Autism-Open Access
Open Access
ISSN: 2165-7890
ISSN: 2165-7890
Research Article - (2024)Volume 14, Issue 4
Objective: The purpose of this case report is to highlight the successful treatment of a patient with Coloboma, Heart defect, Atresia choanae, Retarded growth and development, Genital hypoplasia, Ear anomalies/deafness, (CHARGE syndrome) using a Vagal Nerve Stimulator (VNS).
Background: This is the first documented case report, to the authors' best knowledge, for a patient with CHARGE syndrome, epilepsy, autism and Postural Orthostatic Tachycardia Syndrome (POTS) that was successfully treated with an implanted VNS therapeutic device.
Case presentation: A 25-year-old young lady diagnosed with CHARGE syndrome, drug-resistant epilepsy and Postural Orthostatic Tachycardia Syndrome (POTS) underwent successful treatment with a Vagal Nerve Stimulator (VNS) implantation. Prior to VNS implantation, patient experienced one to two tonic-clonic seizures a year, partial seizures weekly and daily POTS-related symptoms. Patient was having frequent lightheadedness and syncope spells due to a rapid heart rate and low blood pressure. POTS-related events severely impacted her quality of life. The VNS device was programmed to detect and send appropriate stimulation anytime the heart rate exceeded 20% of the patient’s normal baseline. Data from the VNS device revealed frequent stimulation was triggered, mostly during daytime activities due to elevated heart rate. Over the subsequent two years’ post-implantation, her seizures and POTS-related events were controlled effectively. Following the VNS implantation, the patient became more active, alert and communicative. Patient was able to verbally say words and was unable prior. Improvements in the patient’s disposition are believed to be secondary to parasympathetic stimulation, adequate heart rate control, in addition to behavioral changes and other benefits via her implanted VNS.
Conclusion: VNS showed positive results in improving the patient's quality of life and managing her diverse symptoms, including dysautonomia, POTs, cognitive functioning as well seizure control.
Cognitive functioning; Vagus nerve; Coloboma; Heart defect; Atresia choanae; Retarded growth; Genital hypoplasia; Ear anomalies
Vagal Nerve Stimulation (VNS) therapy involves surgically implanting an electric stimulation device under the skin in the left chest [1]. A wire under the skin connects the device to the left vagus nerve. When VNS is activated, electrical signals are sent along the left vagus nerve to the brainstem, impacting the brain.
Following implantation, physicians can customize the device to suit each patient's specific needs [2]. Both the Food and Drug Administration (FDA) and various studies have cited VNS as a safe treatment for pharmaco-refractory epilepsy in non-surgical candidates over the past two decades [3]. Additionally, VNS has emerged as a therapeutic option for treatment-resistant depression in the field of psychiatry [4]. While VNS has shown efficacy in treating and aiding recovery in various cardiac disorders, its use for orthostatic-related neurocardiogenic dysfunction is a relatively recent area of exploration [5].
Postural Orthostatic Tachycardia Syndrome (POTS) is characterized by a heart rate increase of over 30 beats per min upon standing or during a head-up tilt within 10 min, without orthostatic hypotension. Symptoms include prolonged dizziness, anxiety, brain fog, incongruous tachycardia with no discernible cardiac cause and in some cases, syncope [6].
CHARGE syndrome is a multi-system genetic disorder commonly associated with several cranial nerve anomalies [7]. The acronym CHARGE stands for Coloboma, Heart disease, Atresia of the choanae, Retardation of growth and development, Genital anomalies and Ear malformations with hearing loss, with mutations typically found in the CHD7 gene [8]. The diagnosis of CHARGE syndrome is a clinical one that encompasses a broad phenotype. Unique features, such as coloboma, choanal atresia, atypical semicircular canals and multiple cranial nerve anomalies are common in CHARGE syndrome [9,10]. Features like hearing and/or vision loss, heart malformations and gastrointestinal complications are linked to mutations at the 8q12 site on the CHD7 gene [11]. Research has established links between congenital cardiac defects and subsequent heart rhythm abnormalities due to compromised cardiac structure affecting heart electrophysiology [12]. The pathophysiology of POTS has multiple underlying etiologies which are still under discussion. The treatment modalities are also multifaceted and are best targeted to fit the needs of individual patients [13].
Given VNS's demonstrated efficacy in treating epilepsy, refractory depression and cardiac disorders, this article aims to contribute to the literature on VNS treatment modalities. It presents the first documented case report of a patient with POTS, CHARGE syndrome, drug-resistant epilepsy who clinically improved with daily function, physical activities as well as cognitive function when treated with implanted VNS therapeutic device.
This case involved a 25-year-old female patient diagnosed with CHARGE syndrome, Postural Orthostatic Tachycardia Syndrome (POTS) and treatment-resistant epilepsy. Previous Electroencephalograms (EEGs) revealed abnormalities, including generalized slowing consistent with mild encephalopathy, along with evidence of frontal epileptiform discharges indicative of focal onset seizures. Due to her medication-resistant epilepsy and ineligibility for surgery, patient was considered a candidate for Vagal Nerve Stimulation (VNS) implantation, approved by the FDA. POTS was diagnosed by cardiology following a family request for testing. Despite lifestyle modifications and medication, her POTS symptoms persisted, including fatigue, dizziness and poor circulation in her feet, leading to cognitive decline and reduced exercise tolerance.
VNS implantation was completed in April 2022 and the therapeutic dose of VNS stimulation, set at 1.5 mA, was reached by June 2023. The VNS settings included automatic additional stimulation when detecting a heart rate 20% above the patient’s baseline.
Significant improvement was observed following VNS implantation, noted within 3-6 months’ post-implantation. According to her family, the patient became more alert, less fatigued and more socially engaged since receiving the device. The patient demonstrated remarkable progress, transitioning from being wheelchair-bound to taking a few steps independently and her speech and communication also improved. Figure 1, demonstrates the number of VNS auto stimulation triggers by elevated heart rate (20% above baseline) over the past 2 years. The patient’s physical activity and stamina improved over time. This was also associated with her having fewer episodes of detected elevated heart rate. Notably, in July 23-25 2023, patient even “tolerated a roller coaster ride at Disneyland”, during which her device registered an elevated heart rate without triggering seizures or syncope and patient attended International Charge Conference (ICC) event party and swimming event, as shown in Figure 2. The VNS has allowed her to do more activities during hot summer months without syncopal episodes. As seen in Figure 3, most of the episodes of elevated heart rate were seen during the daytime, consistent with POTs, rather than her seizures, which usually occurred in the evenings. The VNS device significantly improved her quality of life and in the past six months, in 2024, patient has been able to lower the dosage of one of her anti-seizure medications (Figures 1-3).
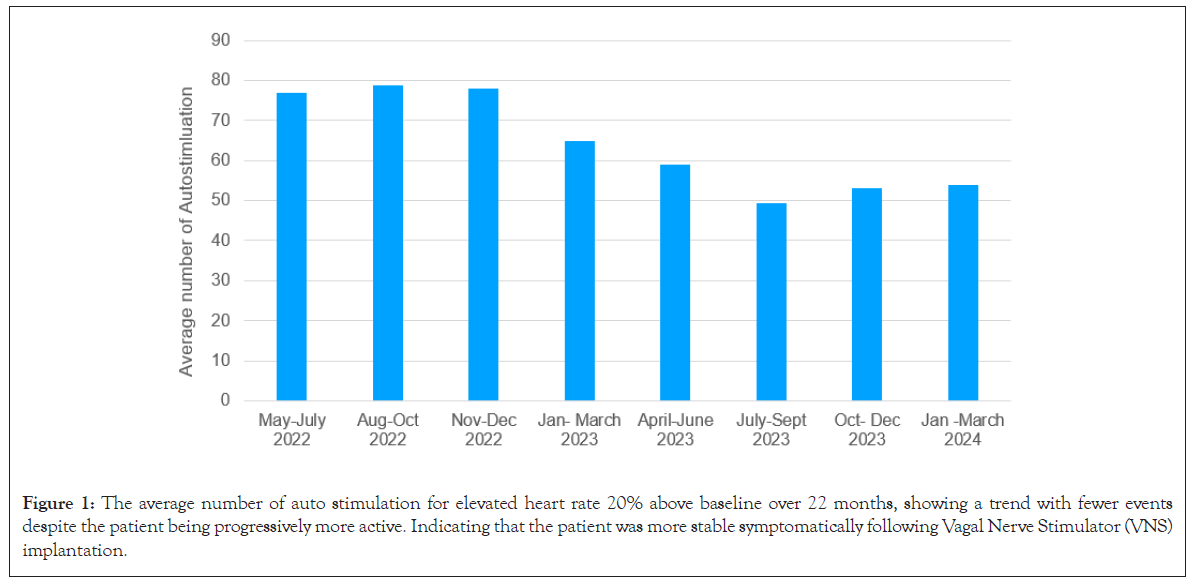
Figure 1: The average number of auto stimulation for elevated heart rate 20% above baseline over 22 months, showing a trend with fewer events despite the patient being progressively more active. Indicating that the patient was more stable symptomatically following Vagal Nerve Stimulator (VNS) implantation.
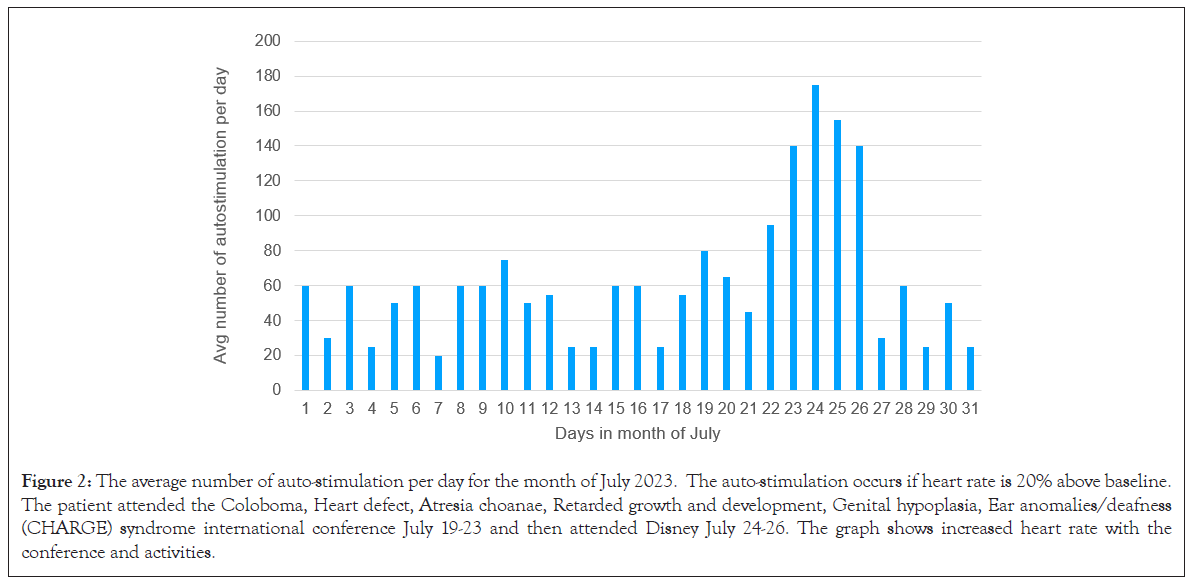
Figure 2: The average number of auto-stimulation per day for the month of July 2023. The auto-stimulation occurs if heart rate is 20% above baseline. The patient attended the Coloboma, Heart defect, Atresia choanae, Retarded growth and development, Genital hypoplasia, Ear anomalies/deafness (CHARGE) syndrome international conference July 19-23 and then attended Disney July 24-26. The graph shows increased heart rate with the conference and activities.
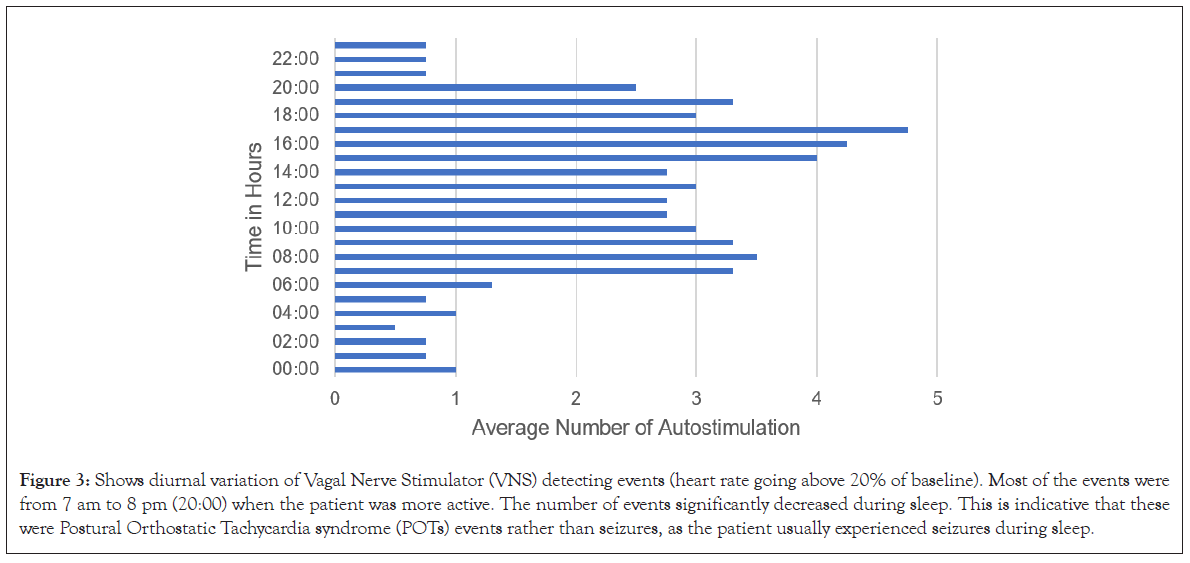
Figure 3: Shows diurnal variation of Vagal Nerve Stimulator (VNS) detecting events (heart rate going above 20% of baseline). Most of the events were from 7 am to 8 pm (20:00) when the patient was more active. The number of events significantly decreased during sleep. This is indicative that these were Postural Orthostatic Tachycardia syndrome (POTs) events rather than seizures, as the patient usually experienced seizures during sleep.
This case report illustrates the clinical improvement of an adult patient with CHARGE syndrome after VNS device implantation and shows effectiveness in treating drug-resistant epilepsy and severe POTS. While the primary diagnosis prompting VNS implantation was drug-resistant epilepsy, however, we found most of the clinical improvement was due to treatment of patient's POTS-related symptoms. POTS in CHARGE syndrome likely is due to underlying abnormalities of the vagal nerve. This patient surpassed her regained previous physical abilities, exhibiting improvement in communication, mobility and participation in various activities such as talking, horseback riding, doing music class, going swimming and other activities.
Individuals with CHARGE syndrome are now surviving and thriving into adulthood due to earlier diagnosis, treatment intervention and enhanced clinical management [14,15]. Resources such as the CHARGE syndrome clinical checklist, that includes a section for older individuals, serves as valuable tool for families and professionals [16]. Additionally, family-run support groups, as mentioned in this case report, provide important source of information. The family, in this case, learned about POTS and its association with CHARGE syndrome from an international conference organized by non-profit organization. At the 2023 International CHARGE syndrome conference in Florida, USA, the family presented their experience alongside senior authors [17]. It was revealed that some individuals with CHARGE syndrome have found some success in managing POTS-related symptoms utilizing lifestyle modifications and external vagal nerve stimulators.
The significance of case reports like these cannot be overstated, particularly considering the scarcity of literature on complex genetic syndromes children transitioning into adulthood. Often, it is the families who must advocate for themselves to education among adult specialists. The two senior authors have developed pamphlets on POTS in CHARGE syndrome for families and professionals, which is now available for download.
POTS is frequently overlooked in individuals with CHARGE syndrome due to their complex physical and multi-organ conditions. However, developments in diagnostic tests have led to increased accuracy in diagnosis and more effective treatment plans. These diagnostic tests and methods include orthostatic blood pressure testing, i.e., bedside lying, standing pulse rate and blood pressure testing alongside trigger documentation. Cranial nerve anomalies affect many if not most individuals with CHARGE syndrome, resulting in facial palsy and auditory, vestibular, olfactory and swallowing disorders [18]. Research regarding vagal nerve dysfunction in CHARGE syndrome is limited. However, a zebrafish model of CHARGE syndrome has been found to have reduced vagal innervation of the gastrointestinal tract and impaired gut motility. This suggests that cranial nerve dysfunction may underlay the autonomic dysfunction seen in CHARGE syndrome [19]. This is supported by the documented severe gut motility abnormality that individuals with CHARGE syndrome experience [20-22].
In the family's own words, 2024 (2 years after VNS implantation)
Before VNS implantation: Patient seemed to be extremely exhausted! Sometimes didn’t want to get out of bed. Author thought patient was having migraines. Patient just seemed to be feeling yucky. Patient is nonverbal so the patient can’t explain how patient was feeling like if patient was experiencing brain fog, etc., but author had to follow patent’s body language. Just walking tired patient out. Patient’s balance seemed off too. Before I knew patient had POTS patient’s heart rate must have been really high when patient was up walking. Author feel bad they didn’t know this! For example, “when we first saw the cardiologist Nurse Practitioner (NP) to confirm POTS, patient took heart rate sitting and it was 90 and then patient had her stand upholding onto a walker and in one min patient’s heart rate jumped to 200! The heat really bothered to patient. Taking a shower too and author didn’t realize hot baths in patient’s whirlpool wasn’t good for patient! Wonder why patient seemed sick after a bath. Even when we were at Disney world which we go a lot, the heat really bothered patient’s and the rides even though patient likes them she would seem more tired and not smiling or happy”.
Following VNS implantation: Patient can “tolerate the rides (At Disney) patient loves like roller coasters and during our last trip patient just seemed happier-smiling and more vocal and not tired”. Author don’t stay the whole day because of the heat. Author go back to our hotel for a pool break and we go back into the park in the evening. We also get to the parks at rope drop (park opening).
Patient has been using “iPad with touch chat and letting us know how patient is feeling which is awesome!! This is huge!!” Patient for example said I feel sick and then she hit the nurse button. She did this a few times. She connected being sick with seeing the nurse. This was so exciting!!
VNS devices and implants may emerge as a potential treatment option for individuals with CHARGE syndrome with resistant form of POTS despite behavioural and medication interventions. Early recognition of POTS symptoms in adolescents and adults with CHARGE syndrome is key to streamline diagnostic processes and providers can provide essential education and management strategies. Further research is needed to determine efficacy and tolerability of external or implanted Vagal Nerve Stimulators (VNS) in individuals with POTs and CHARGE syndrome. Educating adult neurologists and cardiologists can be facilitated by empowering parents and patients to advocate for comprehensive care. The distribution of pamphlets that describe POTS in CHARGE syndrome can also aid in raising awareness and advocating for young adults with CHARGE syndrome.
This research ‘Vagal Nerve Stimulator (VNS) as a Treatment Approach in CHARGE Syndrome: A Case Report’ won Best Presentation award in World Academy of Science, Engineering and Technology in International Journal of Medical and Health Sciences of Volume 18, Issue number 04, 2024.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Vakili R, Elhajjmoussa L, Omidi-Shal B, Blake K (2024). Vagal Nerve Stimulator (VNS) as a Novel Approach in the Treatment of an Adult with CHARGE Syndrome. Autism-Open Access. 14:413
Received: 06-Sep-2024, Manuscript No. AUO-24-33906; Editor assigned: 09-Sep-2024, Pre QC No. AUO-24-33906 (PQ); Reviewed: 23-Sep-2024, QC No. AUO-24-33906; Revised: 30-Sep-2024, Manuscript No. AUO-24-33906 (R); Published: 07-Oct-2024 , DOI: 10.35248/2165-7890.24.14.413
Copyright: © 2024 Vakili R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.