Rheumatology: Current Research
Open Access
ISSN: 2161-1149 (Printed)
ISSN: 2161-1149 (Printed)
Research Article - (2020)Volume 10, Issue 4
Introduction: The diagnosis of synovitis in Rheumatoid Arthritis (RA) can sometimes be very difficult without the use of advanced imaging techniques. A study was conducted to validate a new clinical test (Babur’s Sign), which we believed would help to detect synovitis in the wrist joint.
Objective: To Validate ‘Babur’s Sign’ on clinical examination in the Identification of Wrist Joint Synovitis in Rheumatoid Arthritis (RA) Patients presenting in a tertiary care hospital of Pakistan.
Methods: Using a sample size of 106 RA patients, consisting of 104 females and 2 males, musculoskeletal ultrasound examination as a control, and well-trained rheumatologists with experience in routine ultrasound examinations, a comparison was made between the test and Ultrasound findings. ‘Babur sign’ is when wrist hyperflexion performed by the clinician on the patient, results in immediate shoulder abduction along with elevation of the elbow in patients with active synovitis. First, Babur’s sign would be performed, after which the subject would have an ultrasound examination of the wrist joint done.
Results: We found Babur’s sign to have a sensitivity of 87.84% and a specificity of 78.13%. These findings support the potential application of Babur’s sign in regular clinical practice.
Conclusion: These findings support the potential application of Babur’s sign in regular clinical practice. Implementing this sign into routine examination, may save time for both the patient and doctor, expenses, with the benefit of being non-invasive and most importantly encourage early treatment thus yielding better prognostic outcomes for RA patients
Rheumatoid arthritis; Synovitis, Wrist, Sign, Clinical examination; Ultrasound; Diagnosis
Rheumatoid arthritis (RA) is a chronic inflammatory disease that is notorious for its irreversible destruction of joints, namely the small joints of the hands and feet [1]. It’s a major health concern, given that the prevalence and incidence of RA has been on the rise since 1990 and has affected 0.5-1% of the population globally [2,3].
Being autoimmune in nature, RA has multiple systemic manifestations [4]. The clinical presentations can vary, but most often it is identified as a gradual symmetrical swelling, stiffness and pain in the small joints, along with morning stiffness lasting at least one hour before improving [5]. The diagnosis of RA can be made using clinical examination, laboratory tests, and imaging studies [4]. Laboratory tests include assessment of the levels of C-Reactive Protein (CRP), Erythrocyte Sedimentation Rate (ESR), Rheumatoid Factor, and Anti-cyclic citrullinated peptide (ACCP) [4]. However, it must be kept in mind that all the laboratory parameters have to be combined with history and clinical examination before labeling a patient to have RA, as up to 30% of cases are negative for markers of RA [4]. One of the main symptoms related to the musculoskeletal system is synovitis [6]. In RA the most common areas of clinical synovitis are wrist, metacarpophalangeal joints (MCP joints) and proximal phalangeal joints (PIP joints) in hands [5].
General tests suggesting wrist joint synovitis include the sitting hands test and the windmill test [7]. Many studies have shown imaging techniques, such as MRI and Ultrasound examination to be more sensitive than clinical examinations in the detection of synovitis [6]. The use of ultrasound imaging alongside clinical examination and laboratory data is advantageous, especially as it is deemed as a valid and easily reproducible test to identify synovitis in the joints of the wrist and fingers [1,6].
Clinical studies have indicated that early diagnosis and treatment of synovitis, leads to a better prognosis by decreasing inflammation and limiting the structural changes [6]. ‘Treat to Target’ guidelines were developed by a task force of Rheumatologists, patients and a nursing specialist, with the goal of achieving early remission in RA patients [8]. Remission, however is usually seen in patients with early RA. However, the goal of remission is difficult to achieve in chronic RA patients, so low disease activity in such cases is also deemed as an appropriate alternative [9].
We would like to demonstrate how a simple clinical test ‘Babur’s sign’ could reliably identify synovitis in the wrist joint. This would be advantageous as more patients can be evaluated in busy outpatient departments, given that the time taken to prepare, perform and interpret the ultrasound would be spared. While ultrasound is a valuable investigation, being readily available, relatively cheap, and comfortable for the patient and easy to transport, it does have its pitfalls, such as the physician requiring experience and expertise, having a steep learning curve and a limited field of view [10,11]. Babur’s sign is when wrist hyperflexion performed by the clinician on the patient, results in immediate shoulder abduction along with elevation of the elbow in patients with active synovitis, as seen in Figure 1.
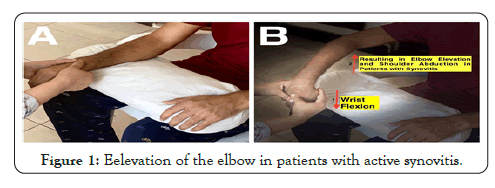
Figure 1: Eelevation of the elbow in patients with active synovitis.
This study was conducted in a tertiary care hospital of Pakistan. We included 106 patients with Rheumatoid Arthritis diagnosed on the basis of 1987 American College of Rheumatology (ACR) Classification criterion. These patients came to the outpatient department between December 2019-January 2020. The selection criteria were such that only RA patients who would come to the OPD for regular follow-ups were included in the study. Meanwhile, RA patients who had the disease for more than one year, clinical or radiologically damaged wrist joints or wrist pain due to any other cause (including trauma, psoriatic arthritis, tenosynovitis and infection) were all excluded from the study.
Once it was established that a patient met the inclusion criteria, the patients signed a document, giving their consent to be included in this study, after which Babur’s sign would be performed on them. As mentioned earlier, Babur’s sign is when wrist hyperflexion performed by the clinician on the patient, results in immediate shoulder abduction along with elevation of the elbow in patients with active synovitis. Regardless of the outcome of Babur’s sign, the patient would then have an ultrasound performed on the wrist joint, which would be interpreted by the two qualified rheumatologists present at the time. Information regarding the patients’ mean age, gender, mean duration of disease, smoking status, and seropositivity markers (RF and ACCP) was also obtained.
After collection of the data, statistical analysis was carried out. The results are as mentioned below in Table 1.
| Babur Sign | +ve | USG | Total | |
| +ve | -ve | |||
| 65 | 7 | 72 | ||
| 87.8% | 21.9% | 67.9% | ||
| -ve | 9 | 25 | 34 | |
| 12.2% | 78.1% | 32.1% | ||
| Total | 74 | 32 | 106 | |
Table 1: Results of Babur’s Sign compared with Ultrasound (USG)examination as a Gold standard.
The study was conducted on a total of 106 patients, with the mean age being 37.32 ( ± 7.50). Given the large female predominance of the disease, this cohort consisted of 104 females and 2 males. The mean duration of the disease was 5.04 years ( ± 0.98), with the majority of patients being non-smokers (95%). With regards to seropositivity, 74 patients (70.0%) patients exhibited a positive Rheumatoid Factor marker was and 67 patients (68%) showed positive Anti-Cyclic Citrullinated Peptide.
Babur’s sign would be considered positive if wrist flexion would result in shoulder abduction and elbow elevation. The sign and ultrasound examination were conducted in all 106 patients. Of these, a total of 72 patients exhibited a positive Babur’s sign (67.9% of subjects).
It was found that 74 patients showed active synovitis on ultrasound examination, of these, 65 of them displayed a positive Babur’s sign (87.8%), while just 9 patients (12.2%) had an ultrasound examination revealing synovitis in conjunction with a negative Babur’s sign. On the contrary, 32 patients displayed no signs of synovitis on ultrasound, 7 of them still yielded a positive Babur’s sign (21.9%). The remaining 25 patients (78.1%) displayed a negative Babur’s sign in the absence of ultrasound findings.
The results of our study therefore conclude that the sensitivity of Babur’s sign is a staggering 87.84%, with a specificity of 78.13%. Positive predictive value stands at 90.28%, and the negative predictive value at 73.53%, with an impressive overall Diagnostic accuracy of 84.91%.
With the rising prevalence of RA, early detection is key in limiting the disease activity and damage. It has been shown, that there was 33% decrease in radiologically evident progression of disease in patients treated earlier than 2 years disease duration with DMARDs in comparison with those treated after [12]. Early diagnosis and treatment may result in not only better prognosis but even remission states [13].
While plain X-rays are a simple, cheap and easily repeatable test, they are not so useful in the early detection of the disease, as they are unable to detect early inflammatory changes [14]. Often, MRI is used as a gold-standard with which Ultrasound examination is compared with [10]. Ultrasound examination is currently regarded as a reliable investigation for the detection of Synovitis in RA. A recent meta-analysis paper revealed the sensitivity and specificity in such cases to be 0.73 (95% CI 0.51, 0.87)/ /0.78 (95% CI 0.46, 0.94), for the wrist joint [6]. We decided to use USG examination as means to compare the reliability of Babur’s sign.
The sensitivity we deduced from our experiment testing Babur’s sign came out to 87.84%, with a specificity of 78.13%. These values lead us to believe that Babur’s sign is reliable in the detection of wrist joint synovitis. The implementation of Babur’s Sign in the routine examination of RA patients may have many benefits, as it is a simple non-invasive test, with no need for training or specific skillsets for interpretation, it does not require the patient to be shifted from one room to another, nor is it time consuming. To our knowledge, this is the first time in Pakistan, that a clinical test is being evaluated in correlation with radiological examination.
In Pakistan, there is a large burden of rheumatic disease, for which there is little provision [14]. There are currently 70 trained rheumatologists in the country, according to the Pakistan Society for Rheumatology, which is considerably low, given the rising prevalence [15,16]. Therefore, having a test that can be conducted swiftly, may allow more patients to be seen on a daily basis, therefore somewhat neutralising the burden.
Our study was limited by the fact that our sample size consisted of only 106 patients, and the vast majority of our subjects were female. In addition to this, it was difficult to follow up on the seven patients who exhibited a positive Babur’s sign, but failed to show ultrasonographic findings, to see if they would later develop characteristic findings of active synovitis.
The use of ultrasound examination has been a ground-breaking revelation in the diagnosis of RA, but it is worth noting that it may not be as easily available in hospitals in rural areas in less developed countries. Furthermore, as mentioned earlier, it has its limitations too, requiring experience and expertise, having a steep learning curve and a limited field of view. Therefore, the implementation of Babur’s sign into regular clinical practice concerning RA patients, may lead to earlier detection and better disease outcomes in patients who do not have access to better equipped hospitals.
None
This study was approved by the Ethical Committee of Fauji Foundation Hospital, Rawalpindi, Pakistan.
The participants all signed a document providing their permission to be included into the study prior to the examination.
The consent for publication was provided in the permission form stated above, which the participants signed prior to the examination.
N/A
N/A
Citation: Salim B, Faisal MJ, Shahid M, Samreen S, Gul H, Nasim A, et al. (2020) Validation of Babur’s sign, a New Clinical Test for the Identificationc of Wrist Joint Synovitis in Rheumatoid Arthritis Patients. Rheumatology (Sunnyvale). 10:268. DOI: 10.35248/2161-1149.20.10.268.
Received: 12-Oct-2020 Accepted: 26-Oct-2020 Published: 02-Nov-2020 , DOI: 10.35248/2161-1149.20.10.268
Copyright: © 2020 Salim B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.