid sheath; thus, the infectious lesion could not be completely removed. Since the abscess cavities were distributed in a honeycomb-like pattern and were not connected to each other, the abscess cavities that were visible to the naked eye were cut open, repeatedly washed with iodophor disinfectant, and treated with negative pressure. Around every 4 days, the wounds were expanded and negative pressure was applied until the honeycomb-like abscess cavities in the deep tissues were fully drained (Figure 1B-1D) [10]. On January 7th, 2021, the reexamination of various laboratory indicators showed the following outcomes: WBC count, 7.69 × 109/L; proportion ofneutrophils, 69.8%; PLT count, 185 × 109/L; PT, 16.1 s; APTT , 53.8 sRBC, 2.59 × 1012/L; Hgb, 80 g/L; GLU, 5.4 mmol/L; ALB, 33 g/L; SCr, 165 umol/L; UA, 246 umol/L; urine GLU, normal; and urine KET, negative. The proliferation of granulation tissue on the wound was obvious and inflammation around the wound gradually decreased on January 14th, 2021. The back split-thickness skin was removed and made into a mesh skin (ratio 1:1.5) which was transplanted on the nape under general anesthesia (Figure 1E). Following the surgery, negative pressure wound therapy was also used to fix the transplanted skin, and the wound was sealed for drainage treatment. The wound was completely healed 2 weeks later (Figure 1F).
Skin disorders may appear as the first sign of DM and develop at any time in the course of the disease [11]. Carbuncle often occurs in middle-aged and elderly diabetic patients who have a poor blood glucose control for a long time [4,12]. A neck abscess is easy to invade and deep neck space infections involve deep fascial space in the head and neck areas [13]. Severe infections may cause sepsis and septic shock if the carbuncle is not treated in a timely manner [2,4,8,13]. Therefore, clinicians should pay further attention to such patients.
This diabetic patient had a poor blood glucose control. When he was admitted to our hospital, the levels of GLU, urine GLU, and urine KET were 43.5, 56 and 1.5 mmol/L respectively. He had developed DKA with unconsciousness. The giant carbuncle in the nape can invade and spread to the deep muscles, fascia, and even bone tissues, causing systemic sepsis [14,15]. Severe infections further aggravated diabetic nephropathy and caused acute kidney damage [4,16]. At the same time, the patient was 72 years old, suffered from basic diseases of hypertension and arrhythmia for several years, and he was bedridden for a long time, which resulted in laborious expectoration and pneumonia. Therefore, after the patient was admitted to our hospital, for a better airway management, he underwent tracheal intubation and NIV. We closely monitored BP and HR when anti-shock drugs were infused, rapid-acting insulin was administrated to control blood sugar, and urinary alkalinization was undertaken to protect kidney function. The anti-infective approach can be selected as topical, oral and intravenous according to the condition of infection [8,17]. A systemic anti-infection therapy was performed based on the results of drug-susceptibility testing for this patient; even debridement was used to remove the infected foci as much as possible.
Whether it is nape carbuncle or back carbuncle, it is more difficult to care for the patient's wound [6,7]. Our experience is to use a rotating bed for such patients. On the one hand, it can assist the patient in prone ventilation, which is beneficial for sputum discharge, and can prevent pressure sores on the buttocks and back caused by long-term supine position. On the other hand, it is convenient for debridement on the nape or back after turning over. Carbuncle is a progressive disease, superficial and local infection of lesions can rely on topical antibiotic ointment, minimal incision, drainage and irrigation with antibiotic-containing solution, even photodynamic therapy [18]. However, the neck structure is complicated, and it is a critical challenge to treat the huge infected lesions. While when the infection spreads to deeper area, simple debridement and drainage cannot completely solve the problem [1]. Giant carbuncles must be surgically removed and the infected lesions must be fully resected to prevent recurrence [13,19]. For some residual hidden infected lesions that could not be completely removed, negative pressure wound therapy was used to strengthen the drainage through negative pressure, which could also promote the hyperplasia of granulation tissue to fill in some tissue defects after excision of giant carbuncles [7,20]. We proposed a treatment strategy for different carbuncles, as show in Figure 2.
Figure 2: Treatment strategy for carbuncles.
Finally, how to repair the wound is also an important issue to consider. Some literature reports that wound closure relies on dressing change to heal eventually, but the time is longer or the healing quality is poorer [9,13]. A split-thickness mesh skin (expansion ratio 1:1.5) graft was used to coTreatment strategy for carbuncles.ver the wound for this patient. We find the survival rate of mesh skin transplantation was credible, and it was conducive to the continuous excretion of wound-based secretions. Therefore, it is necessary to completely remove the giant carbuncle and repair the wound as soon as possible. It is worth noting that after thorough debridement, it is more reliable to use autologous reticular thick skin transplantation after the granulation tissue is fresh or treated with negative pressure [6,7]. In addition, if it is a carbuncle on the face, incision and drainage can be followed by flushing and dressing changes, literatures reported that good results can be achieved without skin grafting [9,21,22].
Skin infections are common in middle-aged and elderly diabetics. A prompt diagnosis is feasible, however, it may cause sepsis due to poor control of diabetes and severe infection. For carbuncles, we believe that the most important therapy is to drain pus sufficiently or excise lesions, which is the first step in saving a patient’s life before systematic treatment. For small carbuncle, it can be healed through various methods of drainage and local anti-infection therapy. For huge carbuncle, secondary wound repair is required after excision,and we think the combination of negative pressure drainage and mesh skin grafting may be a better choice, which guarantees effectiveness and aesthetics, especially for giant nape carbuncle.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Wang X, Zhu F, Tang H, Xiao S, Hu X (2022) Treatment for Giant Nape Carbuncle Complicated by Diabetic Ketoacidosis and Sepsis: A Case Report and Literature Review. J Clin Exp Dermatol Res. 13:619.
Received: 10-Oct-2022, Manuscript No. JCEDR-22-19520; Editor assigned: 12-Oct-2022, Pre QC No. JCEDR-22-19520 (PQ); Reviewed: 26-Oct-2022, QC No. JCEDR-22-19520; Revised: 02-Nov-2022, Manuscript No. JCEDR-22-19520 (R); Published: 09-Nov-2022 , DOI: 10.35248/2155-9554.22.13.619
Copyright: © 2022 Wang X, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.