Journal of Developing Drugs
Open Access
ISSN: 2329-6631
ISSN: 2329-6631
Research Article - (2022)Volume 11, Issue 4
Vesicular Drug Delivery System (VDDS) has been highly explored in the past couple of decades due to benefits such as increased patient compliance, improved drug release, tissue targeting, avoiding the pre-systemic metabolism in the liver etc. However, the stratum corneum poses as the rate limiting barrier to the permeation of drugs through the skin, which has been a continuous challenge in VDDS. This review covers the various types of nanoparticles and nanoemulsion that are currently being investigated for VDDS applications, desirable physical and chemical characteristics of these systems, their routes of penetration through the skin, and summarizes recent advances using these systems in treating conditions such as alopecia, wound healing, psoriasis, and melanoma. Additionally, synergistic effect of iontophoresis and mechanical force mediated drug delivery will be reviewed.
Transdermal drug delivery; Skin diseases; Vesicular systems
At present the most common form of drug delivery system is the oral route. The oral administration route is preferred over the various other administration routes of drug delivery due to the many advantages it exhibits. Due to its drawback like poor bioavailability, hepatic first pass metabolism and need of high or frequent dose there is need to develop a new drug delivery system to overcome this difficulty [1].
Vesicular drug delivery system is also a part of these novel drug delivery systems. Novel vesicular system aims to deliver the drug at predetermined rate as per the need of body during the treatment. In 1995 Bingham has reported the biological origin of these vesicles and named as Bingham bodies [2]. Vesicles have become the vehicle of choice in drug delivery system called vesicular drug delivery system, e.g. liposomes, noisome, pharmacosomes etc.
Today vesicular drug delivery system using colloidal particulate carrier have distinct advantages over conventional ones. Vesicular system in today’s era has changed the definition of diagnosis and treatment in different aspects of biomedical field. The vesicular systems are highly ordered assemblies of one or several lipid bilayers formed that are created when specific amphiphiles molecules. Vesicular system helps to control degradation of drugand loss prevention of harmful side effects and increases the availability of drug at site of disease. Vesicular drug encapsulation will extend the medicine's time in systemic circulation. Lipid vesicles are one type of experimental model of bio membrane which evolved successfully as vehicle for controlled delivery.
Anatomy of skin
Skin is the largest organ of human body and provides the highly differentiated interface of the body with the external environment, having multiple functionalities. Its functions include protection against injury, pathogens, allergens, etc., thermoregulation, acting as barrier to water loss, and serving as an excretory organ. Skin has a surface area of approximately 2 and comprises three basic layers: epidermis, dermis, and hypodermis. The epidermis is the outermost layer of skin; it is of ectodermal origin and is avascular. The thickness of the epidermis ranges from 50 µm to 1.5 mm. It is made up of stratified epithelial cells called corneocytes (keratinocytes). The four terminally differentiated layers of corneocytes are stratum germinativum, stratum spinosum, stratum granulosum and Sratum Corneum (SC). The innermost basal layer is the most active metabolically; it continuously divides [3]. The outermost SC is dense, keratinized, and dead, with a thickness of approximately 10-20 µm. The corneocytes in the SC have an organized intracellular matrix of keratin. Corneocytes are stacked like columns with intercellular spaces in a brick- and-mortar structure (Figure 1).
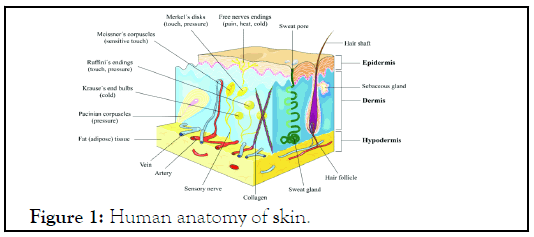
Figure 1: Human anatomy of skin.
Conventional treatment of skin diseases
The common medications for topical use include
Antibacterial: These medicines, like bactroban or cleocin, are often used to treat or prevent infection.
Anthralin (drithocreme, micanol and others: Although not often used, these help to reduce inflammation and can help treat psoriasis [4].
Antifungal agents: Lamisil, lotrimin and nizoral are few examples of common topical antifungal drugs used to treat skin conditions such as ringworm and athletes foot.
Benzoyl peroxide: Creams and other products containing benzoyl peroxide are used to treat acne. Coal tar-this topical treatment is available with and without a prescription, in strengths ranging from 0.5% to 5%. Coal tar is used to treat conditions including seborrheic dermatitis (usually in shampoos) or psoriasis. Currently, coal tar is seldom used because it can be slow acting and can cause severe staining of personal clothing and bedding [5].
Corticosteroids: These are used to treat skin conditions including eczema and come in many forms including foams, lotions, ointments and creams.
Retinoid: These medications (such as retin‑A and tazorac) are gels or creams derived from vitamin A and are used to treat conditions including acne.
Salicylic acid: This medication is available in the form of lotions, gels, soaps, shampoos and patches. It should be used sparingly applied to a particular place on or in the body at once can cause toxicity. Salicylic acid is the active ingredient in many skin care products for the treatment of acne and warts [6].
Oral treatments for skin conditions include
Antibiotics: Oral antibiotics like erythromycin, tetracycline and dicloxacillin are used to treat many skin conditions.
Antifungal agents: Common oral antifungal drugs such as ketoconaole and diflucan can be used to treat more severe fungal infections.
Antiviral agents: Common antiviral agents include valtrex, acyclovir and famavir. Antiviral treatments are used for skin conditions including those related to herpes [7].
Corticosteroids: These medications, including prednisone can be helpful in treating skin conditions linked to autoimmune diseases including vacuities and inflammatory diseases such as eczema and psoriasis. Dermatologists prefer topical steroids to avoid side‑effects; however, short‑term use of prednisone is sometimes necessary [8].
Immunosuppressants: Immunosuppressants, such as azathioprine and methotrexate, can be used to treat conditions including severe cases of psoriasis and eczema.
Biologics: These new therapies are the latest methods being utilized to treat psoriasis and other conditions. Examples of biologics include enbrel, humira, remicade, stelara and amevive.
Vesicular systems
Transferosomes: Transferosomes was introduced for effective transdermal delivery of number of low and high molecular weight drugs. Transferosomes can penetrate the intact stratum corneum spontaneously along two routes in the intracellular lipid that differ in their bilayer’s properties its penetration of intact vesicle. These vesicular transferosomes are several orders of magnitude more elastic then the standard leptosomes and thus well suited for the skin penetration. Transferosomes overcome the skin penetration difficulty by squeezing themselves along the intracellular stealing lipid of the stratum corneum. There is provision for this because of the high vesicle’s deformability. The permits the entry due the mechanical stress of surrounding, in a self-adapting manner. Transfersomes' membrane flexibility is controlled by the necessary surface-active components and phospholipids being combined in the right proportions. Transferosomes based formulation of local anesthetics-lidocaine and tetracaine showed permeation equivalent to subcutaneous injection [9]. Anticancer drugs like methotrexate were tried for transdermal delivery using transferosomes technology. This provided a new approach for treatment especially of skin cancer (Figure 2).
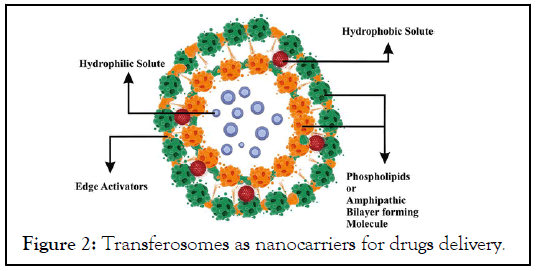
Figure 2: Transferosomes as nanocarriers for drugs delivery.
Mechanism of action
The present investigation indicates that the transferosome’s are drug mover systems that can penetrate across intact skin. It is believed that the unimpeded passage of such carriers is based on two key factors- the high elasticity (deformability) of the vesicle bilayers and the reality of an osmotic gradient across the skin. Because of their high deformability, transferosome’s with the help of EAs generate a trans epidermal osmotic gradient; and further squeeze among the stratum corneum cells and carry drug across the whole skin [10]. The transpore hydrostatic force difference is liable for the penetration or passage of transferosome intact throughout the stratum corneum, i.e. the penetration of transferosome is an outcome of hydrotaxis and the permeation is governed by principles of electro mechanics when a transferosome reaches a pore, it is capable of changing its membrane work reversibly as an effect of its self-optimizing deformability [11]. To go throughout the pore, the mechanism of the transferosome liable for its deformability starts accumulating at the site of tension, whereas the less elastic mechanism experiences dilution, which significantly reduces the active rate of membrane deformation and allows the highly elastic particles to go throughout the pores. The passage of transferosomes through the skin and the epithelial obstacle is greatly prejudiced by the flexibility of their membrane, which can be achieved via a suitable ratio of surfactants [12]. The flexibility of the transfersomal membrane decreases the risk of complete vesicle rupture in the skin and permits the ultra- deformable transferosome to change their membrane composition locally and reversibly when they are pressed against or attracted into a narrow pore [13]. This dramatically lowers the energetic cost of membrane deformation and permits the resulting highly flexible particles first to enter and then to pass through the pores rapidly and efficiently [14].
Method of preparation
Rotary film evaporation method: This method is also known as the hand-shaking process, which was initially invented by Bangham in this process, the quantity needed of phospholipids and surfactants (as EAs) is essential to organize a thin film It is largely worn for the research of multilamellar vesicles. A solution of phospholipids and EAs is organized in a crude solvent such as a combination of chloroform and methanol. The prepared solution is transferred to a round-bottomed flask which is rotated at constant temperature (above the glass transition temperature of lipids) and reduced pressure [15]. A film of lipids and EA is formed on the walls of the flask. The twisted film is then hydrated using aqueous media containing drug. This causes lipids to swell and form bilayer vesicles [16]. Vesicles of desired size can be obtained by extrusion or by sonication of the superior vesicles.
Reverse-phase evaporation method: At this point, the scheme will alter to a viscous gel followed by the arrangement of vesicles [17]. The non-encapsulated material and residual solvents can be indifferentiable using dialysis or centrifugation in this method, lipids dissolved in organic solvents are collected in a round- bottomed flask. Aqueous media containing EAs is added under nitrogen purging. The drug can be added to the lipid or aqueous medium based on its solubility character [18]. The system formed is then sonicated, awaiting its conversion into a standardized dispersion, and should not separate for at least 30 min after sonication. The organic solvent is then removed under low pressure [19].
Vortexing sonication method: In the vertexing sonication method, mixed lipids (i.e. phosphatidylcholine, EA and the therapeutic agent) are blended in a phosphate buffer and vortexed to attain a milky suspension [20]. The suspension is sonication, followed by extrusion through polycarbonate membranes cationic transferosome have also been set by this method, which involves mixing cationic lipids, such as DOTMA, with PBS to attain a concentration of 1.0 mg/ml followed by a count of sodium deoxycholate. The blend is vortexed and sonication, followed by extrusion through a polycarbonate (100 nm) filter [21].
Ethanol injection method: In this process, the aqueous solution containing drug is heated with unremitting stirring at constant temperature. Ethanolic solution of phospholipids and EAs is injected into aqueous solution dropwise [22]. As the solution comes into contact with aqueous media the lipid molecules are precipitated and form bilayered structures. This process offers assorted advantages over other methods, which include simplicity, reproducibility, and scale-up [23].
Applications: Actinic Keratosis (AK) is an ordinary skin ailment caused by long-standing sun exposure, and classically forms on the face, neck, balding scalp, chest, shoulders, and the back of arms and hands of adults, 75% of all reported lesions existing on the head, neck, and forearms. Actinic keratosis is characterized by the shape of keratotic macules, papules, or plaques with superficial scales on a red base. Lesions are frequently asymptomatic, but they can be painful or itchy. Owing to the swelling nature of the condition, the occurrence of AK increases with age and is an ordinary condition in the adult populace aged over 50 years. Treatment of AK depends on the medical appearance of the lesions- it may be fought at exact lesions (lesion directed) or at numerous lesions over a large area (field directed), and occasionally both treatment approaches are used. Therapy options include cryosurgery, curettage, excision surgery, Photodynamic Therapy (PDT), and topical treatments (5-FU cream, diclofenac gel, imiquimod cream, and indenol mebutate gel).
Characterizations of transferosomes: The Morphological characterization of transferosome vesicle such as shape and surface feature were projected by Photomicroscope using a digital Labored camera in 40x resolution and Transmission Electron Microscopy using (TEM,) and photomicrograph was taken. Chemical characterization includes those studies which established the purity and potency of various transfersomal constitutions.
Determination of entrapment efficiency percentage: Transferosome entrapped curcumin was estimated by centrifugation method. The prepared transfersome were placed in centrifugation tube and centrifuged at 14000 rpm for 30 minutes. The supernatant (1 ml) was withdrawn and diluted with phosphate buffer (pH 7.4). The unentrapped curcumin was determined by UV spectrophotometer at 427.2 nm. The samples from the supernatant were diluted 100 times before going for absorbance measurement. The free curcumin in the supernatant gives us the total amount of unentrapped drug.
Vesicle size: Transferosomes up to 300 nm in diameter is capable of permeating stratum corneum. It is measured by zeta sizer vesicle shape will determine by transmission electron microscopy.
Zeta potential: Zeta potential of transferosomes formulation will determined using zeta sizer at 25ºC. Zeta potential is the measure of the magnitude of the electrostatic or charge repulsion or attraction between particles and, known to affect stability.
Ethosomes: “Ethosomes are ethanolic liposomes”. Ethosomes can be defined as noninvasive delivery carriers that enable drugs to reach deep into the skin layers and the systemic circulation. These are soft, malleable vesicles tailored for enhanced delivery of active agents. The vesicles have been well known for their importance in cellular communication and particle transportation for many years. Vesicles would also allow controlling the release rate of drug over an extended time, keeping the drug shielded from immune response or other removal systems and thus be able to release just the right amount of drug and keep that concentration constant for longer periods of time. One of the major advances in vesicle research was the finding of a vesicle derivative, known as an ethosomes. Ethosomes are the slight modification of well-established drug carrier liposome. Ethosomes are lipid vesicles containing phospholipids, alcohol (ethanol and isopropyl alcohol) in relatively high concentration and water. Ethosomes are soft vesicles made of phospholipids and ethanol (in higher quantity) and water. The size range of ethosomes may vary from tens of nanometers (nm) to microns (µ) ethosomes permeate through the skin layers more rapidly and possess significantly higher transdermal flux (Figure 3).
Figure 3: Ethosomes are phospholipid nanovesicles used for dermal and transdermal drug delivery.
Methods of preparation of ethosomes
Cold method: This is the most common method utilized for the preparation of ethosomal formulation. In this method phospholipid, drug and other lipid materials are dissolved in ethanol in a covered vessel at room temperature by vigorous stirring with the use of mixer. Propylene glycol or another polyol is added during stirring. This mixture is heated to 300°C in a water bath. The water heated to 300°C in a separate vessel is added to the mixture, which is then stirred for 5 min in a covered vessel. The vesicle size of ethosomal formulation can be decreased to desire extend using sonication or extrusion method. Finally, the formulation is stored under refrigeration.
Hot method: In this method phospholipid is dispersed in water by heating in a water bath at 400°C until a colloidal solution is obtained. In a separate vessel ethanol and propylene glycol are mixed and heated to 400°C. Once both mixtures reach 400°C, the organic phase is added to the aqueous one. The drug is dissolved in water or ethanol depending on its hydrophilic/ hydrophobic properties. The vesicle size of ethosomal formulation can be decreased to the desire extent using probe sonication or extrusion method.
Method of characterizations of ethosomal formulation
Vesicle shape: Visualization of ethosomes can be done using Transmission Electron Microscopy (TEM) and by Scanning Electron Microscopy (SEM). Visualization by electron microscopy reveals an ethosomal formulation exhibited vesicular structure 300-400 nm in diameter. The vesicles seem to be malleable as evident by their imperfect round shape. Vesicle size and zeta potential particle size and zeta potential can be determined by Dynamic Light Scattering (DLS) using a computerized inspection system and Photon Correlation Spectroscopy (PCS).
Drug entrapment: The entrapment efficiency of ethosomes can be measured by the ultracentrifugation technique.
Transition temperature: The transition temperature of the vesicular lipid systems can be determined by using differential scanning calorimetry.
Drug content: of the ethosomes can be determined using UV spectrophotometer. This can also be quantified by a modified high-performance liquid chromatographic method.
Surface tension measurement: The surface tension activity of drug in aqueous solution can be measured by the ring method in a du nouy ring tensiometer.
Stability studies: The stability of vesicles can be determined by assessing the size and structure of the vesicles over time. Mean size is measured by DLS and structure changes are observed by TEM.
Skin permeation studies: The ability of the ethosomal preparation to penetrate into the skin layers can be determined by using Confocal Laser Scanning Microscopy (CLSM) (Figure 4).
Figure 4: Nanocarrier system for transdermal drug delivery.
Applications of VDDS
Future prospective: It offers an attractive and non-invasive form of drug delivery due to
• The reduced risk of systemic toxicity
• Avoiding the first-pass effect of the GI tract
• Providing higher patient compliance
• Improved bioavailability
Aquasomes: Three layered self-assembly compositions with ceramics carbon nanocrystalline particulate core coated with, glassy cellobiose specific targeting and molecular shielding.
Cryptosmes: Lipid vesicles with a surface coat composed of pc and of suitable polyoxymethylene derivative of phosphotidyl ethanolamine. Capable of Ligand mediated drug targeting.
Discomes: Niosomes solubilized with non-ionic surfactant solutions (polyoxyethylene cetyl ether class). Show ligand mediated drug targeting.
Emulsomes: Nanosize Lipid particles (bioadhesives nanoemulsion) consisted of microscopic lipid assembly with a polar core used parenteral delivery of poor water-soluble drugs.
Enzymosomes: Liposomal constructs engineered to provide a mini bioenvironmental in which enzymes are covalently immobilized or coupled to the surface of liposomes targeted delivery to tumor cell.
Genosomes: Artificial macromolecular complexes for functional gene transfer. Cationic lipids are most suitable because they possess high biodegradability and stability in the blood stream cell specific gene transfer.
Photosomes: Photolysis encapsulated in liposomes, which release the content photo triggered charges in membrane permeability characteristics.
Virosomes: Liposomes spiked with virus glycoprotein, incorporated into the liposomal bilayers based on retro viruses’ derived lipids.
Vesosomes: Nested bilayer compartment in vitro via the inter digested bilayer phase formed by adding ethanol to a variety of saturated phospholipids. Multiple compartments of the vesosomes give better protection to the interior contents in serum.
Proteosomes: High molecular weight multi-submit enzyme complexes with catalytic activity, which is specifically due to the assembly pattern of enzymes, better catalytic activity turn over than the non-associated enzymes.
Emulsomes: Hb containing liposome engineered by immobilizing Hb with polymerizable phospholipids.
Erythrosomes: Liposomal system in which chemically cross- linked human erythrocytes used as support to which lipid bilayer is coated.
Enzymosomes: Enzymes are co-valently immobilized or coupled to the surface of liposomes.Limitations
• The impervious nature of the SC that limits the types of drugs that can enter into the skin.
• The possibility of local irritation induced at the site of application. Nanoparticles have remarkable potential to act as drug carriers and transport them across the skin barrier.
Future developments of TDDSs will likely focus on the increased control of therapeutic regimens and the continuing expansion of drugs available for use. Transdermal dosage forms may provide clinicians an opportunity to offer more therapeutic options to their patients to optimize their care (Table 1).
| Nano-carriers | Characteristics | Advantages | Disadvantages |
|---|---|---|---|
| Liposomes | Hollow lipid bilayer sphere - composed of phospholipids and cholesterol | Can encapsulate both hydrophobic and hydrophilic drug molecules - biodegradable and non-toxic | Large size Small size |
| Transfersomes | Aqueous core surrounded by lipid bilayer with edge activator-used for transdermal deliver | Highly elastic deformable | Hydrophobic drug loading is challenging - transport of particle challenging during occlusive conditions. |
| Ethosomes | Composed of phosphatidylcholine, cholesterol, ethanol, and water-carriers can reach deep within the skin and systemic circulation | Can carry both hydrophilic or lipophilic drugs -can deliver under occlusive and nonocclusive conditions | Long term effects yet to be evaluated |
| Niosomes | Single or multilamellar composed of nonionic surfactants, and cholesterol | Economical to manufacture - superior stability -can make the SC looser and easier to penetrate the skin | |
| Solid lipid nanoparticles | Composed of solid lipids - used extensively for topical applications | Lipophilic drugs can be incorporated in matrix - high flexibility | Poor drug loading capacity - drug discharge during storage |
| Nanostructured lipid carriers | Composed of a mixture of solid and liquid lipids - used for topical applications | Increased drug loading compared to SLN - decreased drug discharge | Long-term physical stability data not available |
| Synthetic NP | Particles typically accumulate in hair follicles -drugs can be adsorbed on NP surface, encapsulated, or dispersed in matrix | Well defined propertied and characteristics | Typically used to deliver small lipophilic drugs (dendrimers can encapsulate both types) -controlled drug release is a challenge in dendrimers |
| Metallic NP | Rigid particles - used in topical administration | Can be fabricated into a wide range of sizes |
Table 1: Nano-carriers characteristics, advantages and disadvantages.
Skin disease: Skin disease here refers to disorders of exclusively (or predominantly) the superficial layers of the skin. Diseases with occasional or accessory skin features-such as leprosy, endemic treponematoses, or different varieties of filariasis, measles, chickenpox, and dengue fever. Deep skin and soft tissue infections (e.g. erysipelas, cellulitis and abscess) are not considered although they may be cited in the context of, for example, complications of superficial infections. This applies also to burns and traumatic sores. Common disorders refer to diseases that occur frequently in the general population (with a prevalence of >1%), or at a primary or peripheral healthcare level. This pragmatic definition is further explained below. Since disorders that are uncommon in some areas may be common in others, geographic specificities, as well as some constant features, should be indicated. Certain disorders-e.g. leishmaniasis, mycetomas, and infection due to Mycobacterium ulcerans are excluded although their frequency may sometimes reach a significant level; in addition, their management is very specific to each condition.
The main disorders that are considered here belong to one of the following categories-
Pyoderma: means any skin disease that is pyogenic (has pus). These include superficial bacterial infections such as impetigo, impetigo contagiosa, ecthyma, folliculitis, bockhart's impetigo, furuncle, carbuncle, tropical ulcer, Treatment of pyoderma gangrenosum is aimed at reducing inflammation, controlling pain, promoting wound healing and controlling any underlying disease. Treatment will depend on several factors, including health and the number, size, depth and growth rate of skin ulcers (Figure 5).
Figure 5: Polyderma used to treat for bacterial infections.
Scabies is a skin infestation caused by a mite known as the Sarcoptes scabiei. Untreated, these microscopic mites can live on your skin for months. They reproduce on the surface of your skin and then burrow into it and lay eggs. This causes an itchy, red rash to form on the skin. The hallmark symptoms of scabies include a rash and intense itching that gets worse at night. Continuous scratching of the infected area can create sores that become infected. Treatment for scabies usually involves getting rid of the infestation with prescription ointments, creams, and lotions that can be applied directly to the skin. Oral medications are also available (Figure 6).
Figure 6: Microscopic scabies in humans.
Tinea capitis is the name used for infection of the scalp with a dermatophyte fungus. Although common in children, tinea capitis is less frequently seen in adults. It gets the name ringworm because the fungus makes circular marks on the skin, often with flat centers and raised borders. Also called tinea capitis, this infection affects your scalp and hair shafts, causing small patches of itchy, scaly skin. Fungi called dermatophytes cause ringworm of the scalp. The most common symptom of ringworm is itchy patches on the scalp. The leading antifungal medications for ringworm are griseofulvin (Grifulvin V, GrisPEG) and terbinafine hydrochloride (Figure 7).
Figure 7: Tinea capitis in children.
Eczema is a condition where patches of skin become inflamed, itchy, red, cracked, and rough. Blisters may sometimes occur. The word "eczema" is also used specifically to talk about atopic dermatitis, the most common type of eczema. Atopic" refers to a collection of diseases involving the immune system, including atopic dermatitis, asthma, and hay fever. Dermatitis is an inflammation of the skin. Atopic dermatitis commonly occurs in infants, with dry and scaly patches appearing on the skin. These patches are often intensely itchy. Treatment for the condition aims to heal the affected skin and prevent flare-ups of symptoms (Figure 8).
Figure 8: Eczema: Atopic dermatitis.
Proriasis is a chronic skin condition caused by an overactive immune system. Symptoms include flaking, inflammation, and thick, white, silvery, or red patches of skin. Psoriasis treatments include steroid creams, occlusion, light therapy and oral medications, such as biologics. The 5 most common symptoms of psoriasis include Rashes or patches of red, inflamed skin, often covered with loose, silver-colored scales. In severe cases, the plaques will grow and merge into one another, covering large areas (Figure 9).
Figure 9: Psoriasis is a skin disease.
Melanoma: Melanoma is a form of skin cancer that arises when pigment-producing cells known as melanocytesmutate and become cancerous. Most pigment cells are found in the skin, but melanoma can also occur in the eyes ocular melanoma and other parts of the body, including, rarely, the intestines. It is rare in people with darker skin. Melanoma is just one type of skin cancer. It is less common than basal cell and squamous cell skin cancers, but it can be dangerous because it is more likely to spread, or metastasize. Melanomas can develop anywhere on the skin, but certain areas are more prone than others. In men, it is most likely to affect the chest and the back. In women, the legs are the most common site. Other common sites are the neck and face. According to the National Cancer Institute, about 87,110 new melanomas were expected to be diagnosed in 2017, and about 9,730 people were expected to die of melanoma (Figure 10).
Figure 10: Melanoma symptoms and cause.
Actinic keratosis: Typically occur on the face, lips, ears, bald scalp, shoulders, neck and back of the hands and forearms. Ranging in size from a tiny spot to as much as an inch in diameter, AKs usually appear as small crusty or scaly bumps or “horns.” The base can be dark or light skin-colored and may have additional colors such as tan, pink and red. Symptoms of actinic cheilitis, a variant of AK that appears on the lower lip, may include chapping, cracks and whitish discoloration.
Examples of typical actinic keratosis are shown here, so examine your skin regularly for lesions that look like them. But it’s not always that simple many actinic keratosis have quite a different appearance, so if you find any unusual or changing growth, be suspicious and see your doctor promptly.
Dermatological treatments are largely divided into external application of drugs, systemic therapies (oral administration of drugs, injections), physical therapies, laser therapies and surgical therapies. Among these treatments, topical therapies are the most important treatments in dermatology. Physical therapies, including irradiation and warming/cooling of affected sites, are also frequently applied. It is essential for dermatologists to have full knowledge of various therapies and combinations of effective treatments (Figure 11).
Figure 11: Actinic keratosis.
Acne: Acne is a disorder resulting from the action of hormones on the skin's oil glands (sebaceous glands), which leads to plugged pores and outbreaks of lesions commonly called pimples or zits. Acne lesions usually occur on the face, neck, back, chest, and shoulders. Nearly 17 million people in the United States have acne, making it the most common skin disease. Although acne is not a serious health threat, severe acne can lead to disfiguring, permanent scarring, which can be upsetting to people who are affected by the disorder. Symptoms can include pimples, pustules whiteheads, blackheads, cysts (Figure 12).
Figure 12: Acen that effect in teenagers.
Dermatitis: Dermatitis is a general term that describes an inflammation of the skin. Dermatitis can have many causes and occurs in many forms. It usually involves an itchy rash on swollen, reddened skin.
Skin affected by dermatitis may blister, ooze, develop a crust or flake off. Examples of dermatitis include atopic dermatitis (eczema), dandruff and rashes caused by contact with any of a number of substances, such as poison ivy, soaps and jewelry with nickel in it.
Dermatitis is a common condition that's not contagious, but it can make you feel uncomfortable and self-conscious. A combination of self-care steps and medications can help you treat dermatitis (Figure 13).
Figure 13: Dearmatitis is inflammation of the skin.
Herbs used in skin treatment
Natural drugs from the plants are gaining popularity because of several advantages such as often having fewer side‑effects, better patient tolerance, being relatively less expensive and acceptable due to a long history of use. Besides herbal medicines provide rational means for the treatment of many diseases that are obstinate and incurable in other systems of medicine. For these reasons several plants have been investigated for treatment of skin diseases ranging from itching to skin cancer. So far 31 plants have been reported to be effective in various skin diseases during the past 17 years (1995‑2012) of research work, which are mentioned below.
Achyranthes aspera (Common name: Prickly chaff flower, Devil’s horsewhip; Family: Amaranthaceae): Traditionally, the plant is used in boils, scabies and eruptions of skin and other skin diseases. The MeOH extract, alkaloid, non-alkaloid and saponin fractions obtained from the leaves of A. aspera exhibited significant inhibitory effects (concentration 100 µg) on the Epstein-Barrvirus Early Antigen (EBV-EA) activation induced by the tumor promotor 12-O- tetradecanoylphorbol-13-acetate in raji cells. In this in vitro assay t he non-alkaloid fraction containing mainly non-polar compounds showed the most significant inhibitory activity (96.9%; 60% viability). In the in vivo two-stage mouse skin carcinogenesis test the total methanolic extract possessed a pronounced ant carcinogenic effect (76%). The results revealed that leaf extract and the non-alkaloid fraction are valuable antitumor promotors in carcinogenesis.
Allium cepa (Common name: Onion; Family: Liliacea): A study undertaken in patients with seborrheic keratoses to evaluate the ability of onion extract gel to improve the appearance of scars following excision, has shown that this extract gel improved scar softness, redness, texture and global appearance at the excision site at study weeks 4, 6 and 10 as assessed by the blinded investigator. In another study, the antifungal activity of aqueous extracts prepared from A. cepa (onion; AOE) and Allium sativum (garlic; AGE) were evaluated against Malassezia furfur (25 strains), Candida albicans (18 strains), other Candida sp. (12 strains) as well as 35 strains of various dermatophyte species. The results indicated that onion and garlic might be promising in treatment of fungal‑associated diseases from important pathogenic genera like candida, Malassezia and the dermatophytes.A. sativum (Common name: Garlic; Family: Liliaceae): In a study conducted on swiss albino mice in whom cancer was induced by 7,12‑dimethylbenz(a)anthracene (DMBA) revealed that best chemo preventive action of garlic was observed in mice in which garlic treatment was performed before and after the induction of skin carcinogenesis. Garlic ingestion delayed formation of skin papillomas in animals and simultaneously decreased the size and number of papillomas, which was also reflected in the skin histology of the treated mice. The protective effect against skin cancer elicited by garlic in mice is believed to be due at least in part to the induction of cellular defense systems.
Aloe vera (Common name: Barbados aloe; Family: Xanthorrhoeaceae): Aloe vera has shown very good results in skin diseases and it is often taken as health drink. It is also found effective in treating wrinkles, stretch marks and pigmentations. It also seems to be able to speed wound healing by improving blood circulation through the area and preventing cell death around a wound. One of the studies conducted on mice to investigate the effects of Scutellariae radix and Aloe vera gel (AV), in spontaneous Atopic Dermatitis (AD)‑like skin lesions revealed that the group receiving only AV in a dose of 0.8 mg/ kg provided relief in AD due to reduction of interleukin (IL)‑5 and IL‑10 levels.
The gel has properties that are harmful to certain types of bacteria and fungi. A cream containing 0.5% aloe for 4 weeks reduced the skin “plaques” associated with psoriasis. Application of gel helped in the improvement of partial thickness burns. When applied to the skin, the gel seems to help skin survive frostbite injury. It might delay the appearance of skin damage during and after radiation treatment.
Azadirachta indica (Common name: Neem; Family: Meliaceae): Leaf extract is applied externally on boils and blisters. In one study, skin tumors were induced in mice by topical application of DMBA (500 nmol/100 µl for 2 weeks) followed by TPA (1.7 nmol/100 µl of acetone, twice weekly) as a promoter. The test group received aqueous Azadirachta Indica Leaf Extract (AAILE) orally at a dose level of 300 mg/kg body weight three times a week for 20 weeks. The results of this study revealed the chemopreventive potential of A. indica against murine skin carcinogenesis. Skin tumors obtained in the DMBA/TPA group exhibited enhanced expression of Proliferating Cell Nuclear Antigen (PCNA, index of proliferation), p21 and cyclin D1, with no alterations in p53 expression in comparison to the control group. Tumors in AAILE+DMBA/ TPA group exhibited low to PCNA and cyclin D1 expression and enhanced expression of p53 and p21 in comparison to the DMBA/TPA group. The skin tumors obtained in the AAILE+DMBA/TPA group exhibited to the high lipid peroxidation levels in comparison to the tumors obtained in the DMBA/TPA group. The observations of the study suggested that AAILE behaves as a pro‑oxidant in the tumors, thereby rendering them susceptible to damage, which eventually culminates into its anti‑neoplastic action. Also, cell cycle regulatory proteins may be modulated by AAILE and could affect the progression of cells through the cell cycle.
Bauhinia variegata (common name: kachanar, orchid tree, camel’s foot tree, mountain ebony; Family: Fabaceae): The bark is internally administered for treating skin diseases, asthma, sore throat, diarrhea and abdominal discomfort and also applied externally for skin ulcers. In the skin papilloma model, significant prevention, with delayed appearance and reduction in the cumulative number of papillomas was observed in the DMBA+Kachanar+croton oil treated group as compared to the DMBA+croton oil group. C57 Bl mice which received a 50% methanolic extract of kachanar extract at the doses of 500 and 1000 mg/kg body weight for 30 days showed increase in life span and tumor size was significantly reduced as compared to controls. In anti‑mutagenic studies, a single application of kachanar extract at doses of 300, 600 and 900 mg/kg dry weight, 24 h prior the i.p. administration of cyclophosphamide (at 50 mg/kg) significantly prevented micronucleus formation and chromosomal aberrations in bone marrow cells of mice, in a dose dependent manner.
Beta vulgaris (Common name: Beetroot; Family: Brassicaceae): The in vitro inhibitory effect of beet root extract on EBV‑EA induction using raji cells revealed a high order of activity compared to capsanthin, cranberry, red onion skin and short and long red bell peppers. An in vivo anti‑tumor promoting activity evaluation against the mice skin and lung bioassays also revealed a significant tumor inhibitory effect. The combined findings suggest that beet‑root ingestion can be one of the useful means to prevent cancer.
Brassica oleraceae (Common name: Red Cabbage; Family: Brassicaceae): Significant reduction of tumors was observed in mice in whom skin cancer was induced by a single topical application of 200 nmol of the initiator DMBA to their backs, followed 1 week later by promotion with 10 nmol of TPA twice weekly for 30 weeks followed by 0.1 g/L of aqueous extract of B. oleraceae 1 week after administration of initiator.
Calendula officinalis (Common name: Marigold; Family: Asteraceae): The flowers of marigold have long been employed in folk therapy and more than 35 properties have been attributed to decoctions and tinctures from the flowers. The main uses are as remedies for burns (including sunburns), bruises and cutaneous and internal inflammatory diseases of several origins. Topical formulations containing Marigold Extract (ME), evaluated in hairless mice against UV-B irradiation-induced photo damage, revealed that application of ME in gel formulation, containing 0.21 µg/cm of narcissin and as 0.07 µg/cm of the rutin in the viable epidermis, were associated with a possible improvement in the collagen synthesis in the sub epidermal connective tissue. One of the experiments carried out in 34 patients with venous leg ulcers to determine the therapeutic efficacy of ME on the epithelialization of lower leg venous ulcers revealed significant acceleration of wound healing by producing epithelialization. Research conducted on cream preparations containing seven different types of marigold and rosemary extracts, revealed that such creams are effective in experimentally induced irritant contact dermatitis when tested on healthy human volunteers.
Camellia sinensis (Common name: Green tea, Chaay; Family: Theaceae): Green tea comes from the tea plant C. sinensis and may play a beneficial role in treatment of skin tumors and cancer. It contains polyphenols, which act as antioxidants in the body. A specific polyphenol in green tea called epigallocatechin gallate, according to the National Center for Complementary and Alternative Medicine, has been reported to prevent the onset of further growth of skin tumor in the body. It can rejuvenate old skin cells to start reproducing again, keeping the skin younger looking.
Cannabis sativus (Common name: Charas, Ganja; Family: Cannabinaceae): The powder of the leaves serves as a dressing for wounds and sores. Ganja is externally applied to relieve pain in itchy skin diseases. Hemp seed oil is useful for treatment of eczema and host of other skin diseases like dermatitis, seborrheic dermatitis/cradle cap, varicose eczema, psoriasis, lichen planus and acne roseacea. By using hemp seed oil, the skin is strengthened and made better able to resist bacterial, viral and fungal infections. Crushed leaves are rubbed on the affected areas to control scabies.
Crocus sativus (Common name: Saffron; Family: Iridaceae): Saffron is a naturally derived plant product that acts as an antispasmodic, diaphoretic, carminative, emmenagogic and sedative. The chemopreventive effect of aqueous saffron on chemically induced skin carcinogenesis using a histopathological approach was studied. Its ingestion inhibited the formation of skin papillomas in animals and simultaneously reduced their size. Saffron inhibited DMBA‑induced skin carcinoma in mice when treated early. This may be due, at least in part, to the induction of cellular defense systems. It has also been found useful in treatment of psoriasis.
Curcuma longa (Common name: Turmeric; Family: Zingiberaceae): A study conducted on male Swiss albino mice in whom skin cancer was induced by topical application of DMBA, revealed a significant reduction in number of tumors per mouse in the group receiving 1% curcumin obtained from rhizomes of C. longa.
Daucus carota (Common name: Carrot; Family: Apiaceae): A study, conducted to investigate the chemopreventive effects of oil extract of D. carota umbels on DMBA‑induced skin cancer in mice for 20 weeks, revealed significant reduction in tumor incidence following administration via intraperitonial (0.3 ml of 2% oil) and topical (0.2 ml of 5, 50 and 100% oil) but least with gavage (0.02 ml of 100% oil).
Echinacea angustifolia, Echinacea purpurea (Common name: Purple cone flower; Family: Asteraceae): Echinacea has been applied to and used to treat skin problems such as skin boils, wounds, ulcers, burns, herpes, hemorrhoids and psoriasis. Forms of Echinacea include tablets, juice and tea. A study conducted on patients to determine the effect of oral supplementation with a nutraceutical, containing methionine, Echinacea, zinc, probiotics and other antioxidant and immunostimulating compounds, on the response of cutaneous warts revealed a significant reduction of warts in such patients.
The herbal extract of E. purpurea (Echinaforce®), readily killed a standard laboratory strain of Propionibacterium acnes (main cause of acne) and several clinical isolates. In cell culture models of human bronchial epithelial cells and skin fibroblasts, P. acne induced the secretion of substantial amounts of several pro‑inflammatory cytokines, including IL‑6 and IL‑8 (CXCL8), as determined by means of cytokine‑antibody arrays. However, the E. purpurea completely reversed this effect and brought the cytokine levels back to normal. Thus Echinaforce® could provide a safe two‑fold benefit to acne individuals by inhibiting proliferation of the organism and reversing the bacterial-induced inflammation.
Eucalyptus globulus (Common name: Blue gum, Camphor oil; Family: Myrtaceae): In a study conducted on humans it was revealed that human facial demodicidosis when treated with freshly prepared camphor oil with or without glycerol dilutions gave complete cure with concentrations of 100%, 75% and 50%respectively. Study conducted on humans revealed that camphor oil with or without glycerol dilutions completely cured zoonotic scabies with concentrations of 100%, 75% and 50% within 5‑10 days.
![]() Euphorbia walachii, Euphorbia hirta, Euphorbia tirucalli (Common name: Wallich spurge; Family. Euphorbiaceae): Juice of E. walachii is used to treat warts and skin infections. A study, conducted on various species of Euphorbia, E. hirta, exhibited best antioxidant activity. The plant extracts showed more activity against gram‑positive bacteria and fungi. The best antimicrobial activity was shown by E. tirucalli. The study supported the folkloric use of E. hirta and E. tirucalli against some skin diseases caused by oxidative stress or by microorganisms.
Euphorbia walachii, Euphorbia hirta, Euphorbia tirucalli (Common name: Wallich spurge; Family. Euphorbiaceae): Juice of E. walachii is used to treat warts and skin infections. A study, conducted on various species of Euphorbia, E. hirta, exhibited best antioxidant activity. The plant extracts showed more activity against gram‑positive bacteria and fungi. The best antimicrobial activity was shown by E. tirucalli. The study supported the folkloric use of E. hirta and E. tirucalli against some skin diseases caused by oxidative stress or by microorganisms.
Ficus carica, Ficus racemosa, Ficus bengaalensis (Common name: Fig; Family: Moraceae): In some rural areas of Iran, a traditional method for the treatment of warts comprises the use of fig tree (F. carica) latex. A study conducted in patients with warts has revealed that this therapy of warts offers several beneficial effects including short‑duration therapy, no reports of any side‑effects, ease‑of‑use, patient compliance and a low recurrence rate. Although, exact mechanism of the antiwart activity of fig tree latex is unclear it is likely to be the result of the proteolytic activity of the latex enzymes. F. recemosa L. bark powder is used externally in case of pimples, itches and scabies and F. bengaalensis L. bark powder is also used externally to cure scabies.
Lavendula officinalis (Common name: Lavender; Family: Labiatae): The effects of lavender oil (1:500, 1:100, 1:10, 1:1, 1:0) on mast cell‑mediated immediate‑type allergic reactions in mice and rats have been studied. It has been reported to inhibit concentration‑dependently the histamine release from the peritoneal mast cells. It also inhibits immediate‑type allergic reactions by inhibition of mast cell degranulation in vivo and in vitro when tested on mice and rats.
Lawsonia inermis (Common name: Henna; Family: Lythraceae): Henna is a traditionally used plant of Middle-East that is applied on hands and feet. In the traditional system of medicine, leafpaste is applied twice a day, on the affected parts to cure impetigo.
In a study, clinical improvement in the patients suffering from hand and foot disease due to use of capecitabine, an anti-cancer drug, with use of henna revealed anti-inflammatory, antipyretic and analgesic effects of henna (Table 2).
| S.No. | Plant | Part used | Family | Disease |
|---|---|---|---|---|
| 1 | Achyranthes aspera | Flower | Amaranthaceae | Boils, scabies and eruptions of skin |
| 2 | Allium cepa | Gel extract | Liliaceae | Scar softness, redness, texture, antifungal |
| 3 | Allium sativum | Gel extract | Liliaceae | Skin carcinogenesis |
| 4 | Aloe vera | Pulp | Xanthorrhoeaceae | Wrinkles, stretch marks and pigmentations |
| 5 | Azadirachta indica | Leaves | Meliaceae | Skin tumors |
| 6 | Beta vulgaris | Fruit | Brassicaceae | Anti‑tumor |
| 7 | Calendula officinalis | Flower | Brassicaceae | Burns (including sunburns), bruises and cutaneous and internal inflammatory diseases |
| 8 | Camellia sinensis | Leaves | Asteraceae | Skin tumors and cancer |
| 9 | Cannabis sativus | Leaves | Cannabinaceae | Dermatitis, seborrheic dermatitis/cradle cap, varicose eczema, psoriasis, lichen planus and acne roseacea |
| 10 | Crocus sativus | Wood | Iridaceae | antispasmodic, diaphoretic, carminative, Emmenagogic and sedative |
| 11 | Curcuma longa | Rhizomes | Zingiberaceae | Tumor and anti-inflammatory |
| 12 | Daucus carota | Root | Apiaceae | Chemopreventive |
| 13 | Echinacea angustifolia | Flower | Asteraceae | Skin boils, wounds, ulcers, burns, herpes, hemorrhoids and psoriasis |
| 14 | Eucalyptus globulus | Fruit | Myrtaceae | Facial demodicidosis |
| 15 | Ficus carica | Latex | Moraceae | Pimples, Itches and scabies |
Table 2: Medicinal plants are used for treatment of diseases.
Since 1981, transdermal drug delivery systems have been used as safe and effective drug delivery devices. Their potential role in controlled release is being globally exploited by the scientists with high rate of attainment. If a drug has right mix of physical chemistry and pharmacology, transdermal delivery is a remarkable effective route of administration. Due to large advantages of the VDDS, many new researches are going on in the present day to incorporate newer drugs via the system. Utilization and solving of critical issues of pharmaceutics field by outstanding examples of vesicular drug delivery system such as liposome, niosome etc. have been proved themselves as novel approach and very much useful as drug delivery system in current field and have remarkable place in pharmaceutical dosage forms over and above to the conventional drug delivery system.
[Crossref] [Google scholar] [Pubmed]
[Google scholar] [Pubmed]
[Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Crossref] [Google scholar] [Pubmed]
[Google scholar] [Pubmed]
Citation: Dwivedi D (2022) Vesicular Drug Delivery System for the Herbal Treatment of Skin Disease. J Develop Drugs.11:177.
Received: 04-Jul-2022, Manuscript No. EOED-22-003-PreQc-22; Editor assigned: 08-Jul-2022, Pre QC No. EOED-22-003-PreQc-22 (PQ); Reviewed: 22-Jul-2022, QC No. EOED-22-003-PreQc-22; Revised: 29-Jul-2022, Manuscript No. EOED-22-003-PreQc-22 (R); Published: 05-Aug-2022 , DOI: 10.35248/2329-6631.22.11.177
Copyright: © 2022 Dwivedi D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.