
Anesthesia & Clinical Research
Open Access
ISSN: 2155-6148

ISSN: 2155-6148
Research Article - (2020)Volume 11, Issue 10
Background: The purpose of this study is to determine the trend of usage of vasopressors in the United States from 2005 to 2014 using a robust database.
Methods: Data from the Agency for Healthcare Research and Quality’s Nationwide Inpatient Sample (NIS) was queried from 2005-2014 for the patients who received vasopressors. Data was dichotomized to teaching and non- teaching institutions. Z-tests were performed using statistical analysis to assess for significant differences.
Results: The usage of Vasopressor Infusion procedure increased by an overall 143% in all hospitals across the US between 2005 and 2014. This increase was particularly seen among teaching hospitals that reported a 246% increase in vasopressor use, compared to non-teaching hospitals that showed a 2% increase. The difference between vasopressor infusions among teaching and non-teaching hospitals was significant in 2010 and 2012-2014 (p-value<0.05).
Conclusion: Our data demonstrates increased overall usage of vasopressors in American hospitals, particularly among the teaching hospitals in the recent years. Further studies are needed to stratify this data among different clinical uses in order to assess factors that explain the association of teaching status with vasopressor use.
Vasopressor; Hospital teaching status; Critical care
Vasopressor use leads to increased systemic vascular resistance leading to increased mean arterial pressure and increased perfusion to organs, which is particularly useful during arterial hypotension in shock [1]. Vasopressor use has been widely described in numerous settings including Intensive Care Units (ICU), emergency medicine, anesthesia, cardiac careunits, obstetrics and more. Vasopressors are especially common in the ICU setting where they can supplement fluid resuscitation in maintaining perfusion pressures in the setting of sepsis, hemorrhage and shock [2]. In fact, high dose vasopressor use has even been demonstrated to be an independent predictor of ICU and hospital mortality [3].
While vasopressor use has been indicated in a myriad of critically ill patients, use of vasopressors also has its share of adverse effects including severe hypertension, cardiac ischemia, acute limb ischemia, arrhythmias and even, mortality [4,5]. Excess use of vasopressors can lead to iatrogenic vasoconstrictive shock in patients with poor cardiac function [6]. And though many studies exist describing the indications and adverse effects of vasopressors, few exist to investigate whether vasopressor use has increased in recent years, and whether any differences in this rate of use exist among teaching and non-teaching hospitals. Our study aims to explore the trend of use of vasopressors in teaching and non- teaching hospitals in the United States from 2005-2014 with the goal of better understanding the amount of usage of vasopressors in hospital medicine.
We conducted a retrospective cohort study utilizing the Healthcare Cost and Utilization Project network (HCUPnet) national database to investigate vasopressor use in teaching vs. non-teaching hospitals between 2005 and 2014. HCUP is a national database and software tool sponsored by the Agency for Healthcare Research and Quality (AHRQ). The database represents the most extensive collection of longitudinal hospital care data in the United States, including the synthesis of data from state healthcare centers, hospital associations, private institutions, and the Federal government.
We identified patients categorized under ICD-9 code 00.17, who received infusion of Vasopressor anytime during their hospital course. Trends during the ten years were compared between teaching and non-teaching hospitals and evaluated using the z-test statistic and P values using a two-tail test with a significance of less than 0.05. The HCUP is an anonymous database and fully complied with the ethical standards and received "exempt" status from the Institutional Review Board (HSC-2015-0408N).
We evaluated 757,537 patients who received a vasopressor infusion in hospitals from 2005-2014. The mean age was 74.4 (± 5.4) years old and the most common age subgroup consistently were 65-84 (45.70% average over the study period). The cohort was mainly Male, 54.26% (± 1.02) over the study period (p=0.24). The incidence of vasopressor infusion, as noted by HCUP, increased during the study period from 48,146 in 2005 to 116,930 in 2014 (143% increase, p=0.001). Specifically, incidence increased from 22,184 to 22,720 from 2005-2014 in non-teaching hospitals (2% increase, p=0.9) and 25,962 to 89,715 in teaching hospitals (246% increase, p=0.001) (Table 1).
| Total | Total rate per 100 K persons | Male rate per 100 K persons (%) | Age rate per 100 K persons (%) | Teaching hospitals total (%) | Non-teaching hospitals total (%) | p-value between teaching and non-teaching | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2005 | 48,146 | 16.3 | 18.1 (54.71%) | -<1 | -18 | -62 | -110 | -149 | -85+ | 25,962 (46.08%) | 22,184 (53.92%) | 0.69819 |
| NA | NA | 2.9 (6.87%) | 17.4 (26.39%) | 72.9 (48.41%) | 133.6 (13.03%) | |||||||
| 2006 | 58,026 | 19.4 | 21.4 (54.14%) | NA | NA | 3.8 (7.44%) | 21.8 (28.23%) | 85.2 (47.45%) | 135.3 (11.35%) | 36,457 (62.83%) | 21,569 (37.17%) | 0.10709 |
| 2007 | 66,117 | 21.9 | 24.4 (54.57%) | 48.3 (3.03%) | 0.9 (0.98%) | 4.6 (7.84%) | 25.6 (29.80%) | 95.0 (47.10%) | 147.5 (11.24%) | 25,862 (39.12%) | 40,255 (60.88%) | 0.09024 |
| 2008 | 59,356 | 19.5 | 21.8 (54.88%) | 35.4 (2.45%) | 1.0 (1.22%) | 4.1 (7.82%) | 23.6 (31.31%) | 81.3 (45.97%) | 128.0 (11.20%) | 35,084 (59.11%) | 24,272 (40.89%) | 0.11218 |
| 2009 | 64,100 | 20.9 | 23.0 (54.20%) | 50.6 (3.16%) | NA | 4.2 (7.45%) | 24.4 (35.8%) | 85.2 (45.55%) | 141.3 (11.83%) | 37,907 (59.14%) | 26,016 (40.59%) | 0.16991 |
| 2010 | 76,198 | 24.6 | 27.0 (53.94%) | 57.4 (2.98%) | 1.3 (1.21%) | 5.6 (8.34%) | 29.1 (31.25%) | 98.9 (45.32%) | 149.8 (10.9%) | 48,006 (63.0%) | 26,798 (35.17%) | 0.02436 |
| 2011 | 72.374 | 23.2 | 25.2 (53.39%) | 38.0 (2.08%) | NA | 5.6 (8.78%) | 29.3 (33.52%) | 88.1 (43.39%) | 142.4 (11.24%) | 42,198 (58.31%) | 27,440 (37.91%) | 0.07903 |
| 2012 | 90,590 | 28.9 | 31.6 (53.88%) | 46.4 (2.02%) | 1.5 (1.19%) | 6.5 (8.22%) | 36.0 (32.95%) | 108.0 (44.41%) | 172.7 (11.21%) | 58,295 (64.35%) | 27,635 (30.21%) | 0 |
| 2013 | 105,700 | 33.4 | 36.7 (54.04%) | 45.8 (1.71%) | 1.6 (1.04%) | 7.7 (8.31%) | 42.0 (32.99%) | 123.4 (45.14%) | 189.0 (10.80%) | 69,430 (65.69%) | 30,685 (29.03%) | 0 |
| 2014 | 116,930 | 36.7 | 40.9 (54.88%) | 52.4 (1.77%) | 2.1 (1.23%) | 9.2 (9.06%) | 46.8 (33.46%) | 129.2 (44.29%) | 193.3 (10.19%) | 89,715 (76.73%) | 22,720 (19.43%) | 0 |
Table 1: Trend of vasopressor infusions (number) through 2005-2014 in teaching and non teaching hospitals.
The percentage of vasopressor infusion that occurred in teaching hospitals was also observed to be steadily increasing going from 53.92% -76.73% from 2005-2014 and steadily decreasing from 46.08% to 19.43% in non-teaching hospitals in the same study period (Figure 1). The incidence of Vasopressor Infusion procedure between teaching and non-teaching hospitals was not significantly different between the years of 2005 to 2009 and 2011 (p-value>0.05, Table 1). However, in 2010 and 2012 onwards, there was a significant difference between the numbers of Vasopressor Infusions between teaching and non-teaching hospitals (p-value<0.05, Table 1).
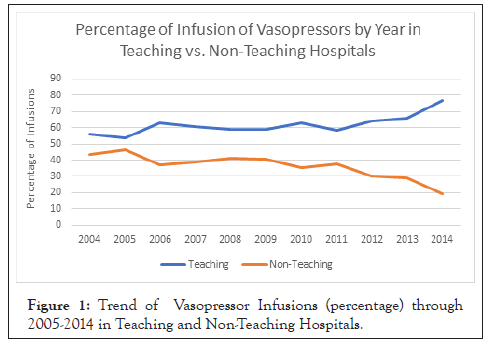
Figure 1: Trend of Vasopressor Infusions (percentage) through 2005-2014 in Teaching and Non-Teaching Hospitals.
Our study reflects that there has been an overall increase (143%) in vasopressor infusion in hospitals across the United States during the 10-year study period of 2005-2014. We also observe that the age group receiving these infusions is particularly the 65-85 age range, making up an average of 45.70% of all the patients over the study period (Table 1). This supports previous research that states that patients over the age of 65 comprise more than half of all ICU admissions in the ICU, where vasopressor infusions are likely to be used [7]. In particular, we observe vasopressor infusions occur in greater numbers and percentages in teaching than non-teaching hospitals. We observe a 246% increase in vasopressor infusion in teaching hospitals during the study period and a 2% increase in non-teaching hospitals. Moreover, more difference in vasopressor infusions among teaching and non-teaching hospitals are seen in the last few years of this study.
Interestingly, Raffa et al. observed a decreasing trend of vasopressor usage in ICU patients between the years of 2003-2011, attributed to prolonged use of vasopressor leading to higher mortality in these patients [8]. These results contradict what we observed, an overall increase in vasopressor infusion however our study periods are different. Further, it’s important to note that our study focused on all hospital patients rather than just critical care patients and one possible explanation for the greater use of vasopressors that we observed is the discovery of benefits of vasopressor therapy in a variety of new settings, outside the ICU. While vasopressor therapy has been a mainstay in vasodilatory shock and ACLS treatment for decades, vasopressors have also been found to be useful in prevention in cardiogenic shock, decreasing complications in corrective cardiac surgery in patients with pulmonary arterial hypertension, and post cardiopulmonary bypass vasoplegia syndrome, among many others [9-11]. These new discoveries of vasopressors might be contributing to the overall increase in vasopressor infusion that we observed. It is further interesting to note that different vasopressors have been used preferentially in varying settings, such as an uptrending use of norepinephrine in ICU and an increased use in phenylephrine in the operating rooms [12,13]. Recent research on novel vasopressor agents has also led to the discovery of Angiotensin II approved in the USA and other novel agents such as terlipressin that are approved for use outside the US. The discovery of these new agents may also contribute to increased overall vasopressor infusion that we observed in our study [14].
Our analysis of the increases in vasopressor infusions demonstrated that these increases primarily occurred in the teaching hospitals. While non-teaching hospitals decreased the percentage of vasopressor infusions from 46.08% to 19.43%, teaching hospitals increased their use in patients, from 53.92% to 76.73% (Figure 1). Currently, there are little to no studies of this kind comparing medication usage in teaching hospitals vs non-teaching hospitals, therefore this study presents novel results showing use of vasopressors have been rapidly increased in teaching hospitals in recent years compared to non-teaching hospitals. While there are likely several factors contributing to this difference, the most likely one we theorize is that the acuity of patients is much higher in teaching hospitals than it is in non-teaching hospitals. This has been supported by studies showing higher illness severity in the patient case load in teaching hospitals as compared to non- teaching hospitals [15,16]. Shahian et al. found that part of the reason for this difference in illness severity of teaching and non- teaching hospitals might be contributed by the fact that teaching hospitals tend to serve a greater portion of minority populations and patients requiring transfer from other hospitals for advanced care, many of whom are complex and severely ill [17]. This idea supports the greater number of critically ill patients that may be requiring vasopressor infusions.
While vasopressors have a variety of uses as discussed earlier, these drugs aren’t without their adverse effects and recent studies show independent association of early vasopressor use in critically ill patients and therefore should be used in caution. Further investigations on multiple variables would be helpful in aiming the research specifically at ICU patients between teaching and non-teaching hospitals, adjusting for illness severity, and exploring other factors contributing to the differences in hospital teaching status, and understanding better in which conditions and settings vasopressor infusions were primarily used. This could help understand the appropriateness of current vasopressor use trends, as well as better understanding how our healthcare differs among teaching and non-teaching institutions.
Our data demonstrated an overall increase in vasopressor infusions in all hospitals across the United States in the study period of 2005- 2014, with higher usage among teaching hospitals. This difference may support difference patient complexity and acuity in teaching hospitals requiring greater vasopressor usage.
None to declare
None to declare
None to declare
AY: writing the manuscript and entire analysis; SA: Editing and writing, AS: mentor and design of the project. All authors read and approved the final manuscript.
Not applicable.
The data supporting the findings of this study are available to public at: https://hcupnet.ahrq.gov/#setup
Citation: Yarram A, Abughazaleh S, Seifi A (2020) Trend of Usage of Vasopressors in the United States. J Anesth Clin Res. 11: 971.
Received: 05-Oct-2020 Accepted: 19-Oct-2020 Published: 26-Oct-2020 , DOI: 10.35248/2155-6148.20.11.971
Copyright: © 2020 Yarram A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.