Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Case Report - (2020)Volume 10, Issue 3
Introduction: The use of TKA to treat active joint tuberculosis remains controversial and most orthopedic surgeons would advise against it in cases with active tuberculosis (TB). Skeletal tuberculosis is an uncommon infection that accounts for approximately 2% of all musculoskeletal tuberculosis.
Methods: This case reported is of a 36 years old male diagnosed to have knee tuberculosis after suffering with progressive symptomatic arthropathy for 4 years with multiple attempts to detect extrapulmonary TB found negative. He then had a TKA which histopathologically confirmed the through only a positive ZN stain on the synovial tissue. This treatment has led to a reduction in pain, excellent range of motion and no reactivation of TB. He had initially been diagnosed to have pillonodularsynovitis on two biopsies and treatment geared toward the same was not successful in alleviating symptoms.
Results: The good result of intervention in this patient despite the duration of symptoms and the infective cause can be attributed to the biological behavior of Mycobacterium tuberculosis and its reaction to implant as compared to other bacterial infections such as Staphylococcus aureus.
Conclusion: The diagnosis of knee Tuberculosis can be challenging especially in patients with no obvious pulmonary disease and discharging sinuses. ZN staining was able to detect the TB when the microscopy for Acid Fast Bacilli could not. Active TB diagnosed after TKA has been reported in several small series with good outcomes after systemic chemotherapy. The clinical outcomes of TKA in patients diagnosed with TB post-surgery compare favorably with those of non-infected knees.
Tuberculosis; Pillonodularsynovitis; Total Knee Arthroplasty (TKA); Postoperative
In the musculoskeletal system it affects most commonly the spine followed by hips and knees. The knee joint has the least documented cases catering only for 8% of the skeletal manifestations of the infections (Figure 1).
Figure 1. Comparison of musculoskeletal TB numbers vs. other milliary TB.
There are many cases of progressive osteoarthritis that do not yield good results on medical therapies offered, and lead to TKR being offered as the only option towards relief, and TB of the knee is a condition often tested for only from the synovial fluid sampling which in this case repeatedly yielded negative results for both AAFB and ZN staining. A strong chance is there that we are actually missing cases of TB knee due to the lower sensitivity of the sampling methodology. It may be considered to send all tissue samples from TKRs for evaluation of possible tuberculous infection.
A 36 years old male who presented with a history of right knee pains, swelling and progressive stiffness with severe limitation of function was seen at the The Mp Shah Hospital in Nairobi over a 4 year duration. He had been seen elsewhere and diagnosed with pillonodularsynovitis after an open biopsy and arthroscopic biopsy without significant improvement. The initial x- rays did not reveal any significant joint destruction (Figure 2).
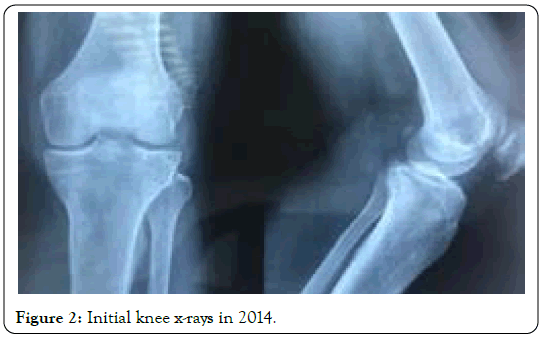
Figure 2. Initial knee x-rays in 2014.
The initial biopsy in 2016 was arthroscopic and the mantoux test then was negative for TB with an ESR of 66 mm. The second biopsy was done open in 2017 and included metaphyseal biopsy of the tibia and revealed pillonodularsynovitis. We repeated an arthroscopic biopsy which revealed pillonodularsynovitis and he was sent for radiotherapy and physiotherapy which on completion he still reported severe pains and limitation of movement.
Due to the progressive limitation of function and severe pains with no signs to suspect active TB in any of the systems or organs both clinically and radiologically, we proceeded plan for a synovial biopsy and total knee replacement. The pre op MRI revealed severe degenerative changes with synovial changes suggestive of pillonodularsynovitis (Figures 3A and 3B).
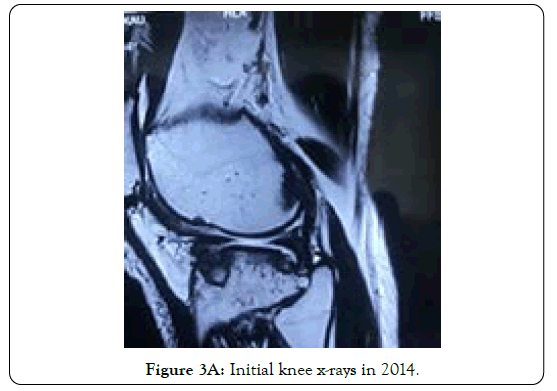
Figure 3A. Initial knee x-rays in 2014.
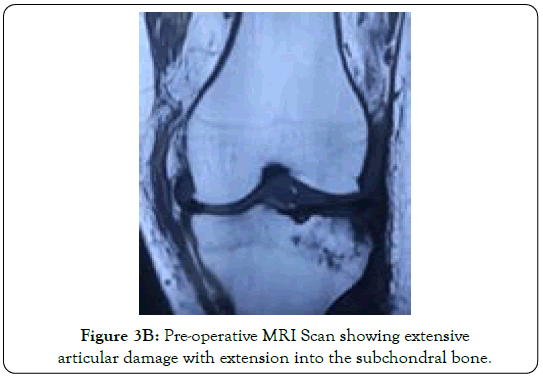
Figure 3B. Pre-operative MRI Scan showing extensive articular damage with extension into the subchondral bone
His Haemoglobin was 14.7 g/dl, total WBC count 7.50 × 109/l, and lymphocyte count of 21.1%. He was seronegative, had a normal uric acid level but the acute and chronic inflammatory markers were normal.
Intra-operatively we found a totally inflamed synovium with nodules and complete damage to the articular surface with multiple punched out lesions (Figure 4). A total synovectomy and biopsy was done and sent for histology. TKA was done using Smith and Nephew cemented knee implant. The biopsy specimens were firm brownish membranous tissue fragments aggregating to 7 cm and weighing 3.6 grams.
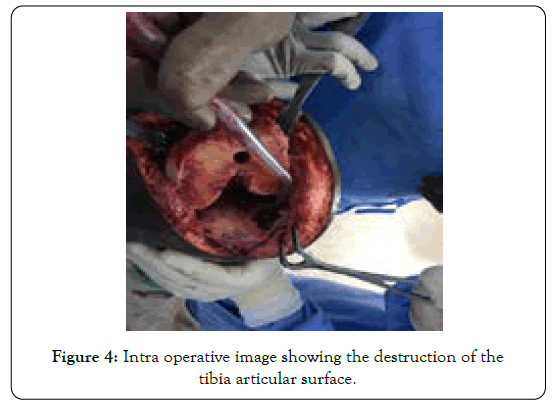
Figure 4. Intra operative image showing the destruction of the tibia articular surface.
The biopsy report was reported as granulomatous synovitis consistent with tuberculosis. Synovium specimen microscopy showed necrosis and granulomas attended with epitheliod cells, lymphocytes, plasma cells and langerhan’s cells. The ZN stains were positive. But AFB and fungal staining came as negative.
Post operatively he was started on 9 months Anti TB chemotherapy including Rifafour (Rifampicin, Isoniazid, Ethambutol and Pyrazinamide) once a day for 2 months for the intensive phase followed by 7 months of treatment of continuous phase with Rifinah (Rifampicin and Isoniazid alone) by the infectious disease specialist. His postoperative check x-rays had a good alignment implant position (Figures 5A and 5B).
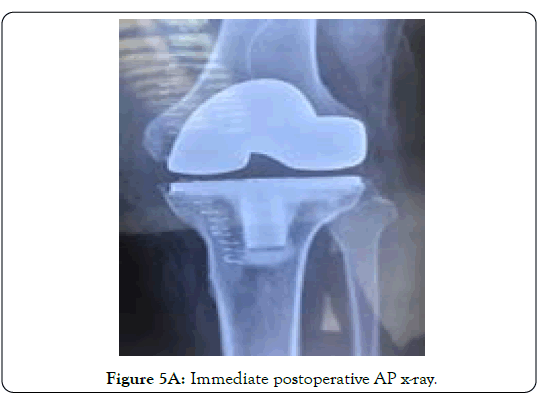
Figure 5A. Immediate postoperative AP x-ray.
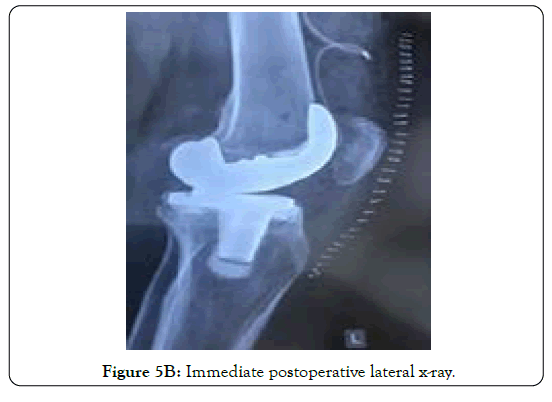
Figure 5B. Immediate postoperative lateral x-ray.
He was mobilized from the second day post-operative with active exercises and discharged on the 5 post-operative day for outpatient follow up.
Patient has been followed up for eight months so far without any reactivation of tuberculosis or implant loosening. The patient had been given Weltek Joint as a supplement to promote healing of the joint, taking one sachet a day. Six months follow up post op x-rays showed good alignment of the implants (Figures 6 and 7). His functional outcome was also good with improvement in range of flexion from 10 degrees pre op to 120 degrees post op and normal quadriceps muscle bulk (Figure 8).
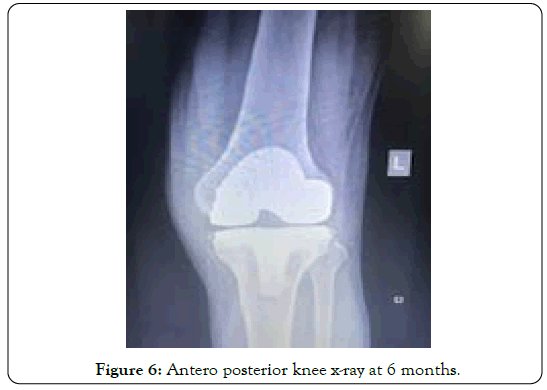
Figure 6. Antero posterior knee x-ray at 6 months.
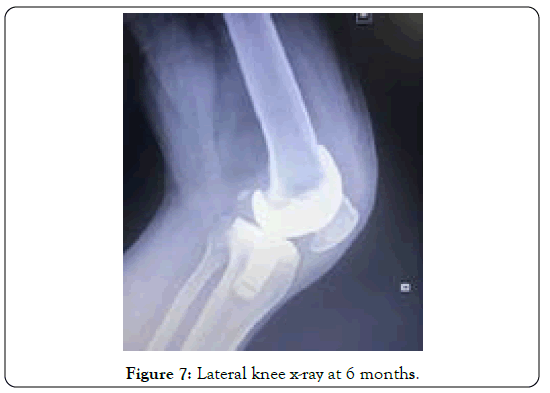
Figure 7. Lateral knee x-ray at 6 months.
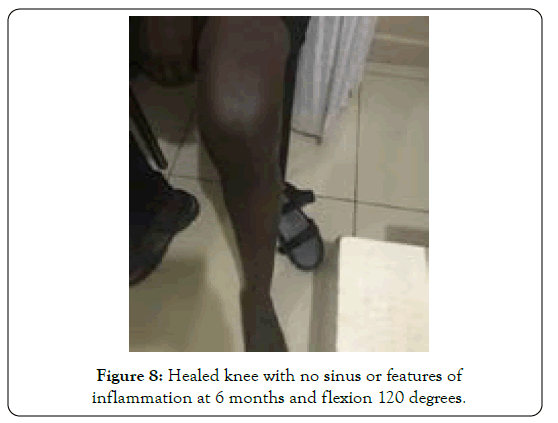
Figure 8. Healed knee with no sinus or features of inflammation at 6 months and flexion 120 degrees.
His liver function was deranged slightly with mild elevation of GGT levels upon completion of the treatment but this resolved insidiously within six months post exposure to the anti-tuberculous drugs.
“This case demonstrates an unusual presentation of extra pulmonary Myobacterium tuberculosis in a young seronegative patient missed on two initial biopsies. The postoperative incidental diagnosis after TKR has allowed us to study the behavior of orthopedic implants in an actively infected joint on treatment for TB. Traditionally the treatment of choice for active TB in a joint includes debridement, arthrodesis and resection arthroplasty along with proper anti TB treatment using regimens for extra-pulmonary infections [1-8].
But debridement will damage the cartilage hence resulting in further pain and reduced range of movement. Arthrodesis gives a pain free joint but with major functional limitation. Resection arthroplasty on the other hand gives a hypermobile painless but unstable joint. Hence today it’s imperative to explore treatment options for joints with active TB that gives the patients a better quality of life. In this case the patient had an ankylosed joint with severe pains that could only be relieved by total joint replacement.
Therefore TKR can be safely done in joints with active TB if the patient is properly treated with anti TB treatment pre operatively and postoperatively with good outcomes compared to the alternatives. Su et al. reviewed 15 patients (16 knees) who had TKR done prospectively and divided into two groups [4]. Group I of 8 knees had active TB and treated pre operatively and post operatively with anti TB regimen. Group II of 8 knees included cases with no active TB hence no anti TB regimen given pre operatively but as they were diagnosed to have TB after surgery they were administered TB drugs post operatively. Group I had one relapse attributed to steroid intake while Group II had four relapses.
Most orthopedic surgeons would be reluctant to treat tuberculosis of the major joints with replacement procedures due to the risk of reactivation. However it is important to note the mycobacterium tuberculosis has specific biologic behavior that distinguishes it from most pyogenic infections and hence its response to implanted materials also differs significantly. Firstly the mycobacterium is known to reproduce slowly while producing minimal adhesion molecules, slime and occasionally becomes dormant.
Secondly TB Bacilli forms a biofilm that differs from other pyogenic organisms and which according to Ha et al. TB bacilli rarely or don’t adhere to the metal surfaces [5]. This in in contrast to a study by Ma et al. that described biofilm formation by M tuberculosis on the surface of cobalt-chromium-molybdenum alloy or titanium alloy [8]. Further to this M tuberculosis is known to divide once in 15-20 hours, which is a much slower rate than Staphylococcus Aureus that divides every 20 min.
The difficulty of diagnosis osteoarticular TB originates from the lack of specific clinical symptoms and timely laboratory tests, which often results in delayed diagnosis [9-14]. The diagnosis of tuberculosis infection after TKA is challenging and after a review by Harwin [12] tuberculosis infection after TKA can be divided into early and late onset. Early-onset infections were classified as those occurring less than eight weeks after surgery as in this case report, while late-onset infections are those occurring more than eight weeks post-surgery. Tokumoto and group [15] have advanced three possible reasons for the delayed diagnosis of tuberculosis infection after TKA: (1) a missed diagnosis of joint tuberculosis infection before TKA, (2) suspected tuberculosis infections are difficult to diagnose, and (3) other, more readily diagnosable bacterial infections that can misdirect clinical management. In addition, the atypical nature of the presentation, and frequent lack of classic definitions of prosthetic joint infections, such as that of the Musculoskeletal Infection Society (MSIS), can result in false negatives [16]. Currently, the gold standard for diagnosis includes a joint fluid or synovial tissue analysis for acid-fast bacilli culture and histo-pathological examination [14, 17-21].
In a study of 23 cases of active TB of the hip joint confirmed histologically and by Polymerase Chain Reaction test with an average follow up of 4.7 years reported no reactivations [2]. All the patients in the study were given three months pre op and 18 months post op TB systemic treatment in conjunction with having undergone a cemented total hip replacement. In another study involving seven cases of active TB septic arthritis of the hip without discharging sinus treated by uncemented THR with thorough debridement and 12 months of post op TB treatment no relapse was recorded at a mean 4.8 year follow up [3].
The management of reactivated infection in a patient with unsuspected TB before arthroplasty as in this case is poorly understood with no clear consensus on treatment [19,21]. If there is reactivation of TB then proper TB regimen with or without debridement alone can save the prosthesis. If the prosthesis cannot be saved then its removal with later revision after use of antibiotic spacers after disease control is advocated. Alternatively removal of implant followed by arthrodesis may be the alternative treatment. So in the post-operative follow up if a patient has signs of infection with bacterial culture showing negative results the surgeons should consider the possibility of TB in the joint.
It is important for physicians to consider TB infection in nonspecific chronic knee pains associated with significant joint destruction in young patients. Total knee replacement can be used in the treatment of active joint TB infection because Mycobacterium tuberculosis divides slowly with no major Metal implants biofilmformation.
To the patient for giving consent for this publication. We acknowledge and appreciate MSN laboratories for funding the cost of this publication.
Citation: Jaffer M, Opondo E (2020) Unusual Presentation of Tuberculous Arthritis Diagnosed After Total Knee Replacement. Rheumatology (Sunnyvale). 10:267. DOI: 10.35248/2161-1149.20.10.267.
Received: 31-Jul-2020 Accepted: 14-Aug-2020 Published: 21-Aug-2020 , DOI: 10.35248/2161-1149.20.10.266
Copyright: © 2020 Jaffer M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.