Clinical Pediatrics: Open Access
Open Access
ISSN: 2572-0775
ISSN: 2572-0775
Case Report - (2024)Volume 9, Issue 4
The novel coronavirus was first discovered in China, 2019. With the increase of cases worldwide, the WHO declared the outbreak as a pandemic. Many reports emerged describing the characteristics of this disease. The incidence of infection in the pediatric group has been less compared to the adult. The clinical presentation among pediatrics has been widely variable ranged from asymptomatic to critical. The respiratory symptoms and signs have been more frequent than gastrointestinal. In this report, we present two pediatric cases presented with fever and gastrointestinal symptoms without any respiratory symptoms or signs. However, the chest CT scan of both cases showed ground-glass densities in the lower lobe of the lung. One case was hospitalized and the other one was home isolated. Both cases received oseltamivir and azithromycin for 5 days, and they were cured. Given that clinical presentation, we hope to add more data as regard COVID-19 among pediatrics to improve the diagnostic and therapeutic guidelines.
COVID-19; CT scan; Gastrointestinal symptoms
Unexplained cases of fatal rapidly spreading viral pneumonia were reported in December 2019, in Wuhan, China. A novel type of coronavirus, SARS-CoV-2, was isolated during the examination of the patients' samples. By May 2019, the novel coronavirus has been responsible for more than 3 million infections worldwide with a case fatality rate up to 7% [1]. Many studies have been made on adults, but attention has been less paid to pediatric patients. Maybe, this is related to the lesser incidence and severity in the pediatric age group besides the wide variations in clinical presentation in the pediatric age group [2]. Most pediatric cases developed fever and cough, but the gastrointestinal symptoms were less common. This disparity in symptoms and severity requires a high level of suspicion for SARS-CoV-2 infection on examination [3]. We would like to report 2 pediatric patients infected with COVID-19 presented with gastrointestinal symptoms with no clinical chest findings although CT scan abnormalities were detected.
Case 1
A nine-year-old male child with no significant medical history presented to the outpatient clinic after 2 days of high-grade fever 39.5°C and a sudden onset of loss of taste associated with anorexia. There was no cough or any other symptoms of respiratory tract infection. One day before seeking medical advice, he developed sudden onset of watery diarrhea with 6 motions of loose watery stool of yellowish color associated with mild crampy abdominal pain without vomiting or any other gastrointestinal symptoms. On the initial assessment, his temperature was 39.5°C, pulse 130 beats per minute, respiratory rate 35 breaths per minute with no signs of retractions, and blood pressure 120/70. The chest examination revealed a bilateral equal air entry with scattered sonorous rhonchi. Heart, abdomen, and neurological examinations were free, and there were no signs of dehydration. The child has a history of contact with his uncle who was diagnosed as COVID-19 positive patient and was hospitalized due to bronchopneumonia.
Initial laboratory data were CBC Hb 11 g/dl, Platelets 150,000, TLC 3000 with lymphocytes 10%, CRP 200 mg/l, ABG PH 7.34, PCO2 45 mmHg, PO2 90 mmHg, HCO3 22 mmol/l, LDH 1100 U/l serum ferritin 1000 ug/l, and normal kidney and liver functions. Patient O2 saturation was 95% on room air. Initial blood cultures were withdrawn before starting treatment. According to the hospital policy, a nasopharyngeal swab was sent for PCR. Cultures were negative for bacterial growth. PCR for virology was positive for SARS-CoV-2. The PCR method used was COVID-19 genesig real-time PCR (rtPCR) assay (Primerdesign, Chandler’s Ford, UK), targeting the RNA dependent RNA polymerase gene. The amplification was performed on the Light Cycler 480 instrument (Roche Diagnostics, Mannheim, Germany).
Although the child did not complain of any chest symptoms or even cough, Chest X-Ray (CXR) and CT scan were done. CXR revealed a mild increase in the bronchovesicular markings. (Figure 1) CT scan showed the right lower lung lobe with subsegmental patchy areas of air space consolidation with ground-glass densities of infectious or inflammatory origin. (Figure 2). The patient was home isolated, and the initial medication was started as oseltamivir oral 75 mg once daily for 5 days, azithromycin oral 20 mg/kg every 24 hours for 5 days, oral paracetamol 20 mg/kg every 6 hours until fever resolved within 24 hours, Vitamin D3 1000 IU/day, Vitamin C 100 mg/day, and oral zinc syrup 1 mg/kg/day. After 10 days, his symptoms improved with 2 negative PCR 72 hours apart. Taste sensation was regained after 2 weeks from discharge. Follow up chest CT scan was free after 1 month from the discharge date.
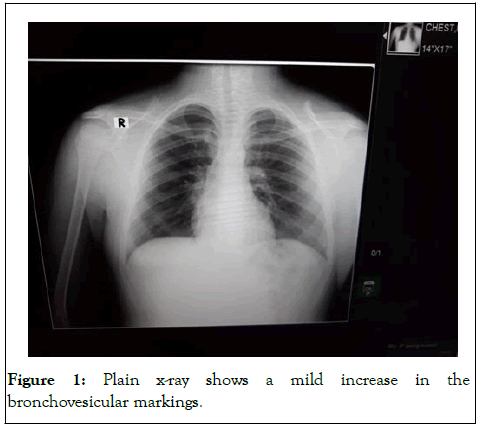
Figure 1: Plain x-ray shows a mild increase in the bronchovesicular markings.
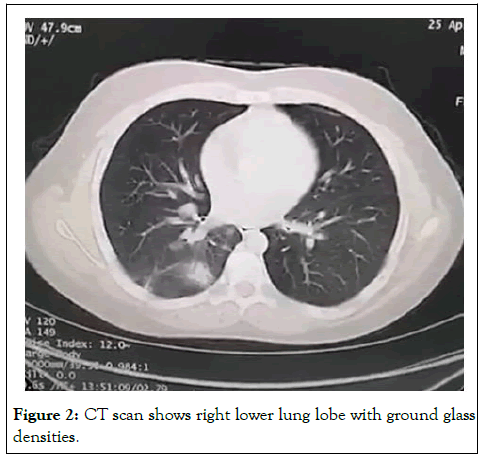
Figure 2: CT scan shows right lower lung lobe with ground glass densities.
Case 2
A one-year-old male child with no significant medical history presented with high-grade fever 40.5°C for 2 days, sudden onset of vomiting 4-5 times per day yellowish vomitus with undigested food, and refusal to food intake. No cough or any other symptoms of respiratory tract infection were present. No dehydration, diarrhea, or any other gastrointestinal symptoms.
The initial assessment was temperature 40°C, pulse 160 bpm, respiratory rate 42 breaths per minute with no signs of retractions, and blood pressure 90/60 mmHg. The chest examination revealed a bilateral equal air entry with no adventitious sound. Heart, abdomen, and neurological examinations were free, and there were no signs of dehydration. His mother was diagnosed as COVID-19 positive patient and was hospitalized due to bronchopneumonia 3 days before the patient started his complaint.
Initial laboratory data were CBC Hb 10 g/dl, PLT 100,000, TLC 1500 with lymphocytes 20%, CRP 150 mg/l, ABG PH 7.4, PCO2 40 mmHg, PO2 95 mmHg, HCO3 27 mmol/l, LDH 900 U/l, serum ferritin 900 ug/l, and normal kidney and liver functions. Patient O2 saturation was 100% on room air. Initial blood cultures were withdrawn before starting treatment. A nasopharyngeal swab was sent for PCR. Cultures were negative for bacterial growth. PCR for virology was positive for SARSCoV- 2. Although the child did not complain of any chest symptoms or even cough, Chest X-Ray (CXR) and CT scan were done. CXR was normal (Figure 3). CT scan showed the left lower lung lobe with subsegmental patchy areas of air space consolidation with ground-glass densities of infectious or inflammatory origin (Figure 4).
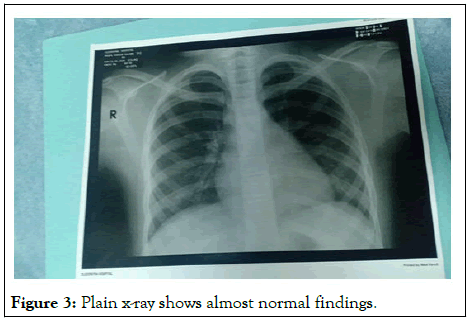
Figure 3: Plain x-ray shows almost normal findings.
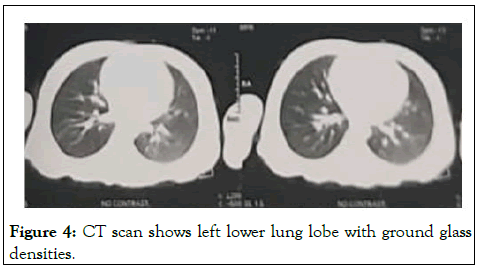
Figure 4: CT scan shows left lower lung lobe with ground glass densities.
The initial medication was started as oseltamivir oral 3 mg/kg/day every 12 hours for 5 days, azithromycin oral 20 mg/kg every 24 hours for 5 days, oral paracetamol 20 mg/kg every 6 hours until fever resolved after 24 hours, Vitamin D3 1000 IU/day, Vitamin C 100 mg/day, oral zinc syrup 1 mg/kg/ day, and ondansetron IM 0.15 mg/kg every 8 hours until vomiting stopped after 4 days. Oral rehydration solutions were given to prevent dehydration. The patient was discharged after one week of hospital admission and was isolated at home. His PCR result was negative after 2 nasopharyngeal swabs 72 hours apart on day 13 from the initial swab. Follow up Chest CT scan was normal after 1 month (Figure 5).
Figure 5: Follow up normal chest CT scan.
On 11th March 2020, The world health organization announced the SARS-CoV-2 outbreak a pandemic [4]. Many cases have been recorded worldwide since the outbreak in China. Adults have represented most cases. The incidence of infection among the pediatric age group <18 years was 1.7% and 2.4% in the US and China, respectively [5,6]. To our knowledge, there is a lack of accurate data regarding pediatric cases in Africa at present. In our report, we present two cases 9 and 1 years old. There is a disparity noticed in the severity of infection among children ranged from asymptomatic to critical, but most cases had mild symptoms including fever, fatigue, myalgia, cough, sore throat, runny nose, and sneezing [7].
In our report, both patients presented with high-grade fever which is like most of the reported cases. The first patient had acute taste loss which resolved 2 weeks after the PCR result became negative for the virus. This correlates with the findings reported by Yan and her colleagues. Of the COVID-19 positive patients, 71% had a loss of taste which resolved with the clinical resolution of illness [8]. The first and second case’s main presentations were diarrhea and vomiting, respectively. Gastrointestinal symptoms are less frequent among pediatric patients [9]. Neither of the patients underwent a rectal swab.
Interestingly, both cases had no respiratory symptoms and minimal signs. They had normal chest X-ray findings, but the CT scans showed ground-glass appearance. Despite these findings, they are not specific to COVID-19. Other pathogens may have the same effect on the lung. Also, some children may have no radiographic abnormalities. Chest radiograph or CT alone is not recommended for the diagnosis of COVID-19 [5]. The American College of Radiology also does not recommend CT for screening or as a first-line test for diagnosis of COVID-19. Currently, there are no studies that compare the chest radiograph with CT or other radiologic tests (lung ultrasonography) to assess COVID-19 in children [10].
As regards the management, they were hospitalized and isolated. We used oseltamivir (antiviral), azithromycin (antibacterial) for the fear of secondary bacterial infection, and oral paracetamol. Both cases did not need respiratory support. They improved with treatment and were discharged after two negative nasopharyngeal swabs. Patients were asked to continue home isolation for two weeks. At present, there is insufficient data to recommend for or against the use of specific antivirals or immunomodulatory agents for the treatment of COVID-19 in pediatric patients. Based on these findings, children with COVID-19 can present with different symptoms that may overlap with other pathogens. The respiratory symptoms are not essential to suspect COVID-19 infection. Patients can be physically free on examination; however, their CT scan may show abnormal findings. Both cases had a history of contact with an infected family member. With the spread of infection, updated diagnostic and therapeutic guidelines are required for pediatric patients.
To conclude, the diagnosis of primary immunodeficiencies entails combining the observed clinical phenotype with immunological and genetic analyses. This combination of clinical and basic scientific approach is now a prerequisite for gaining new insights into immunological mechanism and therefore provide information for better diagnosis and management of these rare disorders. Keeping in mind that a high index of suspicion has a key role in this regard and it is considered as the initial step for further evaluations.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Rezk AR, Ibrahim HM (2024) Two Pediatric COVID-19 Presenting with Gastrointestinal Symptoms and Abnormal Chest CT Findings without Respiratory Symptoms. Clin Pediatr. 09:273.
Received: 16-Apr-2020, Manuscript No. CPOA-24-4861; Editor assigned: 22-May-2024, Pre QC No. CPOA-24-4861 (PQ); Reviewed: 05-Jun-2020, QC No. CPOA-24-4861; Revised: 16-May-2024, Manuscript No. CPOA-24-4861 (R); Published: 18-Jul-2024 , DOI: 10.35248/2572-0775.24.09.273
Copyright: © 2024 Rezk AR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.