International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2021)Volume 9, Issue 3
Objective: A patient’s medical insurance coverage plays an essential role in determining the Post-Acute Care (PAC) discharge disposition. The prior authorization process postpones the PAC discharge disposition, increases the inpatient length of stay, and effects patient health. Our study implements predictive analytics for the early prediction of the PAC discharge disposition to reduce the deferments caused by prior authorization, the inpatient length of stay, and inpatient stay expenses.
Methodology: We conducted a group discussion involving 25 Patient Care Facilitators (PCFs) and two Registered Nurses (RNs) and retrieved 1600 patient data records from the initial nursing assessment and discharge notes
Results: The Chi-Squared Automatic Interaction Detector (CHAID) algorithm enabled the early prediction of the PAC discharge disposition, accelerated the prior health insurance process, decreased the inpatient length of stay by an average of 22.22%.The model produced an overall accuracy of 84.16% and an area under the Receiver Operating Characteristic (ROC) curve value of 0.81.
Conclusion: The early prediction of PAC discharge dispositions can reduce authorization process and simultaneously minimize the inpatient the PAC delay caused by the prior health insurance length of stay and related expenses.
Predictive modelling; Prior authorization; Post-acute care; Acute rehabilitation; Skilled nursing facility; Inpatient length of stay; Health insurance
Prior authorization
Almost every diagnostic test or therapeutic intervention that is being ordered by a hospital, except for the most common blood tests and standard radiographs, mandates prior authorization from the patient’s health insurance company [1,2]. Obtaining prior authorization is cumbersome and often involves several steps that delay the procurement of the information needed to make a proper diagnosis and institute ideal treatment. The delay caused due to the prior authorization process not only deters patient safety but also can affect the doctor-patient relationship. The burden of prior, as described by Dr. Neirenberg, might impose a high cognitive workload on clinician’s doctors.
Prior authorization also imposes administrative costs, both on the insurance company and the care providers. Prior authorization forces post-acute care patients and their providers to navigate an additional barrier when seeking access to care a barrier that is perceived to be time-consuming and nontransparent [3]. Some studies have reported the negative impacts of delays caused due to the prior authorization process. Delays due to prior authorization have affected care quality in the clinical specialties such as pain management [4,5] and mental health [6]. Delay due to prior authorization have resulted in increased emergency department visits [5], poor adherence [6-8] and increased medical expenses [4]. Moreover, prior health authorization issues are concomitant with 92% of care deferments, and they contribute to patient harm and administrative ineptitudes [9]. According to the American medical association’s survey that assessed the experiences of a thousand patient care physicians, 64% reported delays for prior authorization decisions from insurers of at least one business day, and 30% stated they wait three to four business days or longer [9]. In addition, 8 out of 10 physicians said the hindrances related to prior health insurance authorization were high, and 86% of these physicians believed that burdens associated with prior authorization have increased over the past five years and led to increases in Medicare spending, PAC obligations and the services provided by insurance companies, including bundled SNF payments [10].
Post-acute care
Post-Acute Care (PAC) is one of the many healthcare services hindered by prior authorization. PAC focus on the improvement of activities of daily living through physical and occupational therapy and health education [11]. For example, patients with cardiac discomfort receive PAC that is tailored to their cardiac events, such as monitoring the cardiac response to therapy, learning self-management of cardiac symptoms, survival management, and cardiac education. PAC has involved multiple providers administering aid in a disconnected manner and poor communication throughout the health care system [12]. When a patient requires PAC services, there is currently little reason given as to why a patient is discharged to a Skilled Nursing Facility (SNF), a home health agency, an Acute Rehabilitation (AR) facility, or a long-term acute care hospital [13]. The demand of PAC has been increasing with an increase in geriatric population. According to the US Census Bureau, by 2050, the geriatric population will increase to 88.5 million [14,15]. Typically, older adults suffer from multiple ailments and chronic conditions [16]. Thus, the geriatric population requires more medical resources and tends to require lengthy hospital stays and PAC assistance to attain desirable health restitution [17,18]. More than one-third of stroke patients in the United States are discharged to PAC facilities, including AR, SNFs, and long-term care facilities [19]. One out of five patients is admitted to PAC after being discharged from the hospital (about 8 million patients annually) [19]. On average, 22.8% of SNF patients end up back in the hospital within 30 days of their discharge [20]. In 2014, patients suffering from neurological diseases comprised 13% of Medicare cases in AR, up from 5% in 2004 [1]. This increase led to an increase in Medicare spending, which grew from $20.3 billion in 2001 to $41.3 billion in 2014 [2].
Delayed PAC can result in poor care, higher readmission rates, and suboptimal patient outcomes [3]. The inpatient stays of patients discharged to PAC are typically lengthier and more expensive than routine discharges [4-8]. The stay length and cost are influenced by the complexity of medical conditions [5] and PAC facility placement delays caused by prior health insurance authorization requirements. The Institute for Healthcare Improvement says that hospital-wide patient flow should deliver the right care, in the right place, at the right time [9]. PAC discharge dispositions require the meticulous coordination of insurance administrators and patients [6]. They are also affected by the availability of required settings, the accessibility of the patient, and pecuniary incentives that might not be allied with medical requirements or cost-effectiveness. A whitepaper from the Institute for Healthcare Improvement suggests working with AR and SNF facilities to improve patient flow through advanced planning, coordination, and partnership development [8]. However, no significant research has been performed to address advanced PAC discharge disposition planning and improved coordination between acute and post-acute services [8].
Role of machine learning
In healthcare, Machine Learning (ML) research has started to have a significant impact on clinicians (e.g., aiding for accurate image interpretation), patients (e.g., assisting processing their own data to better engage), and healthcare system (e.g., improving workflow and reducing medical errors) [2]. The integration of ML into the healthcare system is not only changing the dynamics such as the role of healthcare providers but also creating new potentials to improve patient safety [9], as well as the quality of care [3]. It has assisted clinicians in making better diagnoses [6], improved drug safety [4], and enhanced patient-care monitoring [5-8]. Machine learning enables computers to utilize labeled (supervised learning) or unlabeled data (unsupervised learning) to identify hidden information or make classification about the data without explicit programming [7]. With the increasing amount of data within the healthcare industry, the prevalence of implementing machine learning is gaining momentum [20]. Today in healthcare, a large amount of data is available from Electronic Health Records (EHRs), which contains both structured and unstructured data, and machine learning methods can allow computers to learn from EHR data and develop predictions by identifying hidden patterns.
Given the benefits and potential of ML in healthcare domain, we hypothesis that ML can also assist in predicting PAC services required by patients and thus enable doctors to commence the process of prior authorization in advance. According to research, PAC when provided on time, have improved the physical independence and recovery of patients. In this study, we propose an advanced PAC discharge disposition plan and leverage ML algorithm to address the delay in PAC caused by prior health insurance authorization.
Group discussion and problem identification
To study the PAC discharge disposition procedures and determine the bottlenecks responsible for PAC discharge delays and long inpatient stays, we conducted an online group discussion involving 25 Patient Care Facilitators (PCFs) and two Registered Nurses (RNs). The following three main questions were discussed in this session.
What criteria do we use to determine whether a patient should go to acute rehabilitation?
What criteria do we use to determine whether a patient should go to a skilled nursing facility?
Is there a defined process map that we follow before a patient discharge note is signed by a doctor? (Only to the RNs)
The participant for the group discussion was recruited by Mrs. Shelby (senior nurse and informatics in-charge) and Ms. Vannessa (senior process improvement engineer). The participants were spread across 3 hospitals in Iowa, USA.
Group discussion outcomes
All participating PCFs (n=25) and RNs (n=2) agreed that the PAC discharge type was primarily driven by medical insurance coverage and Physical Therapy (PT) and Occupational Therapy (OT) evaluations of a patient. During PT and OT evaluations, care providers used Braden Scale Scores and Hester Davis Fall Risk Scores to identify high risk patient. They also noted the importance of health conditions, such as a stroke, hip fracture, or spinal cord injury, in mandating AR or SNF service for a patient. Additionally, to qualify for PAC, the patient must be able to tolerate three hours of therapy and must be covered by medical insurance. Figure 1 shows an approximate protocol that PCFs, RNs, and doctors typically follow to manage PAC discharges at our target hospitals. The figure was developed based on information gathered from the group discussion and includes only the crucial steps involved in actual practice that are relevant to this study.
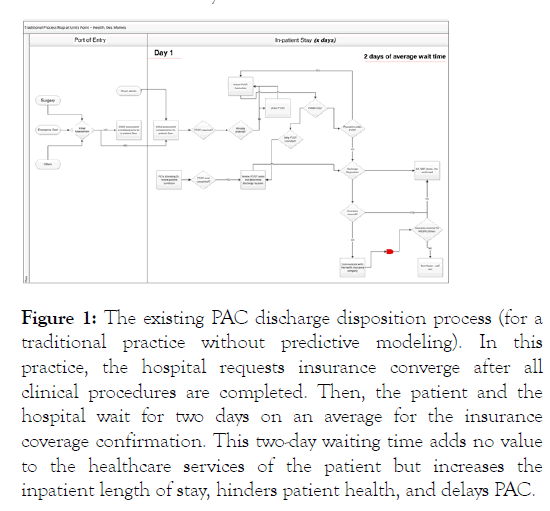
Figure 1: The existing PAC discharge disposition process (for a traditional practice without predictive modeling). In this practice, the hospital requests insurance converge after all clinical procedures are completed. Then, the patient and the hospital wait for two days on an average for the insurance coverage confirmation. This two-day waiting time adds no value to the healthcare services of the patient but increases the inpatient length of stay, hinders patient health, and delays PAC.
After a discharge decision is made and confirmed by both the Post-Acute Care Facilitatory (PCF) and the doctor, the hospital initiates the prior health insurance authorization process; it takes two days on average for the insurance company to confirm whether a patient is insured for AR or SNF, thus postponing the discharge by two days. This process was identified as the bottleneck region responsible for PAC discharge disposition delays and long inpatient stays. To address the bottle neck without changing the clinical workflow and organizational structure, we developed a model to predict the discharge disposition of patients based on patient health data collected during initial nursing assessment. Predicting the discharge location can enable the hospital to commence the prior authorization process in advance.
Data collection and description
We retrieved 1600 patient data records (from July 2018 through August 2018) from discharge and preoperative assessment notes. The data was procured from EHR (EPIC) as shown in Figure 2. The raw anonymized data were used for all analyses contained 629 variables not limited to Hester Davis Fall Risk score, Braden Scale Score, chest pain, history of fracture, history of alcohol abuse, hypertension, history of stroke, and sepsis. Our analysis included only patients discharged to AR or SNF, and missing data and deceased patient data were excluded. For practical reasons, we have categorized the data to the following 14 categories: (a) patient personal information, (b) home setup, (c) PT/OT reasons, (d) Impairment group, (e) history of present illness, (f) medical history, (g) surgical history, (h) family history, (i) allergies, (j) current medication, (k) lab results, (l) vitals, (m) tolerance, and (n) functional deficit (see Supplementary file).
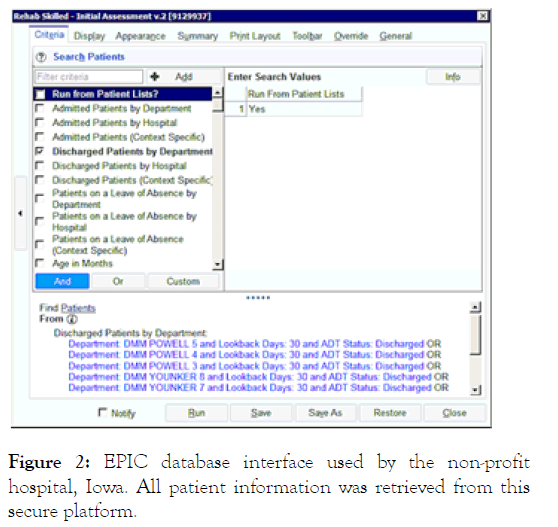
Figure 2: EPIC database interface used by the non-profit hospital, Iowa. All patient information was retrieved from this secure platform.
The Braden Scale was developed by Barbara Braden and Nancy Bergstrom in 1988. It is an important assessment method for identifying patient with risk of pressure ulcers. It involves six different risk factors: sensory perception, skin moisture, activity, mobility, nutrition, and friction and shear and the total scores range from 6-23. A Braden scale score of 9 or less indicates severe patient risk; score between 10 and 12 indicates high risk; moderate risk is denoted by score 13-14; score between 15 and 18 is indicative of mild risk. Hester Davis Scale for fall risk assessment is a nine-factor scale with scores ranging from 0-77. A score of 7-10 indicates low risk to fall, 11-14 indicates moderate risk to fall, and score greater than 15 indicates high fall risk. Hester Davis Scale involves nine factors such as age, date of last known fall, mobility, medications, mental status, toileting needs, volume electrolyte status, communication or sensory function, and behavior. Each factor is a scale item with response categories consisting of increasing levels of risk. The total score obtained from the different indicators (factors) is used to determine if the patient is at risk to fall, and if so, a level of risk is assigned based on the abovementioned scores. Table 1 shows the average Braden scale score, Hester-Davis fall risk score, and the average age of patients per discharge dispositions. Table 2 shows the descriptive statistics of the data set. Illustrate the data (mean and 95% confidence interval). All data points were also tested for normality using Shapiro-Wilk test. In the Shapiro-Wilk test, the null hypothesis is that the population is normally distributed. So, a p-value greater than alpha 0.05 indicates data normality (null hypothesis cannot be rejected).
| Discharge Disposition | Gender | Age | Risk Assessme nt Scales | ||||
|---|---|---|---|---|---|---|---|
| Male | Female | Average (years) | Braden Scale Score | Hester Davis Fall Risk Score | |||
| Another Health Care Institutio n Not Defined | 2 (0.13%) | Missing | 64 | 20 | 7 | ||
| Federal Hospital | 4 (0.26%) | Missing | 68 | 13 | 12 | ||
| Psychiatri c Hospital | 5 (0.33%) | Missing | 49 | 15 | 9 | ||
| Rehab | 24 | 14 | 66 | 17 | 11 | ||
| Facility | (1.58%) | (0.92%) | |||||
| Shortterm General Hospital for Inpatient Care | 4 (0.26%) | 2 (0.13%) | 59 | 17 | 9 | ||
| Skilled Nursing Facility | 76 (5.01%) | 114 (7.52%) | 76 | 16 | 12 | ||
| Swing Bed | 1 (0.06%) | 1 (0.06%) | 92 | 15 | 15 | ||
| Intermedi ate Care Facility | 12 (0.79%) | 17(1.12%) | 73 | 15 | 14 | ||
| Home Health | 75 (4.95%) | 45 (2.97%) | 65 | 18 | 9 | ||
| Care Service | |||||||
| Longterm Care | Missing | 3 (0.19%) | 79 | 15 | 12 | ||
| Expired | 13 (0.85%) | 8 (0.52%) | N/A | N/A | N/A | ||
| Home or Self Care | 499(32.93 %) | 552 (36.43%) | 57 | 20 | 7 | ||
| Hospice | 7 (0.46%) | 5 (0.33%) | 72 | 18 | 14 | ||
| Hospice Medical Facility | 11 (0.72%) | 6 (0.39%) | 79 | 16 | 13 | ||
| Left Against Medical Advice | 10 (0.66%) | 3 (0.19%) | 51 | 19 | 7 | ||
| Court/La w Enforcem ent | 1 (0.06%) | Missing | 40 | 15 | 26 | ||
Table 1: Discharge disposition, patient demographics and average risk assessment scores.
| Predictor | Age (years) | Braden Score Scale | Hester-Davis Fall Risk Score | |
|---|---|---|---|---|
| Min | 16 | 1 | 3 | |
| Max | 97 | 26 | 23 | |
| Range | 81 | 25 | 20 | |
| Mean | 71.9 | 12.44 | 15.52 | |
| Mean Error Std | 1.37 | 0.42 | 0.37 | |
| Std. Deviation | 15.56 | 4.83 | 4.18 | |
| Variance | 242.16 | 23.39 | 17.52 | |
| Skewness | -1.3 | 0.15 | -1.01 | |
| Skewness Error Std | 0.21 | 0.21 | 0.21 | |
| Kurtosis | 2.51 | -0.16 | 1.21 | |
| Kurtosis Error Std | 0.42 | 0.42 | 0.42 | |
Table 2: Descriptive statistics.
Model selection
We used SPSS Modeler and implemented the following five machine learning algorithms: (a) Linear Discriminant Analysis (LDA), (b) the Chi-Squared Automatic Interaction Detector (CHAID), (c) a Random Tree (RT) method (d) a Linear Support Vector Machine (LSVM), and (e) a Classification and Regression Tree (CART). The model that provided the best fit was chosen based on the following three performance measures: (a) overall accuracy and (b) area under the ROC curve (AUC-ROC).
Normality test
Illustrates the QQ-plot for patient age and risk assessment scales. The patient age in AR facility failed to pass the normality test (shaded in red). We compared the risk assessment scores and pat- ient age between SNF and AR.The non-normal data werecompare Mann-Whitney test and data that were normally distributed were compared using two tailed t test. shows the statistic differences between the two PAC facility. We observed significant difference in patient age (p-value <0.00) and fall risk (p-value <0.00) between the two facilities.
Comparative analysis of predictive models
The CHAID algorithm, with the highest overall accuracy of 84.16% and a ROC value of 0.81, was selected as the best fit model.
Proposed process map with CHAID predictive model
The process map after implementing CHAID. The CHAID model identified eligible AR and SNF patients during the initial nursing assessment, thereby allowed the hospital to initiate the prior health insurance authorization process on the first day of an inpatient stay (rather than at the end of the inpatient stay). Early commencement of prior authorization reduced the average length of an inpatient stay from x days to x-2 days (22.22% decreases). The proposed model and workflow do not interfere with clinical processes or replace physician decisions. PT/OT evaluation, initial and continued nursing assessment, and all other essential clinical activities can be processed while the medical insurance company confirms the patient’s insurance coverage, and the patient will not have to wait an extra two days to obtain health insurance authorization after the doctor recommends the discharge location. The model is designed to encourage and enable advanced PAC discharge disposition planning by proactively gauging medical insurance coverage in parallel with the inpatient stay. The new process map ensures the recursive training of the CHAID model, which enhances its reliability and robustness over time and provides a support system for all medical experts
This is the first study that integrates a prediction model into an existing clinical workflow and proposes process map that can assist clinicians to determine patient’s PAC needs based on their initial nursing assessment. Moreover, for patient identified as a candidate for PAC without insurance can be provided with alternate care recommendation. Predicting PAC discharge disposition does not ensure timely prior authorization. The prior authorization process, mainly a product by commercial insurance payers, adds significant delay in a treatment process, which is directly harmful in many health care scenarios. Our study does not address the delays in the prior authorization process, but it allows the providers to comment prior authorization in advance. Additionally, national projections suggest that hospitals may be overcrowded with patients affected with coronavirus (COVID-19) in the coming months. Appropriately, much attention has addressed the acute challenges in caring for this surge of critically ill patients. However, not much has been done to manage PAC services and related prior authorization. Many patients with COVID-19 will require post-acute care to recover from their infection [20]. Our model and workflow may assist in identifying patient’s PAC requirement and thus help in managing PAC services. This will also facilitate faster patient transfer and help in vacating up hospital beds for severely ill patients. Currently, 6-Clicks, which were developed by the Cleveland Clinic Health System , is an effective and user-friendly tool for assisting in PAC discharge disposition planning. The 6-Clicks tool, also known as AM-PAC, is a corroborative tool based on the activity domain of the World Health Organization’s International Classification of Functioning, Disability, and Health (ICF), however, it does not focus on advanced PAC discharge disposition planning.
Our study is the first that implements predictive modeling to determine the PAC discharge type in advance. CHAID is the best fit model, with an overall accuracy of 84.16%. This model has the potential to reduce the inpatient length of stay by 22.22% by encouraging advanced PAC discharge disposition planning, as suggested by the Institute for Healthcare Improvement.
Findings
Healthcare providers and patients are expected to experience lengthy waits before their prior health insurance authorization applications are sanctioned. Seventy-eight percent of providers stated that long prior health insurance authorization processes are associated with patients stopping their treatments. Lengthy inpatient wait times contribute to increased healthcare expenses and poor health outcomes.
Our contributions
This study is the first that implements advanced planning for PAC discharge types to minimize the inpatient length of stay based on predictive analytics.
The CHAID algorithm is implemented and yields an accuracy of 84.16%.
The study uses real data in the analyses.
The PAC discharge time is reduced by 22.22%.
AC conceived and designed the study, participated in data collection, analysis, and interpretation, drafted and revised the manuscript, and approved the final version for submission. AC participated in data collection (literature review), analysis and data interpretation, drafted and revised the manuscript, and approved the final version for submission.
This research received no specific grant from any funding agency in public, commercial, or not-for-profit sectors.
The authors declare they have no conflict of interest in this study.
This study does not involve patient participation, and no personal patient information has been revealed. All analysis and patient data were anonymized for legal and ethical purposes. The study did not seek for IRB approval since the group discussion was a part of routine monthly activity where the analytics team and the care providers meet to discuss systemic problems and develop possible solutions. No patients were involved in this study. All data used were collected retrospectively.
Citation: Choudhury A (2021) Using Machine Learning to Predict Post-Acute Care and Minimize Delays Caused by Prior. Int J Phys Med Rehabil. 9:597.
Received: 09-Mar-2021 Accepted: 23-Mar-2021 Published: 30-Mar-2021 , DOI: 10.35248/2329-9096.21.9.597
Copyright: © 2021 Choudhury A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.