International Journal of Physical Medicine & Rehabilitation
Open Access
ISSN: 2329-9096
ISSN: 2329-9096
Research Article - (2023)Volume 11, Issue 1
Background:The increase in Blood Lactate (BLa) level during incremental exercise testing (Inc-Ex) leads to bicarbonate ion buffering and excretion of carbon dioxide (CO2). The relationship between the excretion of excess CO2 and BLa during Inc-Ex is unclear. This study aimed to verify whether BLa could be estimated from excess CO2 excretion during Inc-Ex.
Methods: We recruited 11 patients (group P, age: 72.6 ± 8.5 years; male: 9) who were prescribed medication for cardiovascular risk factors or diseases. Twenty-two healthy participants (group H, age: 69.3 ± 6.7 years; male: 9) were also recruited for comparison. All participants performed the symptomatic limited cardiopulmonary exercise test, and their BLa levels were measured. Excess CO2 (the difference between oxygen uptake and CO2 excretion) was determined from breath-by-breath gas analysis data. BLa level was measured from arterialized fingertips every minute during Inc-Ex (10 W/min ramp exercise). Plots of per-minute excess CO2 and BLa were linearly regressed, and regression equations and coefficients were calculated along with 95% confidence intervals and prediction intervals.
Results: BLa levels were measured 9.2 ± 2.4 times per participant during Inc-Ex. BLa was significantly correlated with excess CO2 in both groups H and P (all participants: r=0.862, p<0.001, y=0.0139x+1.7364; group H: r=0.872, p<0.001, y=0.0108x+1.617; and group P: r=0.878, p<0.001, y=0.0139x+1.7364).
Conclusion: Excess CO2 aided in verifying BLa levels within a certain range. Excess CO2 during the cardiopulmonary exercise test is useful for estimating BLa levels.
Blood lactate; Incremental exercise; Cardiopulmonary exercise testing; Excess carbon dioxide; Older population; Cardiovascular disease
In cardiac rehabilitation, some countries, including Japan, use Ventilatory Anaerobic Thresholds (VAT) derived from Cardiopulmonary Exercise Testing (CPET) to determine initial training intensity [1,2]. To determine VAT using the cardiopulmonary exercise test, we generally use the V-slope method {oxygen uptake (VO2) Versus Carbon Dioxide Output (V̇CO2) plot} [3]. The energy supply ratio required for an exercise increases the glycolytic metabolism against the aerobic metabolism as the intensity of exercise increases [4,5]. Therefore, the glycolytic pathway is stimulated, lactate production within the exercising muscle increases, and intramuscular lactate translocates into the blood. The Blood Lactate (BLa) level at VAT increases by approximately 0.5 mmol/L above the baseline, and the BLa level continue to rise above VAT [6]. Compared with the other two conventional methods, which entail using the Ventilatory Equivalent (VE/VO2) and end-tidal gas concentrations (end-tidal O2), the V-slope method is more sensitive to excess CO2 (the difference between VO2 and VCO2); therefore, it is presumed that excess CO2 corresponds directly to changes in BLa level [7-9], except for special diseases [3,10,11] (it shows the term "nonmetabolic excess CO2") [12]. Lactic acid almost completely separates into (H+) and (La-) within the physiological pH range [13]. Most of the (H+) in the blood is buffered mainly by bicarbonate ((H+) + (HCO3-) → (H2O) + (CO2) ↑) to maintain body homeostasis [7,14,15]. Therefore, the amount of CO2 exhaled during exercise with lactate accumulation (expired CO2) consists of CO2 produced by metabolism (produced CO2) and excess CO2 excreted (excess CO2). The sum of this excess CO2 excretion is defined as CO2 accumulation, which is considered to reflect the degree of buffering by the bicarbonate system of (H+) that originated from ATP hydrolysis produced by glycolytic metabolism with increased exercise intensity [4,5,12,16]. In contrast, the difference between VCO2 and VO2 (excess CO2) at a certain point of incremental exercise load is considered to reflect the increase in glycolytic metabolism, such as lactate, at the time, although there is a time difference. The predicted BLa increment from excess CO2 and the measured BLa showed a good relationship in healthy men. However, the determination of the slope “a” of the linear function used in this method as the basis for the CO2 accumulation is subjective and lacks objective reproducibility [17].
Previous studies on exercise and the excretion of excess CO2 have had several limitations. First, due to the measurement of BLa by venous blood collection, the values obtained were low compared with that of arterialized blood which is utilized by tissues throughout the body, and the proportion produced by the motor muscles was unknown [12,18,19]. Second, the frequency of blood collection was low; hence, detailed changes were unknown [16,20]. Third, since the study was conducted on healthy men, the appropriateness of applying the results to older adults or those with diseases is equivocal [7,21]. Furthermore, the trend is unclear because of the comparison of pre- and post-BLa samples [17,22].
In summary, although comparisons have been made between excess CO2 (CO2 excess or CO2 accumulation) and BLa increments, the relationship between excess CO2 and BLa at a certain point in Incremental Exercise (Inc-Ex) has not been examined. In addition, it is unclear whether BLa is associated with excess CO2 excretion (excess CO2) during exercise in healthy older adults and patients with cardiovascular risk, who constitute the majority of the population requiring exercise therapy. Therefore, this study aimed to confirm the association between excess CO2 and BLa during Inc-Ex testing. Revealing the relationship between excess CO2 and BLa during Inc-Ex testing makes it simpler to predict BLa trends without requiring invasive BLa measurements. Furthermore, since BLa trends improve with exercise training, we believe that excess CO2 evaluation during exercise testing can help to assess the effects of exercise training [23-25].
Participants
The study required that all participants were aged between 60 and 80 years. We recruited 11 patients who were under medication for cardiovascular diseases (n=5) or cardiovascular risk factors (n=6) (group P, age: 72.6 ± 8.5 years; male: 9). Cardiovascular disease etiologies included post-coronary artery bypass graft surgery for coronary artery disease (n=2), myocardial infarction (n=1), and valvar heart disease (n=2). The cardiovascular risk factors included hypertension (n=11), impaired glucose tolerance or diabetes mellitus (n=2), and hyperlipidemia (n=8). Twenty-two healthy participants matched for age (group H, age: 69.3 ± 6.7 years; male: 9) were recruited for comparison (Table 1).
| Characteristics | Healthy group (H: n=22) | Patient group (P: n=11) | |
|---|---|---|---|
| Age (years) | 69.6 ± 6.6 | 72.6 ± 8.5 | |
| Sex | M:9, F:13 | M:9, F:2 | |
| Height (cm) | 158.5 ± 6.4 | 164.8 ± 3.6 | |
| Body weight (kg) | 56.0 ± 8.4 | 66.1 ± 10.5 | |
| BMI | 22.2 ± 2.1 | 24.4 ± 4.1 | |
| CTR (%) | 0 | 48.6 ± 4.3 | |
| BNP (pg・dL-1) | 0 | 79.8 ± 131.6 | |
| LVEF (%) | 0 | 68.3 ± 14.1 | |
| Comorbidity | |||
| Hypertension (n (%)) | 0(0) | 11(100) | |
| Dyslipidemia (n (%)) | 0(0) | 8(73) | |
| Impaired glucose tolerance (n (%)) | 0(0) | 2(18) | |
| Obesity (n (%)) | 2(9) | 4(36) | |
Note: Data are presented as mean ± SD, and obesity was defined as BMI >25 kg・m2. No significant differences in clinical characteristics, such as age and BMI, were observed between groups H and P. CTR, cardiothoracic ratio; BMI, body mass index; BNP, brain natriuretic peptide; LVEF, left ventricular ejection fraction.
Table 1: Data of participants' clinical characteristics.
Exclusion criteria included change in medication within 6 months, infection within 2 weeks, body temperature >37.5˚C, chronic atrial fibrillation or flutter, permanent pacemaker, and the presence of orthopedic conditions rendering the individual unfit for exercise testing. In addition, we excluded participants taking warfarin or other anticoagulants and metformin for diabetes. The cases and measurement records for this study were collected from participants in our previous study (https:// pubmed.ncbi.nlm.nih.gov/34678888/). We did not use the cases that could not perform the second measurement in that study, but we included them in this study.
Exercise testing
Cardiopulmonary exercise testing was performed using a stationary bicycle (Strength Ergo 8; Mitsubishi Electric Engineering, Tokyo, Japan) and a breath-by-breath gas analyzer (AE-300S; Minato Ikagaku Co., Tokyo, Japan). Symptomatic maximal exercise was performed using a ramp protocol of 10 W/min (Inc-Ex). Warm-up exercises were performed for 2 minutes at 10 W. We used 10-s average data for all analyses. The output was obtained using a gas analyzer system.
VAT determination
We determined the VAT during Inc-Ex testing. VAT was visually determined using the modified V-slope method described by Sue et al. [26], a modification of the method described by Beaver et al. [27]. The details of this method have been published [28,29]. In summary, this V-slope method involves drawing a line through the data points parallel to the respiratory exchange ratio (RER)=1 diagonal, which is referred to as the pre-VAT baseline. The point at which the data begin to deflect towards the left is selected as the VAT. The data points preceding the parallel line were disregarded. A line drawn parallel to the RER=1 diagonal signifies a change of 1.0 in the rate of ΔV̇CO2/ΔV̇O2. Therefore, the point at which this index begins to increase above 1.0 is the VAT deflection point [28,29]. We used this approach to identify the VAT in this study.
BLa measurement
Blood was sampled using a finger stick. A topical vasodilator (Finalgon cream, nonivamide butoxyethyl; Boehringer Ingelheim, Gaithersburg, MD, USA) was applied to three fingers of the left hand (2nd, 3rd, and 4th). The cream was removed after 10 minutes, and the entire left hand, including the distal part of the forearm, was placed in a water bath (at 43˚C-45˚C) for 10 minutes [6,30]. The BLa levels were determined using Lactate Pro LT-1730 (Arkray, Kyoto, Japan). The instrument was calibrated using a calibration strip before each exercise session. Blood samples were collected every minute during the ramp exercise.
Excess CO2 and BLa and correction of rightward shift
The difference between VO2 and VCO2 per minute (excess CO2; mL/min) was determined from the VO2, and VCO2 values obtained from the exhaled gas analysis matched to the time of the BLa measurement. In addition, we attempted to correct excess CO2. The buffering of CO2 induced by exercise appeared to be a rightward shift (RtShift) in the V-slope method. To correct for excess CO2, we used a mathematical method to exclude differences in individual buffering capacity. The amount of RtShift was mathematically determined by regressing the individual V-slope graphs (moving average of eight breath-bybreath data) with a quadratic function and calculating an approximate equation to find a tangent line parallel to R=1 [29]. The difference between VO2 and VCO2 was calculated, and the individual RtShift values were subtracted to obtain the corrected excess CO2 (mL/min) (Figure 1).
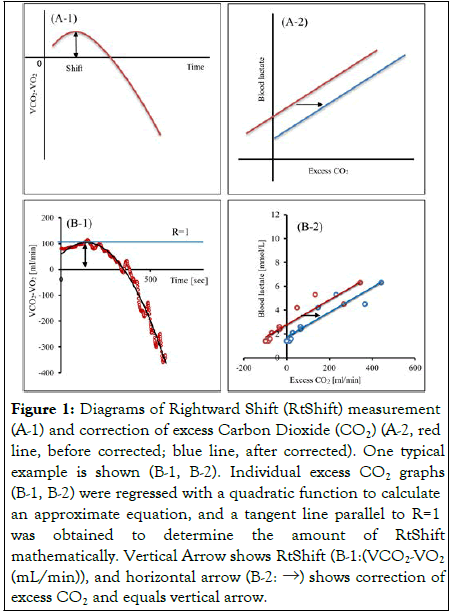
Figure 1:Diagrams of Rightward Shift (RtShift) measurement
(A-1) and correction of excess Carbon Dioxide (CO2) (A-2, red
line, before corrected; blue line, after corrected). One typical
example is shown (B-1, B-2). Individual excess CO2 graphs
(B-1, B-2) were regressed with a quadratic function to calculate
an approximate equation, and a tangent line parallel to R=1
was obtained to determine the amount of RtShift
mathematically. Vertical Arrow shows RtShift (B-1:(VCO2-VO2 (mL/min)), and horizontal arrow (B-2: →) shows correction of
excess CO2 and equals vertical arrow.
CO2 accumulation and BLa
With the time of VAT as zero, the difference between V̇CO2 and V̇O2 from VAT to peak was integrated with the values of V̇O2 and V̇CO2 per 10 s obtained from the exhaled gas analysis [16]. ΔBLa was determined as the difference in BLa levels from VAT to peak. We plotted ΔBLa and CO2 accumulation and calculated the relationship.
Statistical analysis
Data were presented as mean ± Standard Deviation (SD). Unpaired data were analyzed using Student's t-test. Paired data were analyzed using paired t-test. Plots of the per-minute excess CO2 and BLa and plots of CO2 accumulation and ΔBLa were linearly regressed, and regression equations and coefficients were calculated. The 95% confidence intervals were also calculated to determine the relationship between excess CO2 and BLa.
Statistical analyses were performed with Statistics for Excel 2012 (Social Survey Research Information Co., Tokyo, Japan).
The clinical characteristics of the participants are summarized in Table 1. Group P had a higher proportion of men with a significantly higher mean height and weight than group H.
BLa level
The mean BLa levels at rest and during warm-up were not significantly different {rest: 1.15±0.32 (H) and 1.35±0.29 mmol/ L (P), warming up: 1.26±0.28 (H) and 1.42±0.33 mmol/L (P)}. BLa levels were measured 9.2±2.4 times per participant during Inc-Ex (group H: 9.3±2.6 times vs. group P: 9.0±2.2 times, p=0.775) and for a total of 295 times.
Correlation between excess CO2 and BLa
BLa was significantly correlated with excess CO2 in both H and P groups (all participants: r=0.881, p<0.001, y=0.0104x+2.6316; group H: r=0.862, p<0.001, y=0.0101x+2.5666; and group P: r=0.913, p<0.001, y=0.011x+2.7819) as shown in Figure 2.
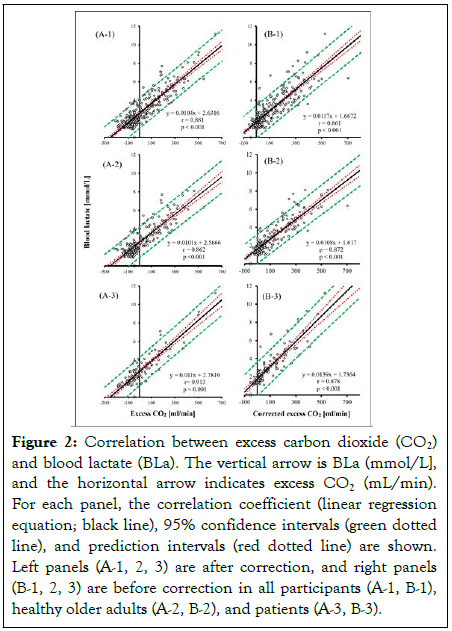
Figure 2: Correlation between excess carbon dioxide (CO2)
and blood lactate (BLa). The vertical arrow is BLa (mmol/L],
and the horizontal arrow indicates excess CO2 (mL/min).
For each panel, the correlation coefficient (linear regression
equation; black line), 95% confidence intervals (green dotted
line), and prediction intervals (red dotted line) are shown.
Left panels (A-1, 2, 3) are after correction, and right panels
(B-1, 2, 3) are before correction in all participants (A-1, B-1),
healthy older adults (A-2, B-2), and patients (A-3, B-3).
Correlation between CO2 accumulation and BLa
ΔBLa was significantly correlated with CO2 accumulation in both H and P groups (all participants: r=0.786, p<0.001, y=0.0005x+1.3213; group H: r=0.793, p<0.001, y=0.0005x +1.2701; and group P: r=0.841, p=0.001, y=0.0006x+1.321) as shown in Figure 3.
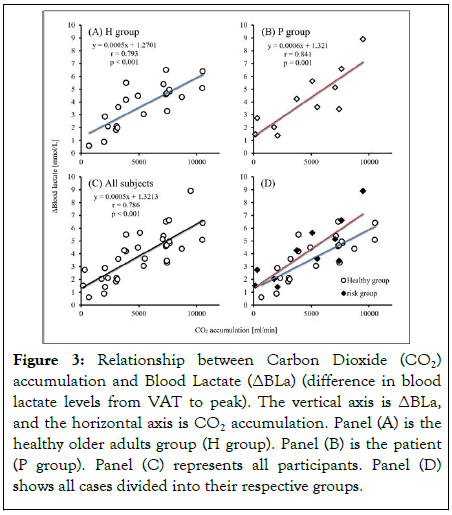
Figure 3: Relationship between Carbon Dioxide (CO2) accumulation and Blood Lactate (ΔBLa) (difference in blood lactate levels from VAT to peak). The vertical axis is ΔBLa, and the horizontal axis is CO2 accumulation. Panel (A) is the healthy older adults group (H group). Panel (B) is the patient (P group). Panel (C) represents all participants. Panel (D) shows all cases divided into their respective groups.
To the best of our knowledge, this is one of the few studies to confirm the relationship between BLa levels and excess CO2 during Inc-Ex testing in healthy older adults and patients with cardiovascular disease/risk factors. In this study, the relationship between time-specific differences in V̇O2, V̇CO2, and BLa during Inc-Ex testing was also investigated in addition to the relationship between CO2 accumulation and ΔBLa as in previous studies. To date, these results have not been reported in healthy older adults or patients with cardiovascular risk.
The results of this study indicate a significant relationship between CO2 accumulation and ΔBLa. When comparing the healthy older participants with the at-risk group, the healthy older participants had lower regression coefficients. Based on reports of athletes in previous studies, we speculate that the atrisk group may have been influenced by a lower buffering capacity of the muscle [16]. Several studies on the relationship between BLa level and excess CO2 have reported an association between CO2 accumulation and changes in BLa level in athletes or healthy participants [12,16,18]. These studies reported higher CO2 accumulation in long-distance runners than in shortdistance runners. The ratio of CO2 accumulation to ΔBLa in short-distance runners is lower than that of long-distance runners, and excess CO2 is low for increased BLa [18]. Long-distance runners have less buffering capacity within the muscle than shortdistance runners. This may be related to the increased diffusion of (H+) into the extracellular fluid due to the high capillary density [31,32]. Another study found an association between endurance training and decreased CO2 accumulation in longdistance runners [33]. This suggests that CO2 accumulation may be a useful indicator of higher or improved lactate-buffering capacity.
Both groups showed a strong correlation between excess CO2 and BLa when the participants performed according to the recommended duration of exercise testing, which is commonly used in symptomatic limit CPET. An increase of 100 mL/min in excess CO2 is considered to increase the lactate level by 1 mmol/ L. An increase in excess CO2 would suggest a decrease in BLa produced at the same exercise protocol and intensity. In other words, it would indicate an increase in lactate-buffering capacity and utilization. Although BLa levels varied in response to excess CO2, based on the confidence interval, the maximum variation was expected to be approximately 2 mmol/L. CO2 accumulation requires further calculations. The method used to calculate CO2 accumulation in previous studies was difficult to reproduce, and the coefficient was unknown [16,17]. However, this study used a mathematical method that maintains reproducibility and reiterates the relationship between ΔBLa and CO2 accumulation. When CO2 accumulation is high and ΔBLa is low, the skeletal muscle oxidative capacity is excellent (i.e., aerobic capacity is high). Thus, CO2 accumulation may be useful for assessing the oxidative capacity of skeletal muscles. Furthermore, excess CO2 can be calculated by simple subtraction alone, which may be useful for estimating BLa levels during Inc-Ex testing.
The results of this study reiterated the usefulness of ΔBLa and CO2 accumulation calculations and showed, for the first time, a relationship between simple excess CO2 and BLa during Inc-Ex. However, this study has some limitations. First, the relationship between excess CO2 and BLa levels is subject to a certain degree of variability. Thus, the BLa level can be roughly estimated from excess CO2. Second, the estimation of BLa from excess CO2 can only be ascribed to Inc-Ex testing combined with exhaled gas analysis. Therefore, the steady-state exercise loads and interval training exercise are unknown. Third, the Inc-Ex protocol in this study was a 10 W/min ramp exercise. Hence, it is unclear whether other exercise loading protocols yield results similar to that of this study. Finally, only the relationship between BLa and excess CO2 should be examined. Future studies should be conducted on the validity and reliability of excess CO2. In conclusion, excess CO2 during CPET correlated BLa meaningfully, and is useful for verifying BLa levels. Moreover, excess CO2 can be a good non-invasive marker for BLa.
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and approved by the Institutional Review Board of Sapporo Ryokuai Hospital (approval number: 19-1). Informed consent was obtained from all participants for participating in this study and publication of this report. The authors confirm that there is no identifying information of the participants in the manuscript and that the information has been fully anonymized. Furthermore, the authors affirmed that all mandatory health and safety procedures were observed while conducting the experimental work reported in this paper.
We would like to thank Editage for assistance in English language editing. The study results are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation, and the results of the present study do not constitute endorsement by the International Journal of Physical Medicine and Rehabilitation.
The dataset used in the current study is available from the corresponding author on request.
The study was conducted in accordance with the principles outlined in the Declaration of Helsinki and approved by the Institutional Review Board of Sapporo Ryokuai Hospital (approval number: 19-1). Informed consent was obtained from all participants for participating in this study and publication of this report. The authors confirm that there is no identifying information of the participants in the manuscript and that the information has been fully anonymized. Furthermore, the authors affirmed that all mandatory health and safety procedures were observed while conducting the experimental work reported in this paper.
This study did not receive any funding support. The authors declare no conflicts of interest.
Not applicable.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Citation: Kominami K, Akino M (2023) Verification of Blood Lactate during Incremental Exercise Testing. Int J Phys Med Rehabil. 11:655.
Received: 06-Dec-2022, Manuscript No. JPMR-22-20663; Editor assigned: 08-Dec-2022, Pre QC No. JPMR-22-20663 (PQ); Reviewed: 23-Dec-2022, QC No. JPMR-22-20663; Revised: 30-Dec-2022, Manuscript No. JPMR-22-20663 (R); Published: 09-Jan-2023 , DOI: 10.35248/2329-9096.23.11.655
Copyright: © 2023 Kominami K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.