Reproductive System & Sexual Disorders: Current Research
Open Access
ISSN: 2161-038X
ISSN: 2161-038X
Research Article - (2023)Volume 12, Issue 1
Background: Complications and obstetric emergencies were taken as an indicator of obstetric need. Obstetric needs are a health problem that needs emergency obstetric intervention. The assessment of unmet obstetric need has never been articulated in studies conducted on emergency obstetric care in the study area. This study identifies gap and deficit of major obstetric intervention for absolute maternal indication in relation to the existing need.
Method: A one year facility based cross-sectional retrospective study was conducted from July 8/2019-July 7/2020 G.C on mothers who delivered with major obstetric intervention (absolute maternal indication and non-absolute maternal Indication) at Debre Berhan referral hospital. Data was collected using structured and pre-tested format by four midwife trained data collectors from patient medical records. Rates of major obstetric interventions performed for absolute maternal indications among all expected births was calculated to assess unmet obstetric need. Training and using structured format were used to ensure the data quality in addition to supervision.
Result: A total of 363 major obstetric interventions were conducted in the study area. The result revealed that the unmet obstetric need of the area was 31.4%. Caesarean sections took the largest share of major obstetric interventions 358 (98.6%). Out of 153 women with absolute maternal indications majority were cephalo-pelvic disproportion which account 87 (24%). The number of major obstetric interventions done without absolute maternal indications was 210 (57.8%) where majority 78 (29.5%) were done for fetal distress.
Conclusion and recommendation: There was higher unmet obstetric needs in rural than urban areas. Even though maternal mortality has been declining and no death was observed. The caesarean section rate was 2.3% this was below the world health organization recommendation 5% to 15%. Estimating the amount of unmet need for major obstetric interventions provide the information necessary for planning and prioritizing the development of services; and lead to action for the reduction of maternal mortality at local level.
Unmet obstetric need; Major obstetric intervention; Absolute maternal indication
AMI: Absolute Maternal Indication; APH: Ante Partum Hemorrhage; CPD: Cephalo Pelvic Disproportion; EB: Expected Birth; EmONC: Emergency Obstetric and Neonatal Care; MOI: Major Obstetric Intervention; MMR: Maternal Mortality Ratio; PPH: Post-Partum Hemorrhage; RR: Relative Ratio; UN: Unmet Need; UON: Unmet Obstetric Need
The concept of unmet obstetric need refers to the discrepancy between what the health care system should do to deal with the obstetric problem in a given population, and the care it actually delivers. Operationally, unmet obstetric need is expressed in terms of women who should have benefited from obstetric interventions, but for whom this intervention did not take place [1].
The unmet obstetric need network is the system that bring together ministers of health, development organization, scientific institution and practitioners who want to plan unmet need for major obstetric for absolute maternal indications as a starting point not just to improve maternal health but also the overall functioning of the health care system. The unmet obstetric need network provides technical support national teams involved in this kind of work, as well as opportunities to learn from each other.
The European commission and a number of other agencies decided to launch a formal UON network. The unmet obstetric need network brought together ministries of health, development organizations, scientific institutions and practitioners who wanted to map unmet need for “major obstetric interventions for absolute maternal indications” as a straight point to improve maternal health care and the overall functioning of their health care system.
The unmet obstetric need concept developed by the unmet obstetric need network considers unmet need by including major obstetric interventions that are done for absolute maternal indications and the gap between those expected and those actually done [2,3].
The discrepancy between the expected and observed major obstetric intervention rate for absolute maternal indications, including CS, hysterectomy and destructive operations, is a powerful indicator of the unmet need for life saving obstetric care [4] (Figure 1).
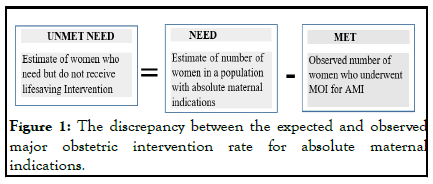
Figure 1: The discrepancy between the expected and observed major obstetric intervention rate for absolute maternal indications.
Operational expression of the unmet obstetric needs concept adopted from previous study. The obstetric need is expressed in terms of the health problems, which necessitate an intervention, by the health care system. Among indications for intervention some are more essential to the survival of the mother and the child and others. These are called “Absolute Maternal Indications (AMI)” and it is on this basis that the indicator of obstetric is constructed. It is necessary, if the indicator is confined to major obstetric interventions for absolute maternal indications (MOI/AMI), in a way that is most relevant to the planning of the minimum interventions required. The AMI are severe ante partum hemorrhages caused by the placenta praevia or a retro placental hematoma (premature detachment of a normally inserted placenta), incoercible post-partum hemorrhages, major foeto-pelvic disproportions (due to narrow pelvis or a hydrocephaly), transverse positions (shoulders neglected) and face presentation [5,6].
The major obstetric interventions for absolute maternal indications comprises caesarean section, laparotomies, hysterectomies, internal versions, craniotomies or embryotomies and symphysiotomy which may be carried out to avoid a caesarean in a case of cephalo-pelvic disproportion [7].
Globally, 289,000 women died from pregnancy related complications in 2015, half of them due to hemorrhage, hypertensive disorders and sepsis [8,9].
Number of facilities with emergency obstetric service is an important indicator. According to UN recommendations, there should be at least one comprehensive and four basic EmOC facilities per 500,000 populations. An estimated 15% of pregnant women develop major direct obstetric complications that require medical care, so the recommendation is that at least 15% births should take place in EmOC. This estimated through the met obstetric need which is an indicator for the interventions conducted for those with AMI should be 100% with the expectation that all women in need of major intervention get it from the health system [10,11].
The unmet obstetric need assessment in five African countries, Benin, Burkina Faso, Mali and Niger shows that the percentage of deliveries receiving surgery for absolute maternal indications was 1.4% in urban areas with functioning hospitals the UON network states, 1.4% was practical low end estimate of the proportion of deliveries that require MOI to avoid maternal death [12].
A survey conducted in seven poor African countries only 1.1% of urban and 0.3% of rural mothers actually benefited from major obstetric interventions. In other word the deficit if unmet obstetric need was 25% in urban and 79% in rural areas [13].
Study conducted to assess UON in Zambia, revealed that unmet obstetric need was 41%. The rural population that suffered the entire deficit, was 73% implying that 77 out of 106 women and unmet needs in 2010. Further, the likelihood of undergoing a major obstetric intervention was 5.5 times higher in women from urban compared to rural areas, which underscores the unacceptably large inequity between urban and rural societies. The substantial rural-urban disparity demonstrated in the present analysis of unmet obstetric needs should alert policy makers and the health care system to improve lifesaving services to rural areas. The commonest indication for major obstetric intervention was cephalo-pelvic disproportion.
Post-operative complications significantly dropped between 2008 and 2012 among patients presenting with non-AMI (P=0.008). No significant change was observed in patient AMI. The most frequent AMI were CPD 71% versus 70%, followed by uterine rupture and pre-rupture. Previous C/S was the main non AMI in 2008 (35%) and 2012 (37%).
Retrospective assessment of UON in Dawro zone, 585 of mother with life threatening was obstetric complications was unable to get intervention and this was interpreted as the number of women who should have helped from a lifesaving intervention but actually did not. Major obstetric interventions for AMI rate of 0.8% and caesarean section took the largest share (81.5%) and the commonest AMI was obstructed labor 39.5%.
Met need for EmONC in all facilities was below 50% in all regions even as low as 3% in Gambela, Somali and Diredawa and higher in Addis Ababa 83%. The fully functioning of comprehensive EmONC was 148% of the 184 recommended leaving a gap of 36 facilities. The least available facility was in SNNP and Diredawa (22%) and the greatest in Harari (126%) which exceeded the minimum recommended number of EmONC facilities while other regions were below the national average (40%).
Among all maternal deaths, 43% were related to direct obstetric complications, 5% indirect causes and 52% were due to unknown or unspecified causes. In this assessment the leading known cause of death were PPH/retained placenta and APH together responsible for 12% of death and severe pre-eclampsia or eclampsia for 10%, more over 26% of maternal complications were due to other direct obstetric complications but responsible for 12% death.
A review of caesarean cases 74% were found to be maternal indications, 22% were due to foetal indications i.e., foetal distress and mal presentation. Indication related to CPD, prolonged and obstructed labor and arrest disorder 39%, foetal distress and non-reassuring foetal heart rate 13% and previous scar 13% was the leading indication for CS. Elective CS were most common among women with a previous scar was 47%.
A cross-sectional study conducted in Zambia revealed that, major obstetric intervention for AMI were higher in urban 2.1% than in rural areas 0.4%, with an urban to rural rate ratio of 5.5.
There is an important gap regarding the availability of service in women living in areas classified as urban, and thus residing within 10 km of the hospital, the 55 MOIs for AMI represents 0.9% of all deliveries and 183 MOIs for AMI in rural women represents 0.5% of all deliveries.
Thus this study has an important contribution to determine the prevalence of unmet obstetric need and recommendation to decrease maternal mortality for decision maker among the selected community in North Shoa zone, Amhara region, Ethiopia.
Study area and period
Institutional based cross-sectional study was conducted from March 14 to 25, 2021 in Debre Berhan which is located in North Shoa zone, Amhara region. Debre Berhan is capital city of North Shoa which is found 130 km from Addis Ababa in the Northeast direction and also 665 km far from Bahirdar the capital of Amhara region. The study includes five woreda (Debre Berhan, Baso, Angolela tera, Asagirt and Ankober) those who do not have primary or district hospital for Comprehensive Emergency Obstetric Care (CEmOC). According to CSA the urban total population was 113,693 out of which 56,995 were male and 56,698 were female and the rural total population was 386,376.
Sample size determination
The population projection for 2017 in this study area was calculated from the 2007 census to be 113,693. Assuming the crude birth rate of Amhara is 31.8/1000 population then a total of 3616 (population*crude birth rate) births from urban and 12287 birth from rural were expected in 2018. Benchmark of the median for five sub-Saharan African countries, Haiti, Morocco and Pakistan 1.4% (EB*1.4%) of births were expected to get major obstetric complications that needs intervention was considered. Therefore a total of 223 births need major obstetric interventions for both urban and rural of the study area.
Sampling technique and procedure
First the main registration book of the operation room where all emergencies registered according to their order was used to list all absolute maternal indications. All the name of the mother and Medical Registration Number (MRN) was selected from register and their chart were selected from medical record unit. All mothers who would get emergency and elective procedures were included. The inclusion criteria were based on the list of diagnosis as recorded by the physicians:
• Any mother with absolute maternal indications.
• Any mother who had received major obstetric interventions.
Data collection and instrument
The information was gathered from hospital records. These are theatre registries, delivery books or obstetric records and other relevant documents. A structured format from previous study was used to gather maternal information as a secondary data.
Four midwife data collectors were recruited. They were preferred because of their orientation on the technical terms stated in the formats and the fact that they read the registries better as they are familiar with the records.
The list of AMI is based on the degree of severity of the indication, the relative stability of its incidence and relatively reproducible diagnosis. The standard list of absolute maternal indications adopted for this study includes:
• Antepartum hemorrhage (placenta praevia or abruption placenta).
• Abnormal presentation (transverse lie or shoulder presentation, face with persistent mento-posterior position or brow presentation).
• Major CPD (due to small pelvis or hydrocephalus; including pre-rupture and rupture of uterus).
• Uncontrollable post-partum hemorrhage.
The list of major obstetric intervention includes:
• Caesarean section.
• Hysterectomy.
• Laparotomy for uterine rupture.
A woman presented with more than one complication, the data collectors were only select the complications believed to be the most life-threatening. The number of women with complications was counted, not the number of complications.
The principal data source was the operating theatre register, where most MOI were recorded. Information about the indications for the intervention and other personal data on the women was obtained from patient delivery files, maternity ward registers and admission records for maternity ward.
Data quality control issue
The quality of data was assured by proper designing of the forms and training of the data collectors and supervisor before the actual data collection. Every day after data collection, forms were reviewed and checked for completeness and relevance by the supervisor and principal investigator and the necessary feedback was offered to data collectors.
Data management and analysis
The collected data was checked for completeness, cleaned manually and entered in to Epi data version 3.1 statistical software and then transferred to SPSS window version 21.0 for further analysis. The data was cleaned again for inconsistencies and missing values. Frequencies were used to summarize descriptive statistics.
The indicator of unmet need for major obstetric interventions for a given population in a given period was calculated as:
• Unmet obstetric need=(Complicated BE × RR)-(Number of MOI for AMI).
• BE=number of births expected on in the period under study.
• RR=reference ratio or low end estimates or benchmark of MOI for AMI from other study.
• Number of MOI for AMI=number of major obstetric interventions for absolute maternal indications carried out in the same population during the same period.
When calculating met need, only one obstetric complication per women should be counted. Data on obstetric complications treated more accurately should be called data on women who experienced at least one major obstetric complication.
Socio-demographic characteristics of mother with major obstetric intervention
The mean age of mothers was 27.5 (SD ± 4.8). Majority 339 (93.4%) are married 15 (4.1%) are single and 8 (2.2) are divorced. Concerning education, none educated 344 (94.4%), read and write 19 (5.2%). While considering the address from patient’s charts, the distance from living area to the hospital in KM was analyzed and 167 (46%) cases more than 10 KM far from the hospital and 196 (54%) cases within 10 KM of radius from hospital (Table 1).
| Age (years) | Frequency | Percent |
|---|---|---|
| 15-19 | 6 | 1.7 |
| 20-24 | 93 | 25.6 |
| 25-29 | 153 | 42.1 |
| 30-34 | 67 | 18.5 |
| 35-39 | 41 | 11.3 |
| 40-44 | 3 | 0.8 |
| Total | 363 | 100 |
| Marital status | ||
| Married | 339 | 93.4 |
| Single | 15 | 4.1 |
| Divorced | 8 | 2.2 |
| Widowed | 1 | 0.3 |
| Total | 363 | 100 |
| Education | ||
| None | 344 | 94.8 |
| Read and write | 19 | 5.2 |
| Total | 363 | 100 |
| Distance from the hospital in KM | ||
| Urban(<10 km) | 196 | 54 |
| Rural(>10 km) | 167 | 46 |
| Total | 363 | 100 |
| Place of delivery | ||
| Debre Brehan referral hospital | 356 | 98.1 |
| Home | 6 | 1.7 |
| Other institution | 1 | 0.3 |
| Total | 363 | 100 |
| Time of admission | ||
| Day | 286 | 78.8 |
| Night | 77 | 21.2 |
| Total | 363 | 100 |
Table 1: Socio-demographic characteristic of mother with major obstetric intervention in Debre Berhan referral hospital, 2021.
Obstetrics profile
Among 363 patient with MOI, majority of mother were Primi 182 (50.1%) Multi 160 (44.1%) and the least one grand multi 21 (5.9%). Most 284 (78.2%) of the mothers have history of ANC follow up, 79 (21.8%) of patient had not ANC follow up (Table 2).
| Parity | Frequency | % |
|---|---|---|
| Primi | 182 | 50.1 |
| Multi | 160 | 44.1 |
| Grand multi | 21 | 5.9 |
| Total | 363 | 100 |
| ANC | ||
| Yes | 284 | 78.2 |
| No | 79 | 21.8 |
| Total | 363 | 100 |
| Present obstetric problem | ||
| Anemia | 7 | 1.9 |
| Preeclampsia diabetes | 22 | 6.1 |
| Heart disease | 14 | 0.3 |
| Multiple gestation | 11 | 1.1 |
| HIV | 9 | 32.5 |
| Total | 54 | 14.9 |
Table 2: Frequency distribution of obstetric profile of MOIs in DBRH, 2021.
The predominant MOI was a CS 358 (98.6%) which was the largest share. Caesarean sections were performed more often in urban (<10 km) areas 195 (53.9%) than in rural areas 167 (46.1%) (Figure 2). The crude CS rate, regardless of indication was 2.3% per expected birth in the study area (Tables 3 and 4).
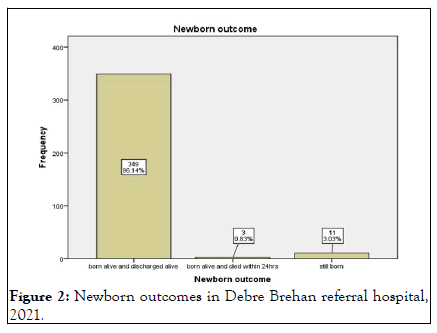
Figure 2: Newborn outcomes in Debre Brehan referral hospital, 2021.
| MOI | Frequency in urban or<10 km | Frequency in rural or>10 km | Total | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| C/S | 195 | 53.9 | 163 | 45.5 | 358 | 98.6 |
| Hysterectomy | 0 | 0 | 5 | 1.4 | 5 | 1.4 |
| Total | 195 | 53.9 | 168 | 46.9 | 363 | 100 |
Table 3: Frequency distribution of major obstetric intervention according to place, 2021.
| Absolute Maternal Indications (AMIs) | <10 km or urban | >10 km or rural | Total | |||
|---|---|---|---|---|---|---|
| Frequency | % | Frequency | % | Frequency | % | |
| Uterine rupture | 0 | 0 | 5 | 1.4 | 5 | 1.4 |
| Obstructed lab or (CPD) | 47 | 13.2 | 39 | 10.8 | 87 | 24 |
| PPH | 3 | 0.8 | 1 | 0.3 | 4 | 1.1 |
| APH for placenta abruptio | 6 | 1.6 | 5 | 1.4 | 11 | 3 |
| APH for placenta previa | 11 | 2.8 | 14 | 3.5 | 25 | 6.3 |
| Two or more previous C/S | 14 | 3.9 | 8 | 2.2 | 22 | 6.1 |
| Total | 81 | 22.2 | 72 | 19.8 | 153 | 42 |
| Preeclampsia | 16 | 4.4 | 4 | 1.1 | 20 | 5.5 |
| Puerperal infections | 1 | 0.3 | 1 | 0.3 | 2 | 0.6 |
| One previous C/S | 20 | 5.5 | 16 | 4.4 | 36 | 9.9 |
| Fetal distress | 51 | 19.3 | 27 | 10.2 | 78 | 29.5 |
| Eclampsia | 0 | 0 | 1 | 0.3 | 1 | 0.3 |
| Other | 38 | 5.8 | 35 | 5.5 | 73 | 11.3 |
| Total | 126 | 35 | 84 | 23 | 210 | 57.8 |
Table 4: Frequency distribution of indications in urban and rural areas, DBRH, 2021.
Maternal outcome: Concerning maternal outcome about 360 (99.2%) reported MOI survived the intervention with no adverse effects and 3 (0.8%) of them develop complication but alive at discharge. About 356 (98.1%) mothers did not develop any immediate complication 4 (1.1%) women developed a complication such as hemorrhage 3 (0.8) develop sepsis. No maternal death was observed after the interventions.
The unmet obstetric need: From a total of 363 major obstetric interventions about 153 major obstetric interventions for absolute maternal indication were carried out during the study period.
Quantification of unmet obstetric need: The unmet need for major obstetric interventions for a given population in a given period is calculated as follows:
• Unmet obstetric need=(EB × RR)-(number of MOI/AMI).
• EB=Expected birth in the period under study.
• RR=Reference ratio of MOI for AMI, number of major obstetric interventions for absolute maternal indications carried out in the same population during the same period.
• EB=15,903 (Expected birth; this is taken from the estimate 2017 population projection), rural EB=12,287 urban EB=3616.
The RR (Reference Ratio) is estimated to be 1.4% (95%CI, 1.27-1.52) (benchmark the median for five sub-Saharan African countries, Haiti, Morocco and Pakistan).
MOI/AMI=153 (Major Obstetric Intervention actually performed for Absolute Maternal Indication in the same population in the same period).
• The UON is therefore 15903*1.4%-153=70 cases or 31.4%relative need.
• For urban 3616*1.4%-81=-30 cases or -58.8% relative need.
• For rural 12287*1.4%-72=100 cases or 58.1% relative need.
Around 70 births which need major obstetric intervention in the study area during the study period did not receive it.
A negative deficit implies that more major obstetric interventions for absolute maternal indications were actually performed than the expected need.
The possibility of some women on admission to hospital giving a temporary address (near hospital) instead of the real address of residence could not be ruled out. Such situation could give rise to overstatement of the number of such women (who gave a temporary address “in town” instead of their real address), thus the negative deficits observed in the urban area.
This study revealed a substantial deficit in the use of emergency obstetric services. However, it was the rural population that suffered the entire deficit, which was 58.1% implying that 72 out of 172 women who had expected MOI for AMI needs.
The finding showed that the rate of major obstetric intervention for absolute maternal indications in the selected woreda was 0.7. This is below the reference rate of 1.4% used in this study. This indicated that there were unmet obstetric needs. To appreciate the significance of these figures, the deficits in absolute terms meant that 70 (31.4%) out of 223 who were expected to benefit from an intervention did not get it.
This finding was consistent with other unmet obstetric need studies conducted in other low-income countries. Figures for Benin, Burkina Faso, Mali and Niger ranged from 0.8% to 1.4% in urban areas and 0.15% to 0.9% in rural areas.
Caesarean sections were the most prevalent interventions (98.6%). This finding is in line with results of six other UON studies, where the proportion of CSs ranged from 73% (Burkina Faso) to 98% in Pakistan. The proportion of hysterectomy for repair of uterus (1.1%) was very low in this area compared with other UON studies in Africa (Benin 10%, Burkina Faso 19%, Mali 8.2% and Niger 12%). This difference might be due to better ANC follow up in this area to identify problems.
The majority of mothers with illness during the current pregnancy had preeclampsia (6.1%) and HIV (2.5%). This is consistent with the findings of a study in rural Ethiopia conducted at Dawro zone Tarcha hospital (5.7%) and (4.5%). Preeclampsia has been incriminated among the indirect and direct causes of maternal deaths globally. But the finding of anemia (1.9%) was very low from the finding in Tarcha hospital (60%) this may be due to the difference in geographical location of the two areas.
Among the MOI conducted caesarean section took the largest share (98.6%) giving a C/S rate per 100 births expected 1% which was below the UN range of 5% to 15%. This is comparable with a study in Kenya which was 1.3 (6). It is worth to note that the increased rate of C/S is not directly proportional to the quality of care. And also below the low end estimate.
The second most often intervention carried out is hysterectomy for ruptured uterus 5 cases (1.4%) of all MOIs. This intervention was slightly higher than study conducted in Pakistan accounted for 0.8% and lower than study conducted in Burkina Faso accounted 14.8% of all MOIs. This difference may be due to the awareness of mother to seek care.
The commonest AMI in this study was obstructed labor accounting for 87 (24%) which is one of the five commonest causes of maternal death in the world. About 57.8% the MOI were done for non AMI mainly for foetal distress. The UON study done in Burkina also showed foetal distress to be the commonest non-AMI. The outcomes of the new born stated the majority 96.14% to be alive until discharge while 3.03% were still born and the rest died within 24 hours. The death of a new born within 24 hours may be due to low neonatal resuscitation capacity. The mothers that suffered from complication after delivery accounted for 1.9% whereby majority of the causes were sepsis and hemorrhage. In a study that did a systematic analysis of causes of maternal deaths in different countries situated in Africa, Latin America and Asia found out that hemorrhage was the commonest cause of death in all continents while deaths due to sepsis were common in Africa as compared to the rest of the world.
The deficit of MOI/AMI rate was 0.7% which is lower than the average of ten countries; accounted 22%. In the case of Burkina Faso the urban areas range of deficit was 0%-4% where the figure in the study area was lower. A study done in Morocco set the value between 1% and 2%. This difference may be due to finding in this study was limited to small population. And this study may not be emphasized on setting appropriate reference ratio which is obtained from a recent data or a pilot project.
Strengths
• It has quantified both the met and unmet obstetric needs.
• The hospital was referral hospital and the only one performing major obstetric interventions in the study area.
• The use of the UON approach has been proven valid in other settings.
In this study area, the prevalence of unmet obstetric need was 31.4%. The overall major obstetric intervention for absolute maternal indication rate of 0.9% and a caesarean section rate of 2.3% among all expected births has important unmet obstetric need when the study results are compared with the 5% threshold. The predominant MOI was C/S and obstructed labor was the dominant AMI. There is a considerable discrepancy when the expected and actual MOI for AMI were compared to whether the woman comes from an area classified as rural or urban.
The low level of actual MOI for AMI (0.6%) amongst the rural population points to major unmet obstetric need there. The high proportions of negative outcomes in mothers undergoing a MOI (complications 1.9%) and in new born (perinatal mortality 0.8%) raise concern about the quality of care being provided. The UONs in rural areas indicate that access to lifesaving obstetric care is a challenge for rural women.
Ethical clearance was obtained from Debre Berhan University department of public health. Formal letter of cooperation was written for North Shoa zone health office and from zone to the hospital.
In this study human subjects were not interviewed rather record was reviewed. The selected hospital was free to enroll and withdraw from the study.
The researcher used hospital records which would have individual addresses and names. But these were not taken as part of the study. Subjects involved in data collection and supervision were under close supervision by the researcher.
Not applicable.
Data supporting the conclusions of this article are available by request to Shambel Mengesha. The relevant raw data will be made available to researchers wishing to use them for noncommercial purposes.
The author declare that he have no competing interests.
Not applicable.
SM wrote the research proposal, analyze the data, wrote the paper and interpret the findings as well as prepare the manuscript as well as supervise the data collection and train data collectors.
WN advised the whole work during proposal and thesis preparation and also participated on the preparation of the manuscript. Both read and approved the final manuscript.
The author would like to acknowledge Debre Berhan university for ethical approval and the advisor. All data collectors are acknowledged for their cooperation during data collection.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kebede SM, Mekonnen WN. (2023) Unmet Obstetric Need in Emergency Obstetric Services in Debre Berhan Referral Hospital, North Shoa Zone, Amhara Regional State, Ethiopia, 2021. Reprod Syst Sex Disord. 12:340.
Received: 18-Aug-2022, Manuscript No. RSSD-22-18950; Editor assigned: 22-Aug-2022, Pre QC No. RSSD-22-18950 (PQ); Reviewed: 05-Sep-2022, QC No. RSSD-22-18950; Revised: 13-Jan-2023, Manuscript No. RSSD-22-18950 (R); Published: 20-Jan-2023 , DOI: 10.35248/2161-038X.23.12.347
Copyright: © 2023 Kebede SM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.